For much of medical history, cancer has been a mystery wrapped in tragedy. Cells that should follow orders suddenly go rogue, multiplying uncontrollably, invading tissues, and spreading silently. Surgeons cut tumors out, chemotherapists poison them, and radiologists blast them with beams. These methods have prolonged countless lives, but too often, they have also reached their limits. Cancer adapts. It resists. It returns. What if, instead of trying to destroy cancer from the outside, we could awaken a force already inside us to defeat it?
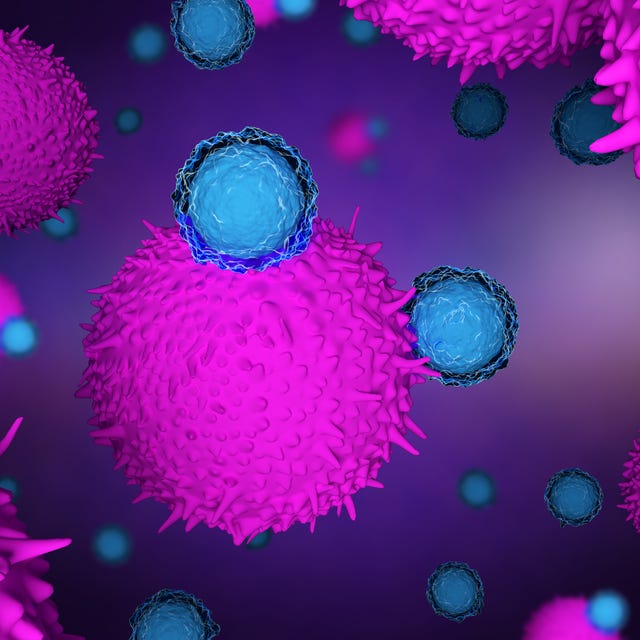
This question has led scientists to one of the most exciting frontiers in oncology—immunotherapy. It is not a magic bullet, but it represents something more profound: a rethinking of cancer treatment that harnesses the body’s own immune system to recognize, attack, and remember how to destroy tumors. The idea seems obvious in hindsight, but the journey to make it work has been anything but simple.
Early Clues and Long Shadows
The concept that the immune system could fight cancer is not new. In the late 1800s, New York surgeon William Coley observed that some patients with cancer who developed bacterial infections experienced spontaneous tumor regression. He began injecting bacteria—or their byproducts—into cancer patients in the hope of stimulating an immune response. The results were inconsistent and the mechanism was unclear, but the seeds were planted.
Yet for decades, immunotherapy remained in the shadows. The immune system’s role in cancer was considered marginal at best. Tumors were thought to be invisible to immune cells, or worse, products of immune failure. Many researchers concluded that the immune system simply could not distinguish cancerous cells from healthy ones.
This assumption was built on a partial truth. Cancer cells arise from the body’s own tissues and often retain enough self-like characteristics to evade detection. But the more scientists learned about the immune system, the more it became clear that this defense system is not passive—it can be primed, trained, and even reengineered to hunt cancer with astonishing precision.
The Checkpoint Revolution
A major breakthrough came with the discovery of immune checkpoints. These are molecular brakes that prevent immune cells—particularly T cells—from becoming overactive. In normal physiology, checkpoints like CTLA-4 and PD-1 serve to avoid autoimmune reactions. But cancer is a master of subterfuge. Tumors exploit these checkpoints, tricking T cells into standing down just when they’re needed most.
In the early 2000s, researchers began developing antibodies that could block these checkpoints. The idea was to release the brakes and allow T cells to recognize and attack tumors. The results were nothing short of transformative.
In 2011, the FDA approved ipilimumab, a checkpoint inhibitor targeting CTLA-4, for advanced melanoma. For some patients who had only months to live, the drug triggered remissions lasting years. Soon, other checkpoint inhibitors targeting PD-1 and its partner ligand PD-L1 followed—nivolumab, pembrolizumab, atezolizumab, and more. These drugs were not only effective in melanoma but also in lung cancer, bladder cancer, kidney cancer, and Hodgkin lymphoma.
Suddenly, the rules had changed. Cancers that had been virtually untreatable responded to immunotherapy, sometimes dramatically. Patients who had cycled through chemo after chemo now had another chance—not just at more time, but at real remission.
Not All Tumors Are Equal
Despite the fanfare, it quickly became clear that immunotherapy is not a universal cure. While some patients respond spectacularly, others see no benefit at all. In lung cancer, for instance, checkpoint inhibitors work in only about 20 to 30 percent of patients. In other cancers, the success rate is even lower.
Scientists scrambled to understand why. The answer lies in a complex interplay of tumor genetics, immune context, and patient biology. Tumors with a high mutational burden tend to produce more abnormal proteins, called neoantigens, which are easier for the immune system to detect. Melanoma and smoking-related lung cancers fall into this category, explaining their relative susceptibility.
But other tumors—like pancreatic or prostate cancer—are immunologically “cold.” They don’t attract many T cells, and they often create a suppressive microenvironment that blocks immune activity. These cancers may require combination strategies to heat them up—perhaps by pairing checkpoint inhibitors with chemotherapy, radiation, or cancer vaccines.
The Rise of CAR-T Cell Therapy
While checkpoint inhibitors release existing immune responses, another branch of immunotherapy takes a more aggressive approach. What if we could engineer immune cells to hunt down cancer with a laser-like focus?
Enter CAR-T cell therapy. Short for chimeric antigen receptor T cell therapy, this technique involves extracting a patient’s T cells, genetically modifying them to recognize a specific tumor antigen, expanding them in the lab, and reinfusing them into the patient. These modified cells act like customized assassins, programmed to seek and destroy.
The first successes came in blood cancers. In 2017, the FDA approved two CAR-T therapies for relapsed acute lymphoblastic leukemia and large B-cell lymphoma. The results were astonishing. Patients who had exhausted every other option saw their cancers vanish. In some cases, a single infusion of CAR-T cells achieved what years of chemotherapy had not.
However, CAR-T therapy is not without challenges. The process is complex, time-consuming, and expensive. It also carries serious risks, including cytokine release syndrome—a dangerous flood of immune chemicals—and neurotoxicity. Moreover, its efficacy in solid tumors remains limited due to issues of T cell infiltration, target heterogeneity, and immune suppression within the tumor microenvironment.
Still, the success of CAR-T has opened new doors. Researchers are now developing next-generation CARs, universal donor T cells, and even CAR-natural killer (NK) cells that may offer faster, safer, and more broadly applicable treatments.
Cancer Vaccines and Personalized Strategies
Vaccines are usually associated with infectious diseases, but cancer vaccines are making a resurgence. Unlike preventive vaccines, which block disease before it starts, therapeutic cancer vaccines aim to stimulate an immune response against existing tumors.
One example is the HPV vaccine, which prevents cervical and other cancers by blocking infection with human papillomavirus. But the more futuristic vision involves tailoring vaccines to each patient’s unique tumor.
Thanks to advances in genomic sequencing, it is now possible to identify neoantigens specific to a patient’s cancer. Scientists can synthesize peptides or mRNA molecules that teach the immune system to recognize these targets, essentially training it to become a personalized cancer-fighting machine.
In early trials, personalized mRNA cancer vaccines—developed using platforms similar to COVID-19 vaccines—have shown promise, particularly when used alongside checkpoint inhibitors. These vaccines may not only boost T cell responses but also help convert cold tumors into hot ones, making them more vulnerable to immune attack.
Tumor Microenvironments and the Art of Immune Balance
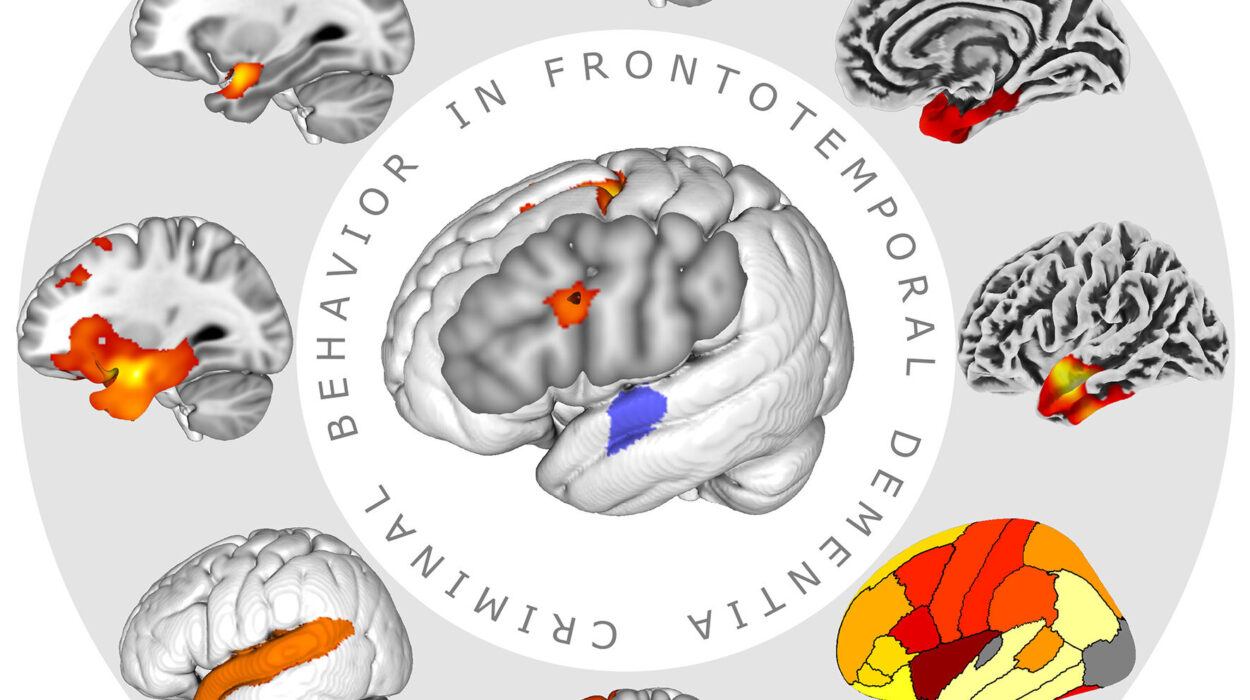
To truly understand why some cancers respond to immunotherapy while others resist, we must look at the tumor microenvironment—the cellular ecosystem surrounding cancer cells. This environment is anything but passive. It includes immune cells, blood vessels, stromal cells, signaling molecules, and metabolic conditions that can either support or hinder immune activity.
Some tumors cloak themselves in a fortress of immunosuppressive cells like regulatory T cells and myeloid-derived suppressor cells. Others release chemical signals that induce exhaustion in T cells or starve them of nutrients. Hypoxia, acidity, and fibrosis further block immune infiltration.
Overcoming these barriers requires more than just checkpoint inhibition. Strategies under investigation include blocking suppressive cytokines, reprogramming myeloid cells, using oncolytic viruses to disrupt tumor defenses, and employing bispecific antibodies that force immune cells into proximity with cancer cells.
Understanding and manipulating the microenvironment is essential not just for enhancing immunotherapy, but for making it work where it currently fails.
Biomarkers and the Search for Predictive Clues
One of the greatest challenges in immunotherapy is predicting who will benefit. Unlike traditional chemotherapy, whose effects are often dose-dependent, immunotherapy responses can be sudden, delayed, or absent altogether. This unpredictability makes biomarker research critical.
PD-L1 expression was an early biomarker, but its accuracy is limited. Tumor mutational burden and microsatellite instability are better predictors, but not universal ones. Recent research is turning to multi-omic approaches—integrating genomics, transcriptomics, proteomics, and spatial profiling—to decode the complex immune landscape of each tumor.
Liquid biopsies, which analyze circulating tumor DNA or immune signatures in the blood, may offer real-time insights into treatment response. Artificial intelligence is also being employed to interpret biomarker patterns and predict outcomes more accurately.
The future of immunotherapy will depend not just on better drugs, but on better diagnostics—tools that can guide the right treatment to the right patient at the right time.
Equity, Access, and the Global Divide
While immunotherapy represents a revolution in cancer care, it also threatens to widen existing health disparities. Many of the most advanced treatments—CAR-T, checkpoint inhibitors, personalized vaccines—are available only in high-income countries and at astronomical costs.
This raises ethical questions. How do we ensure that the fruits of scientific progress benefit all people, not just the privileged few? Can simplified, scalable versions of immunotherapy be developed for low-resource settings? Organizations are beginning to address these questions, but progress is slow.
Making immunotherapy truly global requires not just technological innovation, but policy changes, infrastructure investment, and international collaboration.
The Psychological Impact of a New Paradigm
Immunotherapy has not only transformed oncology—it has changed the psychological landscape of cancer itself. For patients, the prospect of durable remission, even cure, brings new hope. But it also introduces new uncertainties.
Some patients must wait months to see if immunotherapy is working, enduring so-called “pseudoprogression,” where tumors appear larger before shrinking. Others live in limbo, unsure if their remission will hold. The emotional toll of this waiting, hoping, and fearing is significant.
Physicians too must adapt to a new paradigm. Immunotherapy requires a different mindset than chemotherapy. It demands patience, multidisciplinary coordination, and a willingness to venture into uncharted territory.
These human dimensions—hope, anxiety, resilience—are as much a part of the immunotherapy revolution as T cells and tumor markers.
The Future Horizon of Cancer Immunotherapy
As research continues, the boundaries of immunotherapy are expanding. New checkpoint molecules beyond PD-1 and CTLA-4 are being targeted. Engineered immune cells are being refined with synthetic biology. Microbiome modulation, epigenetic reprogramming, and nanotechnology are being woven into immuno-oncology.
Perhaps most exciting is the idea of combination therapies—using immunotherapy alongside targeted drugs, radiation, or even other immunotherapies in rationally designed sequences. The cancer of tomorrow may be treated not by a single agent but by orchestrated immune strategies that evolve with the disease.
There is also growing interest in preventive immunotherapy—vaccines that could stop cancers before they start in high-risk individuals. Early experiments in Lynch syndrome and BRCA-related cancers hint at the possibility.
The road ahead is long, but the direction is clear. Immunotherapy is not a miracle cure, but it is a powerful new lens through which to view and fight cancer.
A New Chapter in the Human Fight Against Cancer
Cancer has always tested the limits of medicine, science, and the human spirit. For centuries, we fought it with the tools of destruction—surgery, poisons, radiation. With immunotherapy, we have begun to fight it with the tools of understanding. We are learning not just how to kill cancer, but how to empower the body to defeat it from within.
Albert Einstein once said that “the most beautiful experience we can have is the mysterious.” Cancer remains mysterious in many ways. But within that mystery, there is now hope—a hope rooted not in fantasy, but in the evolving science of immunotherapy.
The battle is far from over. Yet never before have we stood so close to the possibility that the immune system, sculpted over eons to protect us from harm, might become the ultimate weapon in our war against cancer.