Acne is often framed as a teenage rite of passage, the awkward skin rebellion that vanishes once adulthood arrives. But what happens when the pimples don’t leave? For millions of women, the breakouts persist—or even begin—for the first time in their twenties, thirties, or forties. This isn’t just lingering adolescent acne. It’s something more insidious, more persistent, and more deeply rooted in the body’s hormonal landscape. This is hormonal acne.
Hormonal acne doesn’t play by the typical skincare rules. It doesn’t care if you wash your face religiously or dab on expensive creams before bed. It tends to show up like an uninvited guest right before your period, often on your chin, jawline, or cheeks—just where it’s hardest to conceal. And because it’s driven by internal imbalances, external treatments only offer temporary relief. Understanding how to manage hormonal acne requires a shift in perspective: it’s not just a cosmetic concern but a sign of deeper hormonal conversations happening beneath your skin.
What Hormonal Acne Really Is
At its core, hormonal acne is triggered by fluctuations or imbalances in your body’s natural hormone levels. The culprits are often androgens—“male” hormones that all women have in smaller amounts, such as testosterone. When these hormones become elevated or overly active, they stimulate the skin’s sebaceous (oil) glands to produce more sebum. Combine that excess oil with dead skin cells and bacteria, and you’ve got the perfect recipe for clogged pores, inflammation, and the kind of deep, painful pimples that seem to last forever.
But hormonal acne isn’t just about androgens running wild. Estrogen, progesterone, cortisol, and even insulin all play supporting roles in this skin saga. Stress, diet, menstrual cycles, polycystic ovary syndrome (PCOS), and birth control decisions can all tip the hormonal scales and trigger breakouts. That’s why hormonal acne can feel so confusing and frustrating—it’s not just about what you put on your face, but how your body is functioning as a whole.
The Hormone-Skin Connection
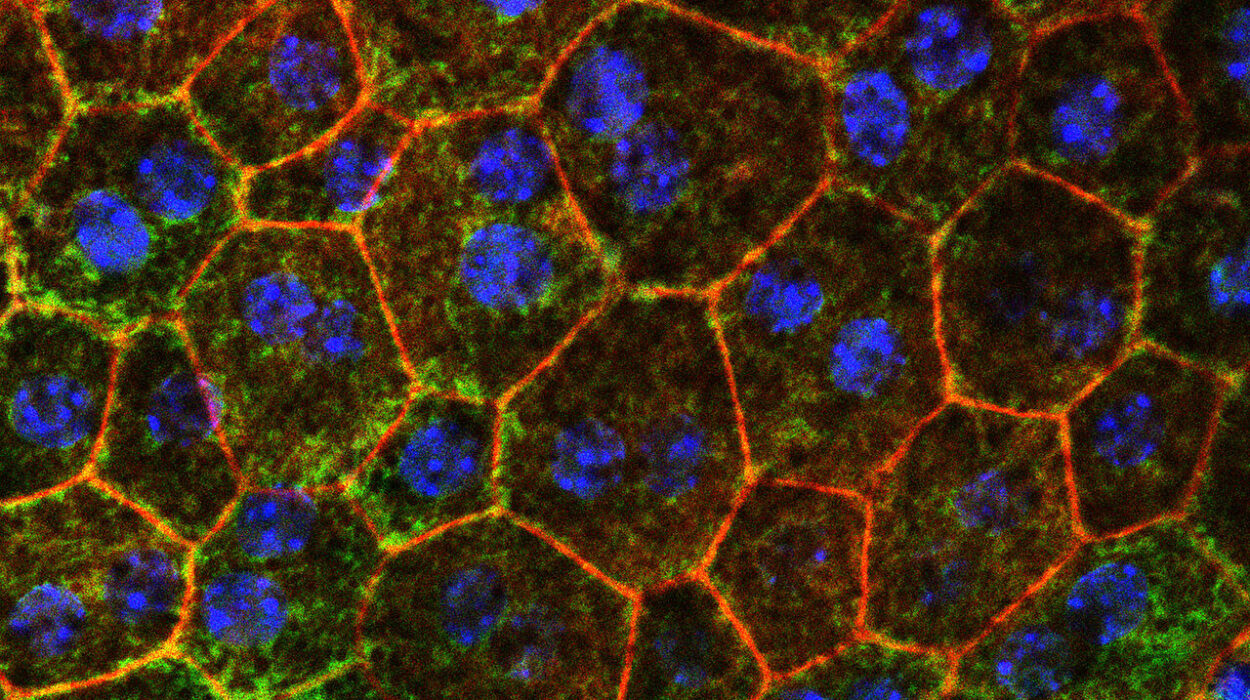
To really get to the root of hormonal acne, you have to understand the intricate relationship between hormones and skin health. The skin is a hormonal organ. Yes, you read that right. Your skin doesn’t just respond to hormones—it actually produces some itself and has receptors that are finely tuned to pick up hormonal signals.
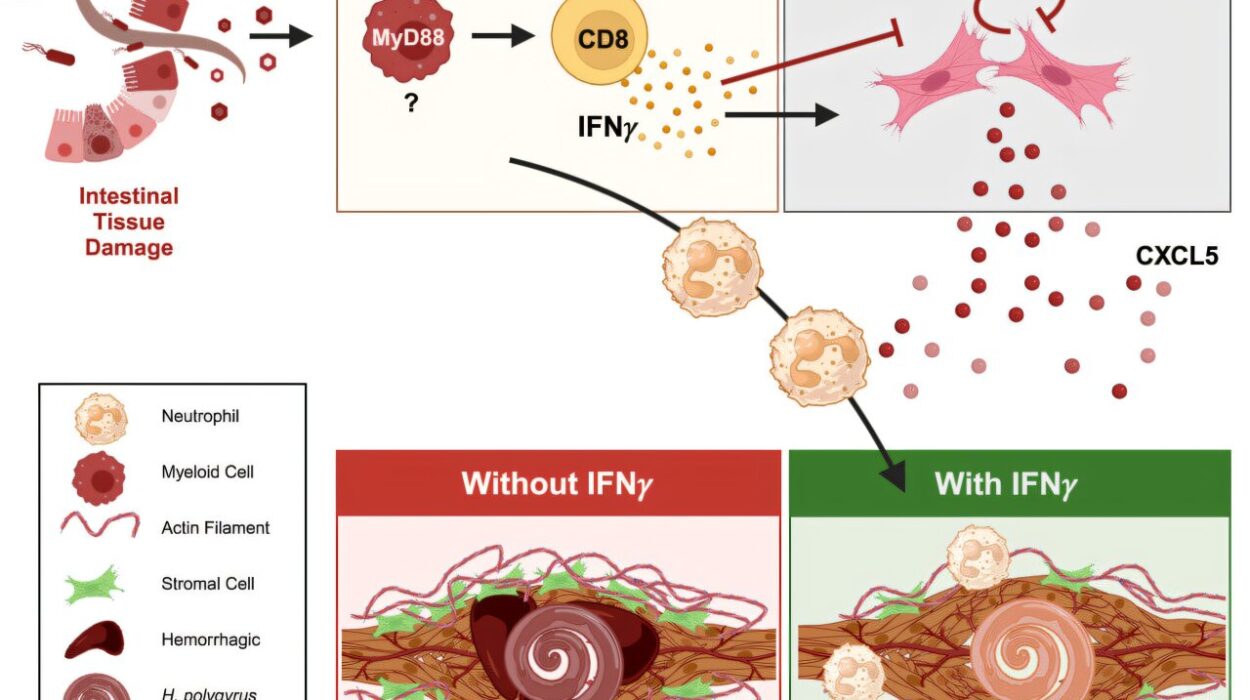
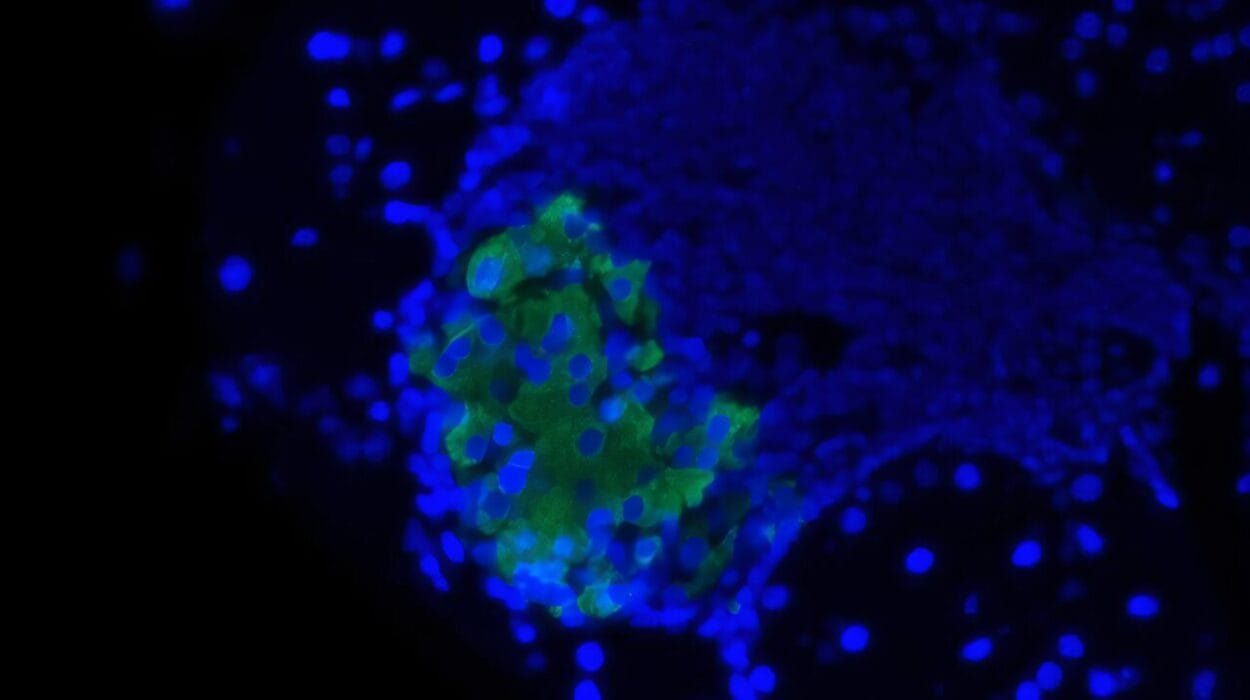
Androgens like testosterone can increase oil production by binding to receptors in sebaceous glands. In women with hormonal imbalances, this increase in sebum often creates the ideal environment for the bacteria Cutibacterium acnes to flourish. This bacteria thrives in oil-rich environments and triggers the immune system to respond, leading to inflammation, redness, and those painful under-the-skin cysts that define hormonal acne.
Meanwhile, estrogen and progesterone also influence sebum production and skin cell turnover. When estrogen levels drop—like in the days before menstruation—testosterone can temporarily gain the upper hand. This is why many women notice a breakout pattern that follows their cycle. And if you have conditions like PCOS, where androgens may be consistently elevated, the acne can be more chronic and difficult to manage without a multi-pronged approach.
Signs You’re Dealing with Hormonal Acne
It can be tough to know whether your acne is hormonal or just stubborn, but there are some telltale signs. Hormonal acne often appears in a predictable pattern—on the lower face, jawline, and neck—and tends to flare up cyclically, often around menstruation. It may include deep, painful cysts that take weeks to heal and often leave behind dark marks or scarring.
This type of acne is also often resistant to conventional treatments like over-the-counter benzoyl peroxide or salicylic acid. It’s like your skin is saying, “Nice try, but this isn’t just about clogged pores.” Hormonal acne doesn’t just pop up out of nowhere—it usually corresponds with bigger shifts in your body, whether it’s coming off birth control, dealing with chronic stress, navigating perimenopause, or managing a condition like PCOS or insulin resistance.
Understanding these patterns and timing is essential. Hormonal acne is your body’s way of flagging an internal issue. The skin isn’t betraying you; it’s sending a message.
Why Conventional Treatments Often Fail
Walk down any skincare aisle and you’ll be bombarded with promises: this cleanser will purify, that serum will exfoliate, this cream will calm your angry skin. While these topical treatments can help manage the symptoms, they rarely address the underlying hormonal chaos that fuels recurring breakouts.
The reality is that most conventional acne treatments were designed with teenagers in mind—teenagers who are experiencing temporary, puberty-induced acne. These products often focus on drying out the skin, targeting bacteria, or increasing cell turnover. And while that might work for mild, surface-level acne, hormonal acne operates at a deeper level.
In fact, overuse of harsh products can backfire, stripping the skin of its natural moisture barrier and triggering even more oil production. This leads to a vicious cycle: breakout, treat, inflame, break out again. Breaking this cycle means stepping back and looking beyond the surface—literally and metaphorically.
Healing Hormonal Acne from the Inside Out
To truly manage hormonal acne, you need a holistic strategy that goes beyond spot treatments. It starts with understanding your body’s unique hormone blueprint and supporting balance through lifestyle, nutrition, stress reduction, and sometimes medical intervention.
One of the most powerful ways to support hormone health is through diet. Your skin is a reflection of what’s happening in your gut, your liver, and your bloodstream. Foods that spike insulin—like refined carbs and sugary snacks—can increase androgen levels and worsen acne. Dairy products, particularly milk, have also been linked to breakouts in some people, possibly because of the hormones and growth factors they contain.
On the flip side, foods rich in omega-3 fatty acids, antioxidants, fiber, and phytoestrogens can support healthy hormone metabolism and reduce inflammation. Think of leafy greens, berries, flaxseeds, fatty fish, and cruciferous vegetables like broccoli and kale. These aren’t just “good for you”—they’re good for your skin at the cellular level.
Gut health also plays a role. An imbalance in the gut microbiome can trigger systemic inflammation and interfere with hormone detoxification. Supporting your gut with probiotics, fermented foods, and adequate fiber can help keep your skin—and hormones—in check.
The Role of Stress and Sleep
Stress is like throwing gasoline on the hormonal acne fire. When you’re stressed, your body releases cortisol, the primary stress hormone. Cortisol doesn’t just make you feel anxious—it also stimulates the sebaceous glands to produce more oil, which can lead to clogged pores and breakouts. Chronic stress also disrupts blood sugar and hormone regulation, creating a perfect storm for acne to flourish.
Sleep is your body’s natural reset button. During deep sleep, hormone production stabilizes, inflammation decreases, and cellular repair takes place. Skimping on sleep throws off your circadian rhythm, which affects everything from cortisol levels to insulin sensitivity. If you’re dealing with hormonal acne, prioritizing restorative sleep is not a luxury—it’s a non-negotiable step in your healing journey.
Managing stress isn’t about avoiding every deadline or becoming a monk. It’s about building resilience and creating rituals that calm your nervous system: daily movement, mindfulness practices, breathwork, and even simple pleasures like reading or taking a bath. Every stress management tool you use is a gift to your skin.
Understanding the Role of Birth Control
For many women, birth control is both a cause and a potential solution for hormonal acne. Some oral contraceptives can help regulate hormone levels by suppressing ovulation and reducing androgen production. This can lead to clearer skin for some users. However, birth control is not a one-size-fits-all solution. In some cases, particularly with progestin-only methods, it can actually worsen acne.
And then there’s post-birth control acne—a phenomenon that many women experience when they stop taking hormonal contraception. Suddenly, the synthetic hormones that were keeping acne at bay are gone, and the body takes time to rebalance. This transition period can be especially difficult, and managing it often requires patience and support from both skincare and internal health strategies.
If you’re considering going off birth control or switching methods, it’s important to have a plan. Supporting your body through this transition with hormone-friendly nutrition, detox support, and perhaps even supplements can make a significant difference in how your skin responds.
Medical Interventions: What Works and What Doesn’t
While lifestyle changes form the foundation of hormonal acne management, some women may benefit from medical treatments. Spironolactone, for example, is a prescription medication that blocks androgen receptors and reduces oil production. It has been a game-changer for many women with stubborn hormonal acne.
Other treatments may include topical retinoids (which increase cell turnover and reduce pore blockage), antibiotics for acute flare-ups, or even isotretinoin (Accutane) for severe cases. However, these options come with potential side effects and are best considered under the guidance of a knowledgeable dermatologist.
It’s also crucial to understand that medical treatments alone may not lead to lasting results unless hormonal imbalances are addressed concurrently. The goal is not just to suppress symptoms but to create a sustainable environment where your skin can thrive.
The Power of a Personalized Approach
No two bodies—and no two breakouts—are exactly alike. That’s why the most effective approach to hormonal acne is one that is tailored to your unique hormone profile, lifestyle, and skin type. This may involve working with a dermatologist, endocrinologist, or functional medicine practitioner who can run hormone tests, assess your gut health, and guide you through a comprehensive healing plan.
This might also include cycle tracking to understand how your hormones fluctuate throughout the month, or targeted supplementation with nutrients like zinc, DIM (diindolylmethane), magnesium, and omega-3s. Even subtle lifestyle tweaks—like balancing blood sugar, reducing caffeine, or supporting liver detoxification—can have a profound impact over time.
The key is to approach hormonal acne not as an enemy to be vanquished, but as a messenger pointing you toward deeper healing. By listening to your body, supporting your hormones, and treating your skin with compassion, you can begin to shift from frustration to empowerment.
Redefining Beauty in the Face of Breakouts
It’s easy to fall into the trap of thinking clear skin equals health, happiness, or worth. But hormonal acne often arrives as a paradox: you may be doing all the right things and still wake up to painful flare-ups. This isn’t a failure—it’s biology. And healing is rarely linear.
One of the most radical things you can do is refuse to let acne define your confidence or your beauty. Your skin is not a measure of your discipline, your hygiene, or your value. It’s a living, breathing organ that is deeply connected to your hormones, your history, and your healing.
This doesn’t mean giving up on solutions—it means approaching them from a place of self-respect rather than shame. Skincare should feel like self-care, not punishment. And managing hormonal acne effectively isn’t just about what products you use or what foods you avoid. It’s about tuning in, supporting balance, and remembering that your skin is on your side.