Cancer is not a single disease but a complex family of disorders with one common theme—cells that refuse to follow the rules. In the healthy body, cells live by a code of cooperation. They grow, divide, and die in regulated patterns that sustain the whole. Cancer arises when this cellular order breaks down. A normal cell becomes rebellious. It divides when it should rest. It resists death when it should self-destruct. It ignores the biochemical stop signs that preserve balance in tissues and organs. Slowly, insidiously, a malignant transformation unfolds.
But what triggers this defiance? Why does a healthy cell, one that may have functioned quietly for decades, suddenly shift into overdrive? The answer lies at the intersection of genes, the environment, the immune system, and time itself. Understanding what causes cancer means understanding how life can go awry at the most fundamental level—and how this knowledge is helping us fight back.
The Genetic Blueprint and Its Fragility
At the heart of every cell is a nucleus filled with DNA, a spiraling molecule that carries the instructions for life. These instructions are encoded in genes, which act like molecular recipes for building proteins. Proteins regulate everything from cell growth to metabolism to immune function. But like any blueprint, DNA is vulnerable to damage. Small errors in the genetic code—called mutations—can have outsized effects.
Most mutations are harmless. Some even do nothing at all. But certain mutations can disable the genes that restrain cell growth or activate those that encourage it. Over time, the accumulation of such mutations can push a cell toward malignancy.
Some of these mutations are inherited, passed from parent to child like a genetic fingerprint. Others are acquired, caused by environmental factors, infections, or random errors during cell division. It’s this dual nature of cancer—both genetic and environmental—that makes it so complex and so challenging to treat.
The Guardians of the Genome
Not all genes are created equal when it comes to cancer. Certain genes act as the body’s natural defense against tumors. Among the most famous is TP53, sometimes called the “guardian of the genome.” This gene produces a protein that can pause the cell cycle, trigger DNA repair, or instruct a damaged cell to self-destruct if repair fails.
When TP53 is mutated, cells can continue dividing even with damaged DNA. It’s no coincidence that TP53 is altered in more than half of all human cancers. Other key players include BRCA1 and BRCA2, genes that help repair double-strand DNA breaks. Inherited mutations in these genes dramatically increase the risk of breast and ovarian cancer.
These tumor suppressor genes operate like brakes on cell division. But cancers also exploit the gas pedals—genes known as oncogenes. When mutated or overactive, oncogenes drive cells to divide uncontrollably. One of the earliest discovered oncogenes, RAS, is implicated in lung, colon, and pancreatic cancers. The balance between these opposing genetic forces—brakes and accelerators—determines whether a cell stays in line or breaks free.
Mutations Through the Lens of Time
Cancer is fundamentally a disease of aging. Though it can strike at any age, the risk increases dramatically as we grow older. This is no accident. Our bodies are made of trillions of cells, and every day, billions of them divide. With each division, the machinery that copies DNA introduces small errors. Most are repaired. Some slip through.
Over decades, these minor mistakes accumulate like rust on a machine. It can take years—or even decades—for a cell to gather enough critical mutations to become cancerous. This is why childhood cancers, while tragic, are relatively rare compared to adult forms. In a young body, the genetic slate is cleaner. In the aged, time itself becomes a carcinogen.
But time is not the only culprit. Environmental exposures can accelerate the mutation rate, nudging cells down the path to malignancy faster and more forcefully.
The Environmental Spark That Lights the Fuse
The environment surrounding our bodies is a chemical soup, and not all of it is benign. Certain substances are known to be carcinogenic—that is, capable of causing cancer. Tobacco smoke is among the most notorious. Laden with over 70 known carcinogens, cigarette smoke damages the DNA in lung cells directly and overwhelms the body’s ability to repair that damage. It’s no coincidence that lung cancer is the leading cause of cancer death worldwide.
Ultraviolet radiation from sunlight is another potent carcinogen. It damages the DNA in skin cells, leading to mutations that drive melanoma and other skin cancers. The link between sun exposure and skin cancer is so strong that in many regions, rates of melanoma are rising in tandem with increased outdoor leisure activities.
Certain chemicals in industrial environments, such as asbestos, benzene, and formaldehyde, are also well-established causes of cancer. Asbestos fibers, once widely used in construction, can lodge in lung tissue and cause mesothelioma—a rare but deadly cancer. These examples underscore a sobering truth: many of the substances we encounter in daily life can subtly rewrite the scripts our cells live by.
The Role of Infections in Driving Malignancy
Not all causes of cancer are physical. Some are biological, stemming from infections that set off long-term changes in the body. Viruses are particularly insidious. The human papillomavirus (HPV), for instance, is the primary cause of cervical cancer. It infects the cells of the cervix and introduces its own DNA, disrupting normal cell function and promoting uncontrolled growth.
Hepatitis B and C viruses can lead to chronic liver inflammation, eventually triggering liver cancer. Epstein-Barr virus, better known for causing mononucleosis, is linked to several types of lymphoma. Even the stomach bacterium Helicobacter pylori, which can cause ulcers, has been implicated in stomach cancer.
In these cases, the infection itself is not the sole cause. Instead, the pathogen creates an environment—chronic inflammation, tissue damage, immune suppression—in which cancer is more likely to emerge. The link between infection and cancer reminds us that the immune system plays a crucial role in keeping our cellular society in check.
When the Immune System Falls Asleep
The immune system is not just a defense against pathogens—it is also a surveillance network, constantly patrolling the body for abnormal cells. This system can recognize and destroy cells that bear the hallmarks of early cancer. In fact, many precancerous cells are likely eliminated by the immune system before they ever pose a threat.
But cancer is clever. Some tumor cells learn how to hide. They may stop displaying the molecular markers that trigger an immune attack. Others release signals that suppress immune activity, effectively lulling the immune system into sleep. This ability to evade immune detection is now recognized as one of the hallmarks of cancer.
Immunodeficiency, whether caused by disease or treatment, increases cancer risk. People with HIV, for instance, are more prone to cancers like Kaposi sarcoma and certain lymphomas. Organ transplant recipients, who must take drugs to suppress their immune systems, also face higher rates of cancer. These patterns reveal the extent to which our immune defenses quietly prevent cancer every day.
The Tumor Microenvironment as a Breeding Ground
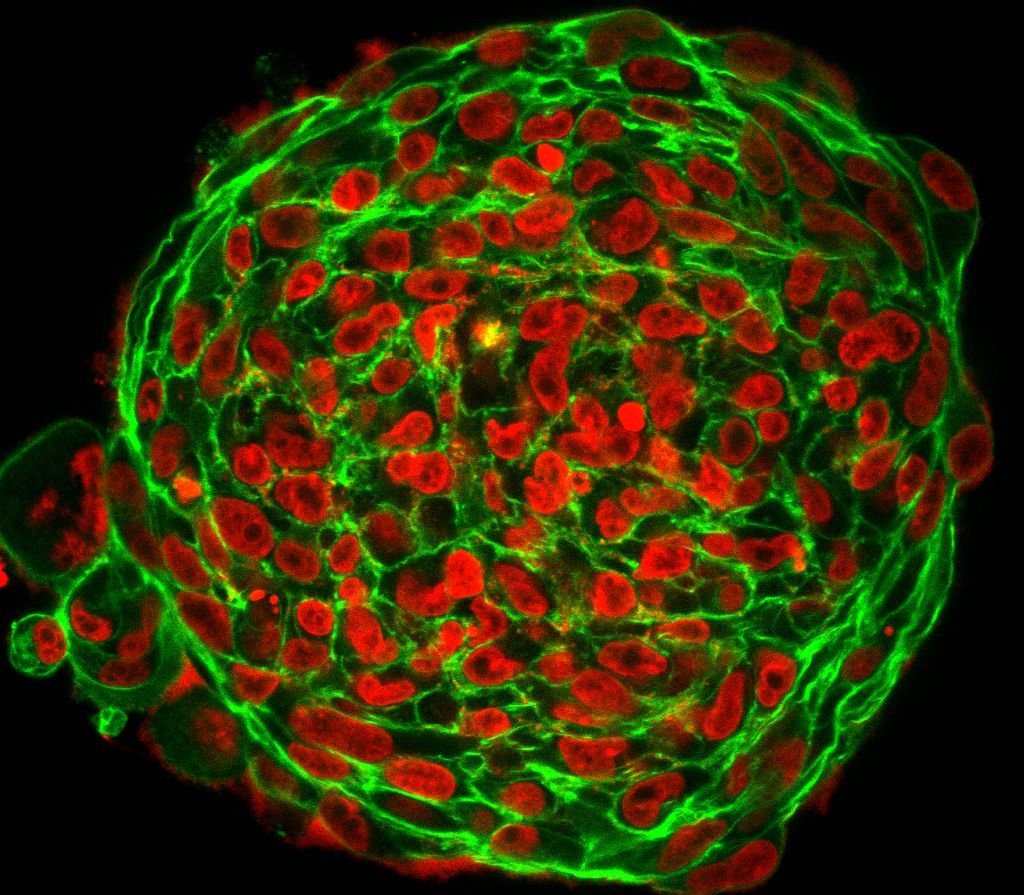
Cancer does not grow in isolation. It reshapes its environment to support its own survival. As tumor cells proliferate, they summon blood vessels to feed their expansion in a process called angiogenesis. They release growth factors that stimulate nearby stromal cells. They recruit immune cells—not to attack, but to assist, often converting them into allies that suppress the anti-cancer immune response.
This dynamic ecosystem, known as the tumor microenvironment, is essential to cancer progression. Within it, normal cells can be co-opted, signaling pathways hijacked, and defenses dismantled. It is not only the cancer cell’s mutations that matter, but the context in which those mutations operate. A cell with harmful mutations might die in a healthy environment—but thrive in a permissive one.
Researchers now recognize that disrupting the tumor microenvironment may be as important as targeting the cancer cells themselves. Therapies that block blood vessel formation or reawaken the immune system are reshaping the landscape of cancer treatment.
Lifestyle as a Modifier of Cancer Risk
While some risk factors lie beyond our control—such as inherited mutations or age—many others are shaped by lifestyle. Diet, exercise, alcohol consumption, and exposure to toxins can all influence the likelihood of cancer. Obesity, for example, is a significant risk factor for at least 13 types of cancer. Excess fat tissue produces hormones and inflammatory signals that can promote tumor growth.
A diet rich in fruits, vegetables, and fiber is associated with a lower risk of colorectal and other cancers, while excessive consumption of red and processed meats may increase risk. Alcohol acts as a solvent, making tissues more vulnerable to carcinogens, and its breakdown in the body produces acetaldehyde, a toxic compound that damages DNA.
Physical activity, on the other hand, is protective. Exercise reduces inflammation, improves hormone regulation, and enhances immune surveillance. These lifestyle factors don’t cause cancer directly, but they shape the terrain in which cancer may or may not take root.
Epigenetics as the Invisible Layer of Influence
Not all genetic changes involve mutations. There is another layer of control above the DNA sequence known as epigenetics. Epigenetic changes can turn genes on or off without altering the underlying code. They work through chemical tags—like methyl groups—that attach to DNA or its packaging proteins.
Environmental exposures, stress, diet, and aging can all influence epigenetic patterns. Some cancers arise not because genes are mutated, but because key tumor suppressor genes are epigenetically silenced. This reversible form of gene regulation offers a tantalizing target for therapies that might reawaken dormant genes and restore normal cellular behavior.
In this way, epigenetics forms a bridge between environment and genetics. It is the mechanism by which external experiences are written onto the genome without rewriting the code—a kind of molecular memory with the power to alter fate.
The Complexity of Risk and the Fallacy of One Cause
One of the most challenging truths about cancer is that it rarely has a single cause. Instead, it emerges from the interplay of many factors—genetic susceptibility, environmental exposure, immune competence, lifestyle choices, and random chance. A person may inherit a harmful mutation and never develop cancer. Another may live in a polluted environment and remain cancer-free.
This complexity can be frustrating, especially when we crave clear answers. But it also opens the door to personalized prevention and treatment. As we learn more about individual risk profiles—through genetic testing, biomarker analysis, and environmental monitoring—we can tailor interventions more precisely.
Rather than asking what causes cancer in general, science is shifting toward asking what causes cancer in this person, at this moment, in this tissue. It is a more nuanced question, and a far more powerful one.
The New Frontier in Understanding and Preventing Cancer
Modern cancer research is increasingly focused on prevention and early detection. By identifying high-risk individuals—those with inherited mutations like BRCA, or those exposed to known carcinogens—we can intervene earlier. Vaccines against cancer-causing viruses like HPV and hepatitis B are already preventing thousands of cases each year.
Advances in genetic screening are helping families understand their inherited risks, while liquid biopsies—blood tests that detect tumor DNA—promise earlier diagnosis. Lifestyle interventions remain one of the most potent tools we have: quitting smoking, reducing alcohol intake, maintaining a healthy weight, and staying physically active can collectively prevent millions of cancer cases worldwide.
The war on cancer is not a single battle. It is a long campaign across many fronts. But each discovery, each refined question, brings us closer to understanding the full story of what causes cancer.
Rewriting the Narrative of Cancer
Cancer is a word, not a sentence. Though its causes are diverse and complex, they are increasingly understood. From inherited mutations to environmental toxins, from viral infections to the slow creep of time, cancer arises when order gives way to chaos. But knowledge restores that order. It offers power—not only to treat cancer when it strikes, but to prevent it before it takes hold.
In the grand story of life, cancer is a rogue chapter. Our growing understanding of its causes is helping us rewrite the ending.