When most people hear the word chemotherapy, their minds flash to scenes from hospitals, bald heads, and intravenous drips. It’s a word heavy with emotion—fear, hope, resilience. But beneath its emotional weight lies a remarkable world of cellular warfare. Chemotherapy is not just a treatment; it’s a battleground strategy, forged at the microscopic level, where chemicals are unleashed to destroy one of biology’s most insidious mistakes—cancer.
To understand how chemotherapy works, we need to enter the living, breathing tissue of the human body. Here, in this bustling metropolis of cells, each cell has its job, its role, and most importantly, its place in the cycle of life. But cancer disrupts this balance. It’s a rebellion, a refusal to follow the rules, and chemotherapy is the counterstrike designed to stop this cellular anarchy.
Understanding the Enemy in Our Midst
Cancer is not a foreign invader like a virus or bacterium. It arises from our own cells, corrupted and out of control. Normally, cells divide in a tightly regulated process. When cells are damaged, they either repair themselves or die off. Cancer cells, however, ignore these rules. They divide relentlessly, hoarding resources, creating masses called tumors, and in some cases, spreading to distant organs in a process known as metastasis.
This unchecked growth is possible because cancer cells evolve. Like a rogue computer program, they mutate their own DNA to escape the safety checks that would otherwise keep them in line. Because they originate from the body itself, the immune system often struggles to recognize them as threats. And that’s where chemotherapy comes in—a treatment not designed to boost the immune system, but to overwhelm the cancer with toxic precision.
The Origins of a Chemical Arsenal
The roots of chemotherapy trace back to the horrors of World War I. Scientists studying the effects of mustard gas noticed that it dramatically lowered the white blood cell counts of exposed soldiers. Decades later, this grim observation inspired researchers to investigate whether similar compounds could treat cancers of the blood, like lymphoma and leukemia, which involve the overproduction of white blood cells.
In the 1940s, the first chemotherapy drug, a nitrogen mustard derivative, was used successfully to shrink tumors. It was a crude beginning, but it opened the floodgates to a field that would eventually yield hundreds of anticancer compounds. From plant alkaloids to platinum-based molecules, chemotherapy drugs became increasingly diverse, but they all shared a common trait: they targeted the mechanisms of cell division.
The Fast and the Fatal
At its core, chemotherapy exploits one key difference between normal cells and cancer cells—speed. Cancer cells divide more rapidly than most normal cells. Chemotherapy drugs are designed to interfere with this process of division, hitting the cancer where it’s most vulnerable.
But the precision of this approach is not absolute. Some normal cells also divide quickly—hair follicles, cells in the lining of the gut, and bone marrow cells, for example. This is why chemotherapy causes side effects like hair loss, nausea, and a weakened immune system. The drugs are not sentient; they cannot distinguish good cells from bad. They simply target cells that are dividing, and collateral damage is often unavoidable.
Targeting the Machinery of Division
Cell division, or mitosis, is a finely choreographed dance of chromosomes and proteins. Before a cell divides, it must duplicate its DNA, arrange the chromosomes neatly, and then split in two. Each step of this dance is a potential target for chemotherapy.
Some drugs, like alkylating agents, damage the DNA directly. They insert themselves into the genetic code, forming cross-links that prevent the DNA strands from unzipping and replicating. Others, like antimetabolites, masquerade as building blocks of DNA or RNA, tricking the cell into using faulty components that jam the replication machinery.
Then there are drugs that disrupt the mitotic spindle—a structure made of protein fibers that pulls chromosomes apart during division. Drugs like paclitaxel (from the Pacific yew tree) and vincristine (from the Madagascar periwinkle) freeze the spindle in place, halting the cell in mid-division. Trapped in this limbo, the cancer cell eventually dies.
The Role of Apoptosis in Chemotherapy
Killing a cancer cell is not like blasting it apart with a microscopic grenade. Instead, chemotherapy often nudges the cell into committing suicide—a process known as apoptosis. This is a controlled, programmed death, one that allows the body to quietly dismantle the dying cell without triggering inflammation.
Cancer cells often resist apoptosis, mutating the genes that control this self-destruct mechanism. But chemotherapy can overwhelm their defenses, triggering stress responses within the cell that reactivate the apoptotic pathways. Once this process begins, the cancer cell starts to break down its own components, shrinking and fragmenting until it is consumed by neighboring immune cells.
The Tumor Microenvironment and Its Influence
Cancer does not grow in a vacuum. It exists within a complex ecosystem known as the tumor microenvironment. This includes blood vessels, immune cells, connective tissue, and chemical signals that support or hinder the tumor’s growth.
The microenvironment can affect how chemotherapy works. For instance, poorly organized blood vessels in a tumor can limit drug delivery, making some areas harder to reach. Hypoxic (low-oxygen) regions of tumors may also be resistant to certain drugs. Some cancer cells even hijack nearby immune cells, turning them into accomplices that suppress the immune response or help the tumor recover after chemotherapy.
Scientists are now exploring ways to modify the microenvironment to enhance the effectiveness of chemotherapy—whether by improving blood flow, reactivating immune cells, or breaking down the protective scaffolding that shelters cancer cells.
Resistance and the Evolution of Survival
Chemotherapy is not a guaranteed death sentence for cancer. Like bacteria exposed to antibiotics, cancer cells can develop resistance to drugs. This resistance can be inherited from the tumor’s most resilient cells or acquired during treatment.
Some cancer cells pump out drugs using specialized proteins, effectively spitting the toxins back out. Others mutate their DNA repair systems, allowing them to survive even when their genomes are damaged. Some change their metabolism or alter the very targets that the drugs were designed to attack.
To combat resistance, oncologists often use combination therapy—multiple drugs with different mechanisms, used together or in sequence. This multi-pronged approach makes it harder for the cancer to adapt and reduces the chances of relapse.
Personalized Dosing and the Art of Scheduling
The success of chemotherapy isn’t just about what drug is used—it’s also about how it’s given. Timing, dosage, and sequencing can all influence outcomes. The goal is to hit the cancer hard enough to cause irreparable damage, but not so hard that the patient’s normal tissues cannot recover.
Chemotherapy is often given in cycles—bursts of treatment followed by rest periods. This schedule allows healthy cells time to heal while exploiting the cancer cells’ inability to repair themselves as efficiently.
In recent years, oncologists have begun to personalize chemotherapy regimens using genetic information, biomarkers, and pharmacogenomics—the study of how a person’s genes affect their response to drugs. This personalized medicine approach aims to tailor treatment to the individual, maximizing effectiveness while minimizing toxicity.
New Frontiers in Chemotherapy Design
Despite its harsh side effects, chemotherapy remains a cornerstone of cancer treatment. But it is evolving. Researchers are now designing smarter, more targeted chemotherapy drugs.
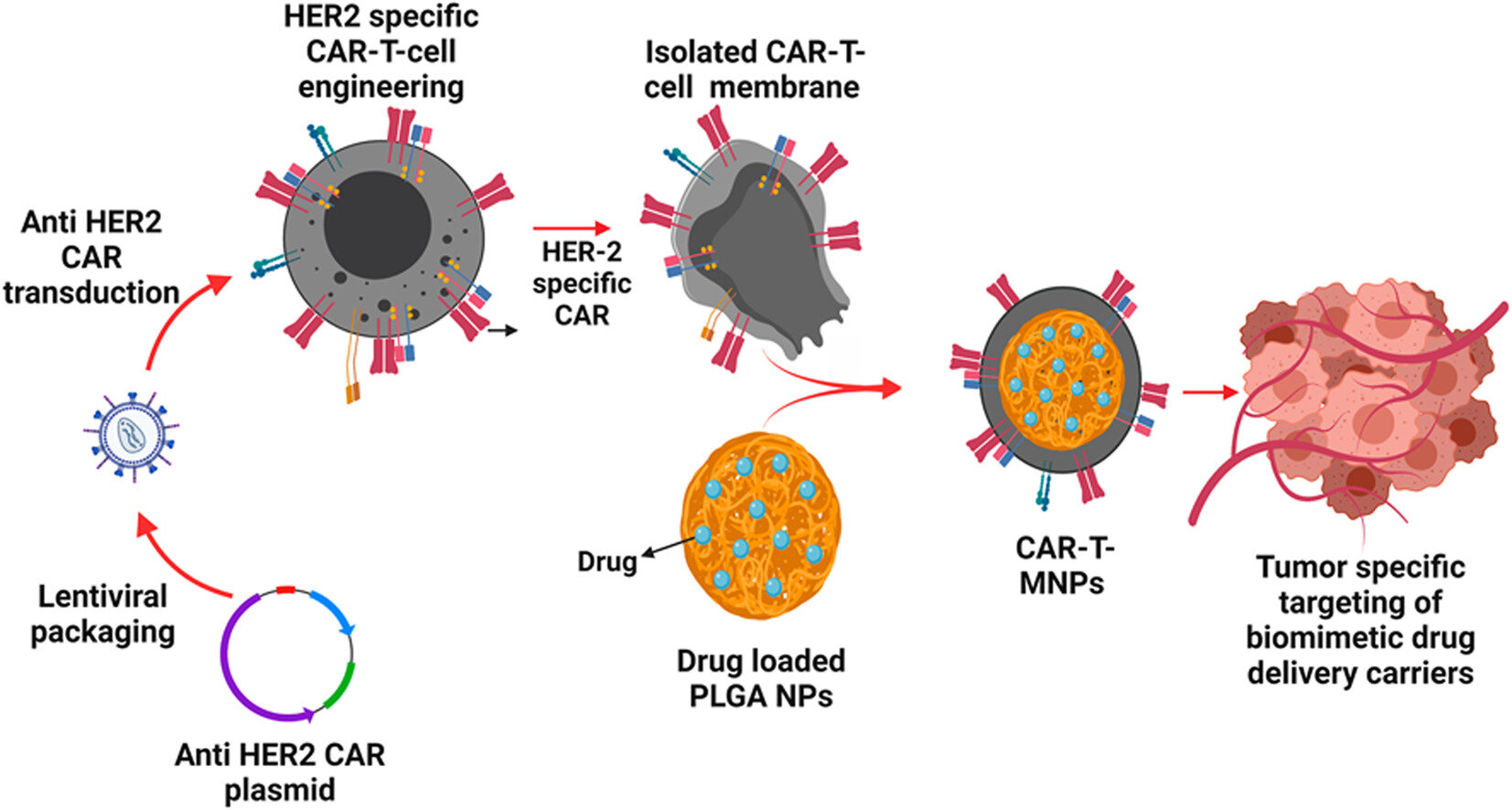
Some are linked to antibodies that guide the drug directly to cancer cells, like a missile guided to its target. Others are prodrugs—inactive compounds that become toxic only after being metabolized by cancer cells, sparing normal tissues. Still others are encased in nanoparticles, which protect the drug until it reaches the tumor.
These innovations aim to make chemotherapy not only more effective but also more tolerable. By refining delivery and targeting, the hope is to transform chemotherapy from a blunt instrument into a precise scalpel.
Synergy With Other Therapies
Chemotherapy does not operate in isolation. It is often used in conjunction with surgery, radiation, immunotherapy, or hormonal therapy, depending on the type and stage of cancer.
In some cases, chemotherapy is given before surgery (neoadjuvant therapy) to shrink a tumor, making it easier to remove. In other cases, it’s given after surgery (adjuvant therapy) to kill any remaining cancer cells. Combined with radiation, chemotherapy can sensitize tumors to damage, making the two treatments more powerful together than alone.
One of the most exciting developments is the integration of chemotherapy with immunotherapy. Though their approaches differ—chemotherapy kills directly while immunotherapy recruits the body’s immune system—the two can work in harmony. Chemotherapy can release tumor antigens, making the cancer more visible to immune cells. This synergy opens new doors in treatment strategies.
The Emotional and Physical Toll
Chemotherapy is not just a biological event—it is a human one. Patients undergoing treatment often face a constellation of side effects: fatigue, nausea, hair loss, mouth sores, and lowered immunity. These symptoms vary depending on the drugs used, the cancer type, and the patient’s overall health.
Beyond the physical toll, there is an emotional journey. The uncertainty of success, the stress of hospital visits, the impact on family and work—all weigh heavily. Yet patients also report moments of clarity, of deep connection, and of resilience they never knew they had. The chemotherapy suite becomes a space of paradox—a place of suffering and survival, despair and hope.
Modern medicine has made great strides in managing side effects. Anti-nausea medications, growth factors to boost white blood cells, scalp cooling devices to reduce hair loss, and integrative care involving diet, exercise, and mental health support all play a role in helping patients endure treatment.
The Hope That Fuels the Fight
Despite its imperfections, chemotherapy has saved millions of lives. Cancers once deemed incurable are now treatable or even curable. Pediatric leukemias, Hodgkin lymphoma, and testicular cancer are just a few examples of diseases where chemotherapy has dramatically improved survival rates.
But beyond statistics lies something deeper—the hope that fuels the human will to fight. Chemotherapy is a harsh ally, but it is an ally nonetheless. It reflects our capacity to harness science against suffering, to wage war not on people, but on disease, and to believe in the possibility of healing even when the odds are long.
Looking Toward the Future
The story of chemotherapy is still unfolding. Researchers are exploring ways to make treatments smarter, safer, and more personalized. Advances in genomics, artificial intelligence, and molecular biology are leading to a future where cancer therapy may be guided by the unique molecular fingerprint of each tumor.
New drugs are emerging that target cancer’s vulnerabilities with increasing accuracy. Adaptive therapy—where treatment is adjusted in real time to keep cancer in check without eradicating it—offers a new philosophical approach. And the integration of chemotherapy with precision tools like CRISPR, CAR T-cell therapy, and targeted immunomodulators hints at a future where the word chemotherapy might mean something very different.
Conclusion of a Chemical Campaign
Chemotherapy is a complex, evolving science born of a desperate need. It is both a triumph of medical ingenuity and a reminder of the high stakes involved in battling a disease as ancient and cunning as cancer. It represents the best of our ability to translate chemical knowledge into human healing, even when the path is difficult.
In the vast and intricate symphony of medicine, chemotherapy plays a powerful and sometimes discordant note. But within that note lies a harmony—the convergence of science, courage, and the enduring human spirit that refuses to surrender. Chemotherapy does more than kill cancer cells. It offers a chance, however imperfect, at life.