Our lungs are not only gateways for air — they are gatekeepers for immunity. When oxygen runs low inside the body, we feel its consequences immediately in dizziness, fatigue, or shortness of breath. But new research reveals something far deeper and more unsettling: hypoxia leaves a genetic scar on the very immune cells meant to defend us, weakening our resistance to infections long after the crisis has passed.
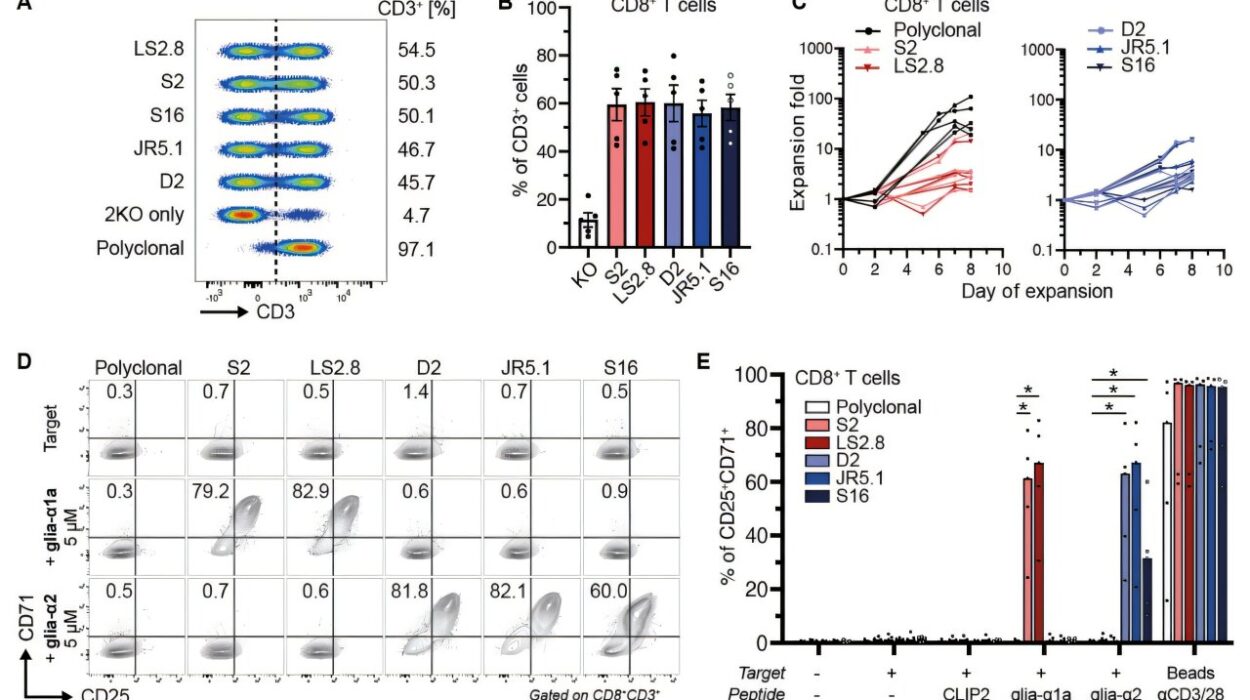
In a study published in Nature Immunology, scientists have shown that even temporary dips in oxygen levels can alter the genetic architecture of neutrophils — frontline immune cells that are built for speed and aggression against microbes. These changes do not fade when oxygen returns. They persist, embedded in the bone marrow factories that continually generate new immune cells, meaning the impact can echo for months or even years after recovery.
When Oxygen Falls, Immunity Falters
Neutrophils act like the immune system’s emergency responders: they rush to the site of an invasion, engulf bacteria, release toxic chemicals, and lay down molecular traps. Their power must be precisely regulated — too strong and they damage healthy tissues; too weak and infection spreads. The new study finds that lack of oxygen tilts this balance toward weakness. Under hypoxic conditions, neutrophils undergo changes in how their DNA is packaged. Certain genes that normally fuel their antimicrobial capability become dampened, dulling their response.
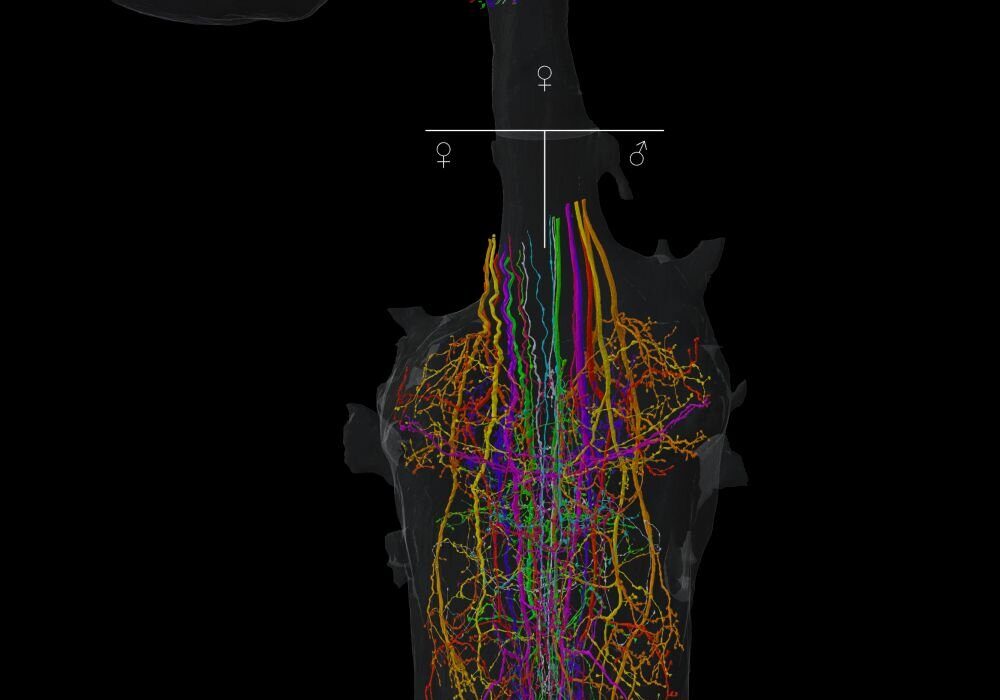
These same genomic changes were found not only in circulating immune cells but also in the precursor cells of the bone marrow that give rise to new neutrophils. That means the body does not just make temporarily weakened immune cells — it begins to manufacture them by default.
A Molecular Memory of Suffocation
The genetic reprogramming detected by the researchers involves histone clipping — a modification to the protein scaffolding that organizes DNA. Histones are like spools around which genetic material is wound; trimming them can expose or conceal genes, switching cellular instructions on or off without altering the underlying DNA sequence. This is a powerful form of epigenetic memory: the cell “remembers” that it once experienced low oxygen and continues to behave as though it is compromised.
This discovery may finally explain a long-standing medical puzzle: why patients recovering from severe respiratory illnesses such as ARDS, or from conditions that chronically limit oxygen like advanced lung disease, remain unusually susceptible to new infections even when their lungs have partially healed. The damage is not only structural — it is immunological and molecular.
Lessons from Illness and Altitude
To test their findings, the University of Edinburgh team examined neutrophils from two groups: patients recovering from acute respiratory distress syndrome, and healthy volunteers exposed to low oxygen at high altitude. Both groups showed the same epigenetic reprogramming, demonstrating that the effect is not restricted to disease — it is a fundamental biological response to oxygen scarcity.
These results recast hypoxia not merely as a symptom or consequence of illness, but as a force that reshapes the immune system’s future behavior. Oxygen deprivation does not simply pause immunity; it rewrites it.
A New Frontier in Treating Post-Illness Vulnerability
The implications are profound. If low oxygen reprograms bone marrow, then recovering patients may carry immunological handicaps long after they leave the hospital. That creates a window of vulnerability — not unlike an open door for future infections. But the discovery also opens a doorway for intervention. If scientists can identify what triggers these epigenetic changes and how to reverse them, it may be possible to restore immune strength in people who today remain fragile months after an illness that deprived them of air.
As Manuel Alejandro Sanchez Garcia, one of the study’s authors, explains, the research does more than diagnose a problem — it reframes long-term immunity: recognizing that low oxygen leaves a lasting imprint on how immune cells read their genetic code clarifies why infection control remains weak long after respiratory recovery. This insight creates new therapeutic targets for rewiring immune function and closing a vulnerability that has until now been invisible.
The Body Remembers More Than We Think
This research deepens a growing realization in medicine: what the body endures is not easily erased. A storm of inflammation, a period of starvation, a burst of radiation, or a lack of oxygen — each leaves a molecular fingerprint that may shape health long into the future. Hypoxia does not merely deprive tissues of breath; it imprints a memory of crisis onto the immune system itself.
The story of this study is ultimately a story about aftermath — about how what threatens us once can continue to weaken us quietly over time. It suggests that to truly understand health after severe illness, medicine must look not only at what has healed on the surface, but at what has been rewritten deep within the cells that guard us.
More information: Hypoxia induces histone clipping and H3K4me3 loss in neutrophil progenitors resulting in long-term impairment of neutrophil immunity, Nature Immunology (2025). DOI: 10.1038/s41590-025-02301-9. www.nature.com/articles/s41590-025-02301-9