For decades, scientists have sought to understand the complex biological roots of autism spectrum disorder (ASD)—a condition that affects how people communicate, interact, and process the world around them. While genetics and brain development are known to play key roles, the precise neurological circuits that drive autism-related behaviors remain difficult to pinpoint.
Now, researchers at Stanford Medicine have uncovered an important piece of the puzzle. By studying brain activity in mice, they identified a small but powerful brain region—the reticular thalamic nucleus (RTN)—that may hold the key to understanding some of the hallmark behaviors of autism.
Even more remarkable, when scientists suppressed the hyperactivity in this brain region, they were able to reverse autism-like behaviors in the mice, raising hope for new treatment strategies in the future.
The Brain’s Gatekeeper
The reticular thalamic nucleus is a thin layer of neurons wrapped around the thalamus, a deep brain structure often described as a relay station for sensory signals. Think of the RTN as a gatekeeper: it regulates the flow of sensory information between the thalamus and the cortex, which is the seat of higher thinking and perception.
When this gatekeeper malfunctions, the brain can become overwhelmed. Sensory information may flood in uncontrollably, leaving individuals hypersensitive to sights, sounds, or touch—a trait often reported in people with autism. Until now, however, the RTN’s role in autism had not been fully understood.
A Window Into the Autistic Brain
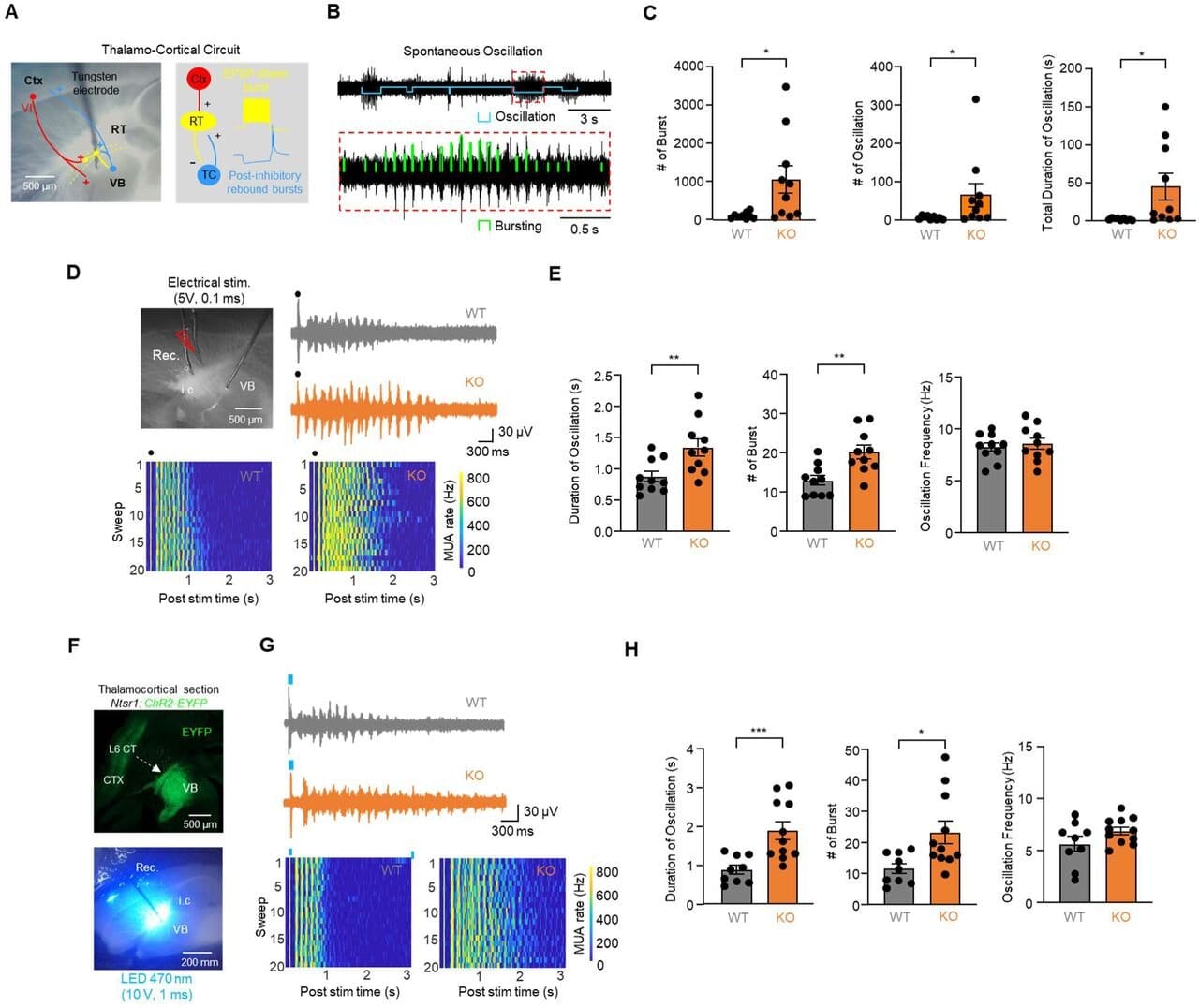
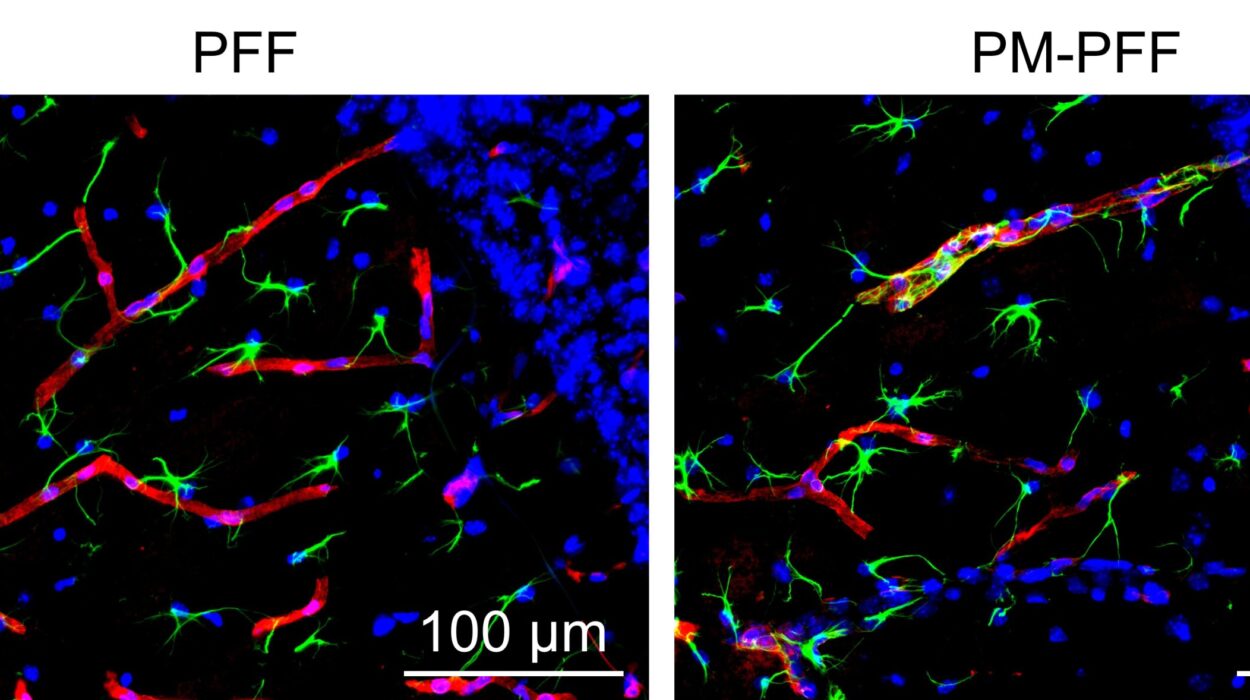
In their new study, published in Science Advances, Stanford researchers monitored the RTN in mice that were genetically modified to mimic autism (known as Cntnap2 knockout mice). These animals displayed behaviors similar to those seen in people with autism, including heightened sensitivity to sensory stimuli, repetitive behaviors, reduced social interactions, and a greater likelihood of seizures.
When the mice were exposed to simple stimuli—such as a flash of light or a puff of air—the RTN lit up with excessive activity. Even during social encounters, this brain region was hyperactive, suggesting that its overexcitement might disrupt the animals’ ability to engage normally. The RTN also produced bursts of spontaneous activity, which triggered seizures.
This finding dovetails with a striking clinical reality: epilepsy affects about 30% of people with autism, compared to just 1% of the general population. The overlap has long been a mystery, but the new study suggests the RTN may be a common link.
Turning Down the Volume
If hyperactivity in the RTN is responsible for these deficits, could calming this brain region improve behavior? The researchers put this question to the test.
They administered an experimental seizure medication called Z944, which dampens activity in the RTN. Astonishingly, the drug not only reduced seizures but also reversed autism-like behaviors in the mice. The animals became less hypersensitive to stimuli, engaged more in social interactions, and showed fewer repetitive movements.
In a second approach, the team used a genetic tool called DREADD-based neuromodulation, which allows scientists to turn neurons “on” or “off” with designer drugs. By dialing down the RTN’s hyperactivity in autistic mice, they restored more typical behavior. Conversely, by ramping up RTN activity in healthy mice, the researchers were able to induce autism-like behaviors.
This provided strong evidence that the RTN is not just involved, but may be a driver of certain autism traits.
A Shared Pathway Between Autism and Epilepsy
One of the most exciting implications of this research is the overlap between autism and epilepsy. Since the same drugs that suppress seizures also eased autism-like symptoms in mice, it suggests that both conditions may arise from similar disruptions in brain circuits.
“This helps explain why epilepsy is so common among individuals with autism,” said study senior author John Huguenard, Ph.D., professor of neurology and neurological sciences at Stanford. “By targeting the RTN, we may be able to address both conditions at once.”
From Mice to Humans: What Comes Next?
While the results are groundbreaking, the research is still at an early stage. The experiments were conducted in mice, and human brains are far more complex. It remains to be seen whether therapies that calm the RTN will have the same effect in people with autism.
Still, the findings open new directions for treatment. Current autism therapies primarily focus on behavioral support and education rather than the brain’s circuitry. By identifying a specific brain region that contributes to autism-related symptoms, scientists may one day design drugs or neuromodulation techniques that directly address the underlying biology.
A Glimpse of Hope
Autism spectrum disorder is deeply varied, with no two individuals experiencing it the same way. There will never be a single “cure,” nor should autism be reduced to something merely to be “fixed.” But understanding the biology behind sensory sensitivity, social challenges, or seizures can help improve quality of life for those who want and need support.
The Stanford study highlights how a deeper look into the brain can reveal not only where things go awry but also where healing might begin. The reticular thalamic nucleus—once an overlooked strip of tissue—has now stepped into the spotlight as a potential key player in the autism-epilepsy connection.
And while much work remains, the discovery offers something precious: a glimpse of hope that science may one day unlock new ways to help people with autism live fuller, more comfortable, and more connected lives.
More information: Sung-Soo Jang et al, Reticular Thalamic Hyperexcitability Drives Autism Spectrum Disorder Behaviors in the Cntnap2 Model of Autism, Science Advances (2025). DOI: 10.1126/sciadv.adw4682