Imagine a condition that affects millions of people worldwide—yet remains shrouded in silence, misunderstood even by the medical community, and frequently dismissed as “just bad cramps.” That condition is endometriosis, a chronic, often excruciating disorder that impacts the lives of up to 1 in 10 people assigned female at birth during their reproductive years. But what exactly is it?
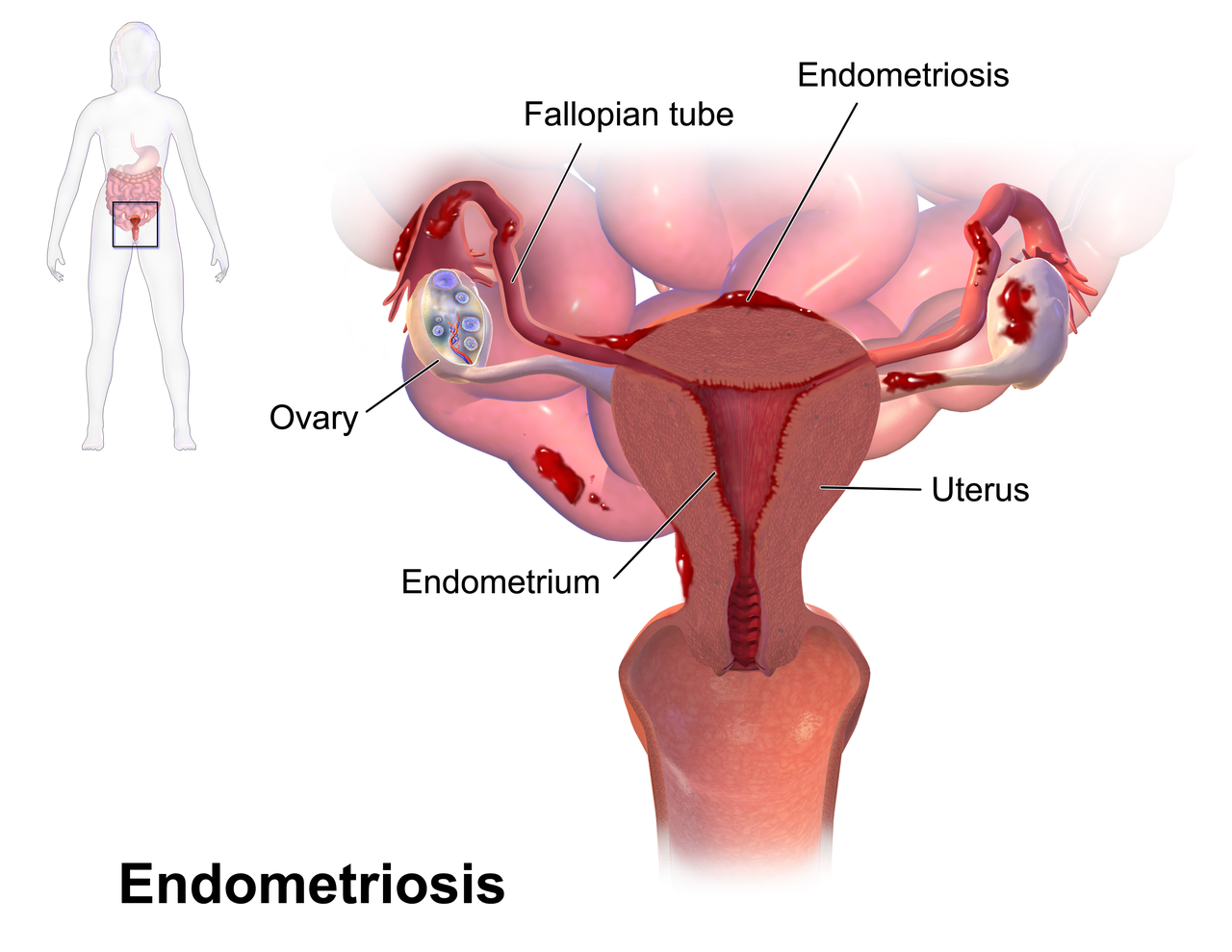
Endometriosis occurs when tissue similar—but not identical—to the endometrium, the lining of the uterus, begins to grow outside the uterus. This tissue might find a home on the ovaries, fallopian tubes, pelvic lining, or even the bladder and intestines. Despite being outside the uterus, it acts like endometrial tissue: it thickens, breaks down, and bleeds with each menstrual cycle. The problem is, there’s nowhere for this blood to go. This can lead to inflammation, scarring, cysts, and adhesions—bands of fibrous tissue that can bind organs together.
Unlike typical menstrual pain, the discomfort from endometriosis can be relentless, unpredictable, and all-consuming. But the pain is just one facet of the disease. Endometriosis can also lead to infertility, digestive and urinary issues, chronic fatigue, and a range of mental health challenges. It can upend careers, strain relationships, and erode quality of life.
Understanding endometriosis means recognizing it for what it is: not just a reproductive issue, but a full-body, systemic condition that demands serious attention, research, and empathy.
The Many Faces of Pain: Symptoms and How They Manifest
Endometriosis does not present the same way in every person. Its symptoms vary dramatically in intensity, timing, and nature. For some, it begins subtly, with periods that seem heavier or slightly more painful than usual. For others, it crashes in like a storm, bringing with it searing pelvic pain that makes walking, sitting, or even breathing feel like an ordeal.
The most common symptom is pelvic pain, especially during menstruation. But endometriosis pain often exceeds what most would consider “normal period cramps.” It can radiate to the lower back and thighs, resemble nerve pain or stabbing sensations, and persist throughout the entire menstrual cycle. Pain during sex—known as dyspareunia—is another hallmark. Some feel intense pain deep in the pelvis during intercourse, making intimacy a physically and emotionally distressing experience.
Other frequent symptoms include painful bowel movements or urination, especially during periods. Many experience bloating so intense that it’s been dubbed “endo belly”—a sensation of fullness or distention that can make someone look several months pregnant. Fertility struggles can also be a clue, especially in people who have tried unsuccessfully to conceive for over a year.
Fatigue is another common but under-discussed symptom. It’s not the kind of tiredness a nap can fix. It’s an all-encompassing, bone-deep exhaustion that interferes with work, hobbies, and day-to-day functioning.
For many, these symptoms are cyclical—waxing and waning with the menstrual cycle—but for others, they’re constant. This unpredictability can make diagnosis all the more difficult, contributing to the average diagnostic delay of 7 to 10 years.
The Diagnosis Dilemma: Why It Takes So Long to Get Answers
You might wonder how a condition so painful and pervasive could go undiagnosed for nearly a decade. The answer lies at the intersection of medical complexity, societal stigmas, and gender bias in healthcare.
For years, the medical community treated menstrual pain as something normal to endure rather than investigate. Patients who reported debilitating cramps were often dismissed with phrases like “it’s just part of being a woman” or “some people just have bad periods.” This normalization of suffering created an environment where endometriosis could hide in plain sight.
Compounding this problem is the fact that endometriosis can’t be definitively diagnosed through blood tests or imaging. While ultrasounds and MRIs can sometimes detect endometriomas (cysts associated with endometriosis), many lesions are invisible on scans. The gold standard for diagnosis remains laparoscopic surgery—a minimally invasive procedure where a surgeon inserts a camera into the abdomen to look for and biopsy suspicious tissue. But surgery is costly, carries risks, and isn’t accessible to everyone.
Moreover, endometriosis symptoms often overlap with those of other conditions like irritable bowel syndrome (IBS), interstitial cystitis, pelvic inflammatory disease, and even appendicitis. This overlap can send patients on a wild-goose chase, bouncing from one specialist to another while their condition worsens.
There’s also a broader cultural issue: many societies are uncomfortable talking openly about menstruation, pelvic pain, or reproductive health. This silence breeds ignorance and delays intervention. Only recently has the conversation started to shift, thanks to advocacy from patients, healthcare professionals, and public figures breaking the taboo.
Causes and Theories: What Triggers Endometriosis?
One of the enduring mysteries surrounding endometriosis is its origin. Scientists have proposed several theories, but no single explanation accounts for every case.
The most widely accepted theory is retrograde menstruation. This occurs when menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of exiting the body. This blood may contain endometrial cells, which can then implant and grow on pelvic organs. But retrograde menstruation happens in many people who never develop endometriosis, so this theory doesn’t hold all the answers.
Another hypothesis is coelomic metaplasia, which suggests that certain cells outside the uterus can transform into endometrial-like cells under specific conditions, possibly influenced by hormones or inflammation. There’s also a theory involving immune dysfunction—perhaps in some individuals, the immune system fails to clear away stray endometrial cells or allows them to flourish in the wrong places.
Genetic factors likely play a role, too. Endometriosis tends to run in families, and researchers have identified specific genes that might increase susceptibility. Environmental toxins such as dioxins have also been implicated, as they can disrupt hormonal balance and immune function.
Some scientists are exploring the possibility that endometriosis is not just a gynecological condition but an autoimmune or neuroinflammatory disease. This would help explain why it affects more than just the reproductive system and why symptoms like fatigue, brain fog, and widespread pain occur.
Despite years of research, we still don’t fully understand why endometriosis develops. What is clear is that it is not caused by lifestyle choices, psychological factors, or sexual activity—misconceptions that have long stigmatized sufferers.
Living with Endometriosis: Daily Challenges and Mental Health
To live with endometriosis is to become an expert in navigating pain. But the toll it takes goes beyond physical discomfort. The chronic nature of the disease, the uncertainty of flare-ups, and the emotional isolation it can bring all contribute to a deeply challenging reality.
For many, the unpredictability is the hardest part. One day might be manageable, the next unbearable. Plans get canceled, social lives shrink, and career ambitions may be altered or postponed. Chronic illness is exhausting in itself, but add the frustration of not being believed or understood, and the emotional weight becomes immense.
Depression and anxiety are common among people with endometriosis. The physical pain can lead to a sense of helplessness, while fertility issues can trigger profound grief. Intimacy problems might strain romantic relationships, and the ongoing need to advocate for one’s own care can be draining.
Financial stress adds another layer. Treatments are expensive. Surgical interventions are often not fully covered by insurance. And time off work can be frequent and unpaid, especially in countries without robust medical leave policies.
Yet despite these challenges, many individuals with endometriosis display extraordinary resilience. Online communities have become lifelines, offering validation, advice, and solidarity. Awareness campaigns are breaking the silence, and patients are becoming powerful advocates for change.
Treatment Options: Managing a Chronic Condition
There is currently no cure for endometriosis, but various treatments can help manage symptoms and improve quality of life. The right approach often depends on the severity of symptoms, the individual’s reproductive goals, and how the disease has progressed.
Pain relief is typically the first step. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help with mild to moderate discomfort. However, they’re often insufficient on their own.
Hormonal therapies are commonly used to suppress the menstrual cycle and reduce endometrial tissue growth. These include birth control pills, progestins, GnRH agonists and antagonists, and the hormonal IUD. While these can be effective for symptom control, they do not eliminate existing lesions and come with potential side effects like mood changes, bone loss, and decreased libido.
Surgical intervention remains a critical option, especially for those with moderate to severe endometriosis. Laparoscopic excision surgery, where the surgeon carefully removes endometrial lesions, is considered the gold standard. Some patients experience significant relief after surgery, although recurrence is possible.
In cases where the disease is extensive and all other options have failed, a hysterectomy (removal of the uterus) may be considered. However, this is not a guaranteed cure, especially if endometrial-like tissue remains outside the uterus.
Complementary and lifestyle approaches—such as pelvic floor physical therapy, dietary changes, acupuncture, and stress reduction techniques—can also make a difference. While these aren’t substitutes for medical treatment, they can be powerful tools in a holistic management plan.
The most important thing is individualized care. What works for one person may not work for another, and navigating treatment options often involves trial and error.
The Intersection with Fertility
Endometriosis and infertility are closely linked. It’s estimated that 30% to 50% of individuals with endometriosis have difficulty conceiving. This can be due to anatomical distortions from adhesions or cysts, inflammation that affects egg quality and sperm function, or disruptions in the hormonal environment necessary for implantation.
However, infertility with endometriosis is not inevitable. Many people with the condition go on to have successful pregnancies—sometimes naturally, sometimes with the help of assisted reproductive technologies like IVF.
Fertility treatments for endometriosis patients require careful coordination. Some benefit from surgical removal of lesions before trying to conceive. Others may move directly to IVF depending on the severity of the disease and age. The emotional aspect of infertility should not be underestimated, and psychological support is essential during this journey.
Advocacy, Awareness, and Hope for the Future
In recent years, the tide has begun to turn. Celebrities like Lena Dunham, Halsey, and Padma Lakshmi have spoken publicly about their struggles with endometriosis, bringing much-needed visibility to the condition. Social media platforms have given patients a voice, helping to push endometriosis into the spotlight.
Advocacy groups around the world are demanding more research funding, better medical education, and policies that support patients. March is now Endometriosis Awareness Month, and the color yellow has become a symbol of solidarity.
Researchers are exploring new frontiers, from genetic studies and biomarkers to better diagnostic tools and non-hormonal therapies. There’s hope that one day, diagnosing endometriosis won’t require surgery, and treatments will target the disease at its root rather than just its symptoms.
But even now, progress is being made—not just in science, but in how we talk about menstrual and pelvic health. The more we acknowledge the reality of conditions like endometriosis, the closer we come to a world where pain is not dismissed, silence is not the norm, and healing is truly possible.
Final Thoughts: Compassion, Clarity, and the Power of Listening
Endometriosis is more than a gynecological disease. It is a complex, chronic, and life-altering condition that touches every facet of a person’s existence—physical, emotional, relational, and economic. It teaches us not only about medical science but about the power of empathy, the dangers of dismissal, and the urgent need for systemic change.
For those living with endometriosis, your pain is real. Your voice matters. And your courage—often displayed in silence—is changing the world. For those learning about this condition for the first time, let this be the beginning of awareness, understanding, and advocacy.
Together, we can move from a world where endometriosis is misunderstood to one where it is recognized, respected, and, one day, perhaps even cured.