The female body is a finely tuned symphony of hormones. These invisible messengers are constantly circulating, directing the tempo of metabolism, menstrual cycles, energy levels, mood, and fertility. When the orchestra is playing in harmony, everything works smoothly. But even the slightest disruption—say, too much of one hormone or too little of another—can throw the entire system out of sync. That disharmony is what we refer to as a hormonal imbalance.
For many women, the words “hormonal imbalance” feel painfully familiar. It can mean anything from fatigue that doesn’t go away with rest, to irregular periods, unexplained weight gain, or persistent acne. But within this wide landscape of hormonal disorders lies a particularly misunderstood condition: Polycystic Ovary Syndrome, better known as PCOS.
The confusion between PCOS and general hormonal imbalance is widespread. They share many symptoms, they often appear around the same time in life, and both can be deeply frustrating to navigate. But they are not the same thing.
To truly understand what separates PCOS from hormonal imbalance—and why that difference matters—we have to explore the female hormonal system, understand how it’s supposed to work, and then examine what happens when it doesn’t. We also need to unpack what PCOS really is, why it’s not a one-size-fits-all diagnosis, and how it fits into the much broader conversation about women’s health and hormonal function.
What Hormonal Balance Actually Means
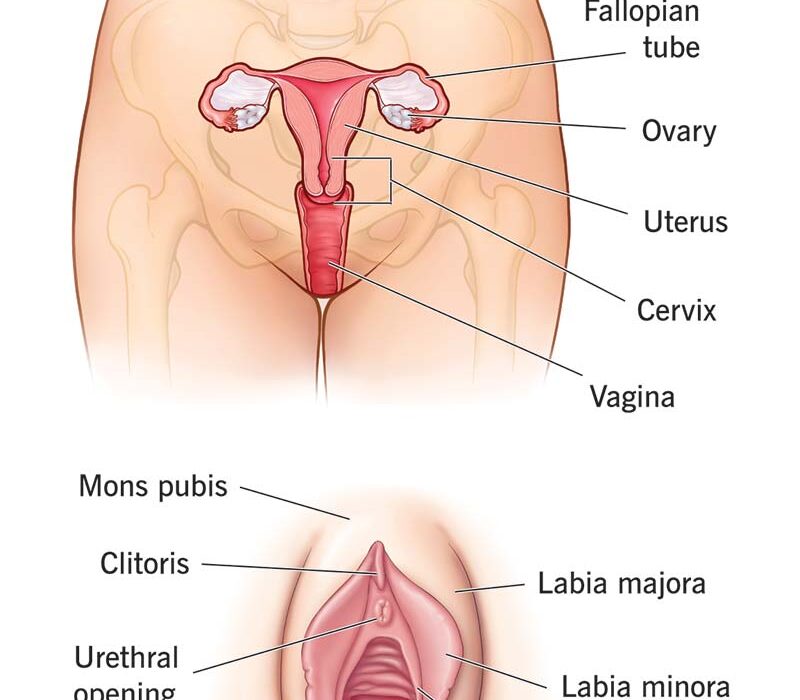
In a healthy body, hormones are constantly fluctuating, especially in women. It’s not about having the same levels all the time—it’s about having the right levels at the right time. The menstrual cycle itself is a hormonal rollercoaster, with estrogen and progesterone rising and falling in a beautifully orchestrated dance. The pituitary gland sends signals to the ovaries, the ovaries respond, and the endometrium prepares for a possible pregnancy. If pregnancy doesn’t occur, hormones shift again to signal menstruation.
Add to this the influence of insulin, cortisol, thyroid hormones, and testosterone, and you start to see just how dynamic and complex the hormonal system is. A hormonal imbalance happens when one or more of these players starts acting out of turn, whether that’s because of stress, diet, lifestyle, medical conditions, or genetics.
Hormonal imbalances can be temporary or chronic. They can be driven by underlying conditions or be the condition themselves. They can also vary wildly from one woman to another. Some might notice mood swings or irregular periods, others might experience sleep problems, weight fluctuations, or chronic fatigue. The effects of imbalance can ripple through every system in the body, affecting not just reproductive health but digestion, skin, hair, metabolism, and even mental health.
The Spectrum of Hormonal Imbalance
Hormonal imbalance isn’t a single diagnosis—it’s a broad umbrella that covers a wide range of disruptions in the endocrine system. One woman’s imbalance might be rooted in an underactive thyroid (hypothyroidism), while another’s might stem from excess cortisol due to chronic stress. Yet another might be dealing with low progesterone, high androgens, or insulin resistance.
Some of the most common types of hormonal imbalances that affect women include:
- Estrogen dominance
- Low progesterone
- High testosterone
- Insulin resistance
- Thyroid dysfunction (hypothyroidism or hyperthyroidism)
- Adrenal fatigue (a controversial and debated diagnosis, but often associated with symptoms of hormonal dysregulation)
All of these can affect how the body functions, particularly the menstrual cycle and ovulation. But not all hormonal imbalances are PCOS—and that’s where many women and even healthcare providers get tripped up.
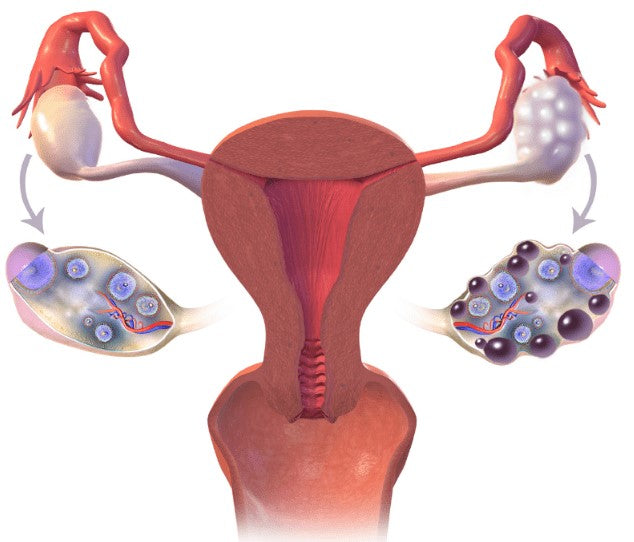
Decoding PCOS: More Than Just Cysts
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders in women, affecting approximately 1 in 10 women of reproductive age worldwide. Despite its name, PCOS is not defined by the presence of ovarian cysts—at least not exclusively.
PCOS is a syndrome, meaning it’s a collection of symptoms rather than a single, easily measurable disease. And like many syndromes, it presents differently in different people. While one woman might experience irregular periods and infertility, another might struggle with acne, hair growth in unusual places, and stubborn weight gain.
There are three primary features used to diagnose PCOS, according to the Rotterdam criteria (the most widely used diagnostic criteria):
- Irregular or absent ovulation (leading to irregular periods)
- Signs of high androgen levels (such as acne, excess facial or body hair, or elevated testosterone levels in blood tests)
- Polycystic ovaries seen on an ultrasound
A diagnosis of PCOS typically requires two of these three features. That means a woman could have regular periods and still have PCOS if she has high androgens and polycystic ovaries. Or she could have irregular periods and high androgens, but no visible cysts.
This complexity makes PCOS difficult to diagnose and easy to confuse with other hormonal disorders. It’s not uncommon for women to go years without a proper diagnosis, often being told that their symptoms are due to stress, weight, or simply “being a woman.”
The Hormonal Roots of PCOS
At its core, PCOS is a hormonal imbalance—but not all hormonal imbalances are PCOS. The key difference lies in which hormones are affected and how.
One of the hallmark features of PCOS is elevated androgens—male sex hormones like testosterone and DHEA. While women naturally produce small amounts of androgens, those with PCOS tend to produce more than usual, which can interfere with ovulation and cause symptoms like hirsutism (excess hair growth), acne, and hair thinning.
Another common feature of PCOS is insulin resistance. In fact, up to 70% of women with PCOS have some degree of insulin resistance, even if they’re not overweight. This means their cells don’t respond properly to insulin, forcing the pancreas to produce more and more to keep blood sugar in check. High insulin levels, in turn, can stimulate the ovaries to produce more androgens, creating a vicious hormonal cycle.
This interplay between insulin and androgens is what makes PCOS such a multifaceted condition. It’s not just a reproductive disorder—it’s also a metabolic one. That’s why women with PCOS are at a higher risk for developing type 2 diabetes, heart disease, and other metabolic conditions.
Why the Distinction Matters: Diagnosis and Treatment
Understanding the difference between PCOS and hormonal imbalance isn’t just an academic exercise—it has real implications for diagnosis, treatment, and long-term health.
If a woman is experiencing symptoms like irregular periods, weight gain, or acne, and is told she has a “hormonal imbalance” without further investigation, she might miss out on a proper PCOS diagnosis. Without that diagnosis, she might not get the targeted treatment she needs. Conversely, some women are incorrectly diagnosed with PCOS simply because they have irregular periods and ovarian cysts, when in fact their symptoms are due to something entirely different—like thyroid dysfunction or hypothalamic amenorrhea.
Treating hormonal imbalance depends entirely on what’s causing it. For someone with hypothyroidism, hormone replacement might be necessary. For someone with high cortisol, stress management and adrenal support could be key. But for someone with PCOS, treatment often involves managing insulin levels, reducing androgen production, and supporting ovulation.
That means a PCOS diagnosis opens the door to specific interventions—such as insulin-sensitizing medications, anti-androgens, or lifestyle changes tailored to metabolic health—that might not be recommended for someone with another kind of hormonal imbalance.
Navigating Life With PCOS
Living with PCOS is not a one-size-fits-all journey. For some women, it primarily affects fertility, making it difficult to conceive without medical assistance. For others, the impact is more cosmetic, with acne or unwanted hair causing emotional distress. For many, it’s the ongoing struggle with weight, fatigue, or mood swings that takes the biggest toll.
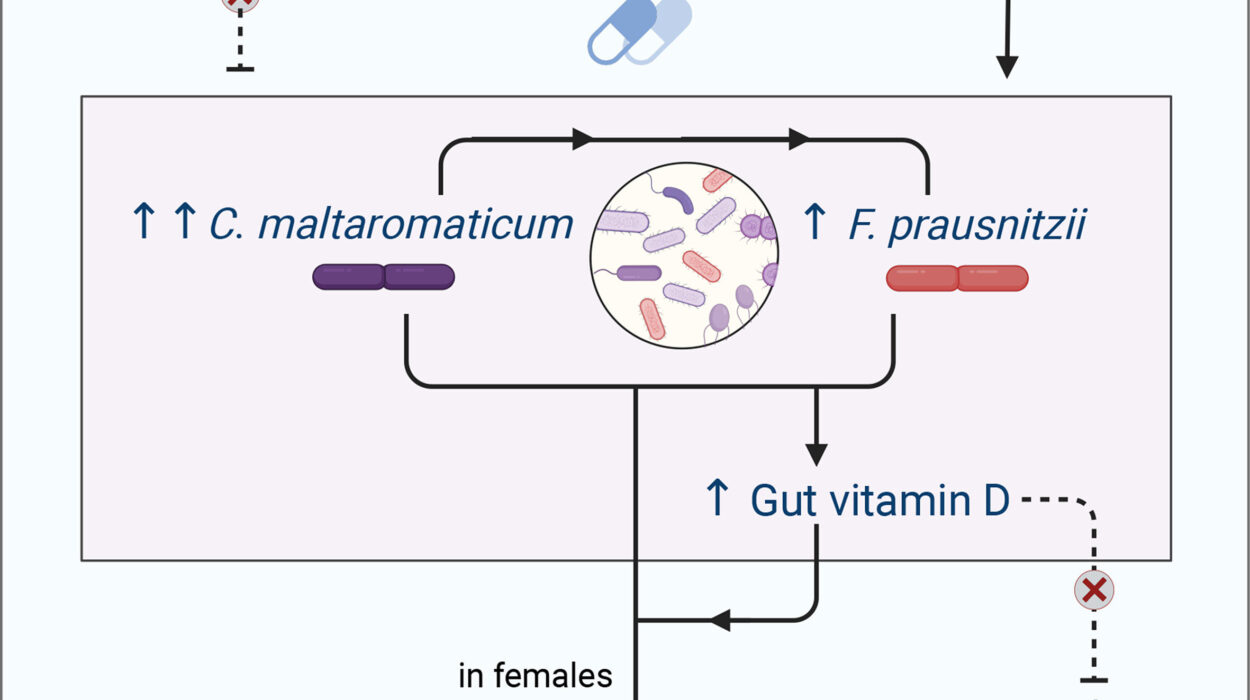
But despite its challenges, PCOS is manageable. Diet and lifestyle play a powerful role in managing symptoms. Research shows that even modest weight loss (5-10% of body weight) can improve insulin sensitivity, restore ovulation, and reduce androgen levels. Diets rich in whole foods, low in refined carbohydrates, and high in fiber tend to support hormonal balance in PCOS. Exercise, particularly strength training and moderate-intensity cardio, can also help regulate insulin and support hormonal health.
Supplements like inositol, omega-3 fatty acids, and vitamin D have shown promise in supporting women with PCOS, and many women find symptom relief through holistic approaches like acupuncture or herbal medicine. Medications such as metformin or hormonal birth control may be prescribed to address insulin resistance or cycle irregularity, but they are not cures.
The key is personalization—understanding what’s driving your symptoms and tailoring your approach accordingly. That’s why an accurate diagnosis is so crucial.
The Emotional Toll of Misunderstanding
The confusion between PCOS and hormonal imbalance isn’t just a medical issue—it’s an emotional one. Too many women are left feeling frustrated, dismissed, or gaslit by a system that doesn’t always take their symptoms seriously.
Being told you have a “hormonal imbalance” without clarity can feel like a non-answer. It’s vague, it lacks direction, and it doesn’t help women understand what’s actually happening in their bodies. On the other hand, receiving a PCOS diagnosis can come with its own emotional weight—fear of infertility, concerns about long-term health risks, or anxiety about lifelong management.
Both experiences can lead to feelings of isolation, confusion, and even shame. That’s why education and awareness are so powerful. When women understand their hormones, they can advocate for themselves, ask better questions, and make informed decisions about their health.
Bridging the Gap: Toward a Better Understanding
So where does that leave us? PCOS is a specific hormonal condition with distinct diagnostic criteria and a strong metabolic component. Hormonal imbalance is a broader term that can refer to many different disruptions in the body’s endocrine system.
Both deserve attention, and both can significantly impact quality of life. But lumping them together—or mislabeling one as the other—does a disservice to women everywhere.
What’s needed is better education, better screening, and better support. Healthcare providers need to dig deeper when a woman presents with hormonal symptoms, looking at the full picture rather than offering a blanket diagnosis. And women need to feel empowered to question, explore, and demand answers.
The path to hormonal health isn’t always straightforward. It requires curiosity, patience, and sometimes a bit of trial and error. But it’s a journey worth taking—because when your hormones are in harmony, everything else has a chance to fall into place.
The Future of Hormonal Health
The conversation around women’s hormonal health is finally starting to shift. Once considered too complex or too taboo, it’s now entering mainstream dialogue thanks to advocacy, research, and the growing chorus of women refusing to be ignored.
More studies are emerging about the intricacies of PCOS, hormonal rhythms, and how things like diet, gut health, environmental toxins, and stress play a role in endocrine function. New tools—from wearable tech to functional medicine testing—are helping women track their cycles and spot imbalances sooner.
The rise of integrative and functional medicine is also changing the way we approach hormonal conditions, treating them not just as isolated symptoms to be suppressed but as signals pointing to deeper systemic issues. The old model of masking symptoms with birth control is giving way to a new approach that prioritizes root cause resolution.
For women with PCOS, that means a more holistic and empowered path forward. For those with other types of hormonal imbalances, it means no longer settling for vague labels and frustrating dead-ends.
Conclusion: Knowing the Difference Empowers You
At the heart of the confusion between PCOS and hormonal imbalance is a bigger truth: women deserve to understand their own bodies. They deserve to know the difference between a general imbalance and a complex syndrome like PCOS. They deserve doctors who listen, tests that dig deeper, and treatments that aim for healing, not just masking symptoms.
Whether you’re navigating irregular cycles, unexplained fatigue, fertility struggles, or any of the other frustrating symptoms of hormonal chaos, know this: your experience is real, and there are answers. It may take time, patience, and a bit of detective work, but clarity is possible. And once you understand what’s going on—whether it’s PCOS or another hormonal issue—you can take the next step toward balance, health, and empowerment.