Inside every woman is a finely tuned, endlessly complex symphony—a biological orchestra in which hormones are the conductors. They don’t just direct menstrual cycles or fertility, as often assumed; they orchestrate everything from mood to metabolism, skin clarity to sleep patterns, bone density to brain chemistry. They rise and fall in intricate waves, shifting delicately through the decades, whispering commands to nearly every cell in the body. Hormones are not just chemical messengers; they are the pulse of womanhood, shaping health in invisible yet profound ways.
At the most basic level, hormones are signaling molecules produced by endocrine glands. These messengers travel through the bloodstream, docking at various organs and tissues, instructing them to perform specific tasks. Think of estrogen, progesterone, testosterone, insulin, cortisol, and thyroid hormones as players on a hormonal stage—each one contributing to a larger narrative that defines a woman’s physical, emotional, and mental well-being.
The Teenage Bloom: Hormones Awaken
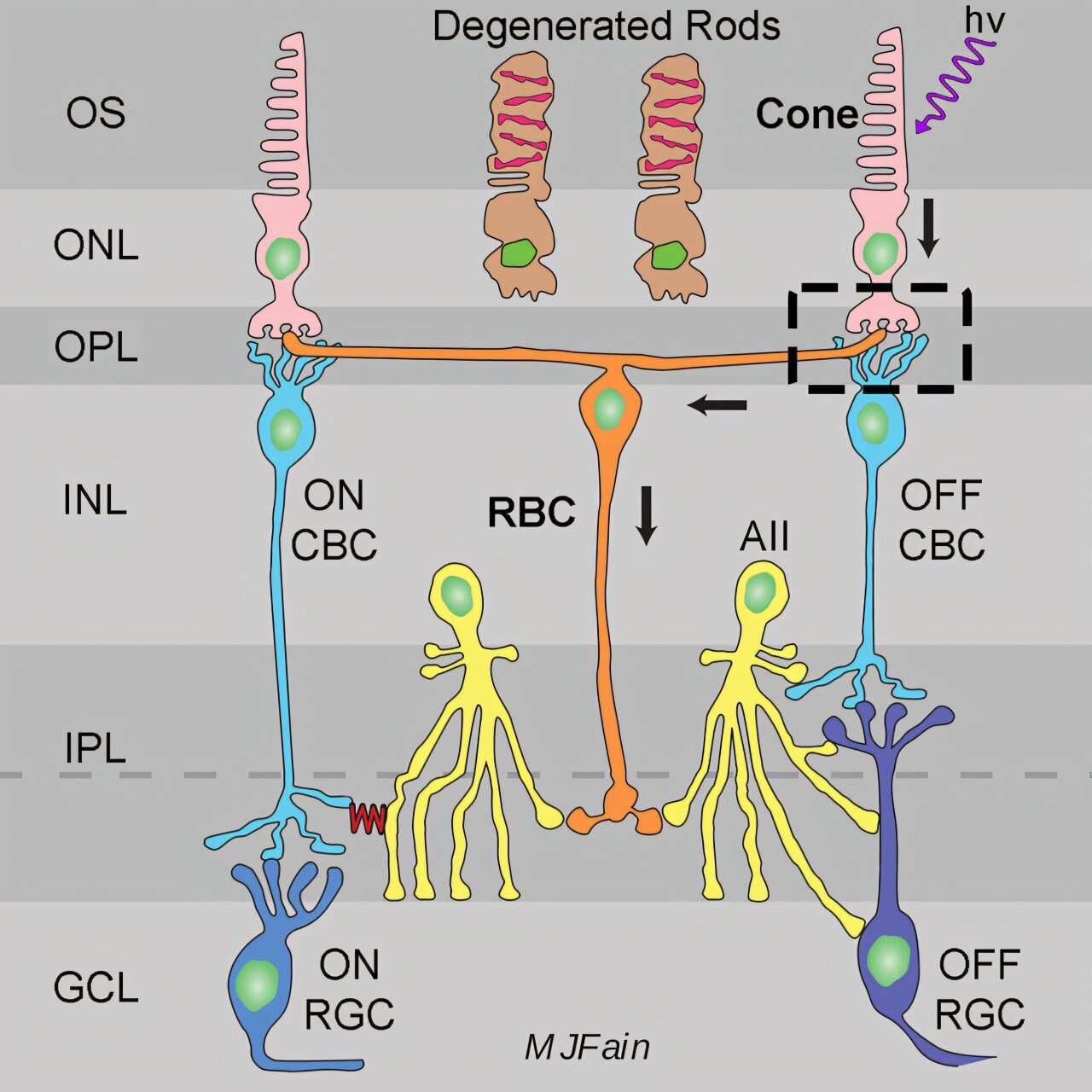
Puberty is the overture to a woman’s lifelong relationship with her hormones. When the hypothalamus in the brain begins to release gonadotropin-releasing hormone (GnRH), it sets off a cascade that activates the ovaries. Estrogen, once barely detectable in childhood, begins to surge, ushering in breast development, body hair, and the beginning of the menstrual cycle. This is not just a physical transformation—it’s a neurological and psychological awakening.
During adolescence, hormonal fluctuations can be tumultuous. The rise and fall of estrogen and progesterone can lead to mood swings, acne, and painful periods. The brain’s reward systems become more sensitive to estrogen, which explains the surge in emotional intensity and the desire for social bonding. It’s no coincidence that many young women begin to experience depression or anxiety for the first time during puberty—hormonal upheaval is not limited to the body.
The adolescent years are also when many young women first encounter the complexity of reproductive health: irregular periods, polycystic ovary syndrome (PCOS), endometriosis, and early signs of hormonal imbalances. Early education and body literacy during this time are essential to helping young women understand and advocate for their hormonal health.
Reproductive Rhythms: The Monthly Cycle of Change
For most of a woman’s life, hormones ebb and flow in a rhythmic, month-long dance. This cycle is more than just menstruation—it is a four-phase process governed by shifts in estrogen and progesterone, and it impacts far more than just the uterus.
The follicular phase begins after menstruation ends. Estrogen levels rise, thickening the uterine lining and preparing the body for ovulation. Women often feel more energized, confident, and mentally sharp during this phase—thanks in part to estrogen’s mood-lifting effects on serotonin.
Ovulation is the high point of estrogen’s influence. The release of an egg from the ovary marks the midpoint of the cycle. Libido often spikes during this time, and many women notice clearer skin and a greater sense of vitality. This is nature’s evolutionary whisper, nudging toward reproduction.
The luteal phase follows ovulation, and progesterone becomes the dominant hormone. While it plays a crucial role in preparing the body for pregnancy, it can also cause bloating, fatigue, and mood changes in some women. If pregnancy does not occur, both estrogen and progesterone levels drop, triggering menstruation and restarting the cycle.
Hormonal fluctuations during the menstrual cycle affect far more than the reproductive system. They influence sleep, appetite, immune function, and even pain tolerance. Women might feel like different versions of themselves week to week, not because they are moody or unstable, but because their biochemistry is actively changing.
Hormones and Mental Health: The Mood Connection
The link between hormones and mental health in women is profound. Estrogen has a direct influence on neurotransmitters like serotonin, dopamine, and norepinephrine—all of which regulate mood. When estrogen levels are high, women often feel happier and more optimistic. But when estrogen plummets, as it does during PMS, postpartum, and perimenopause, mood disorders can arise or worsen.
Premenstrual Syndrome (PMS) and its more severe cousin, Premenstrual Dysphoric Disorder (PMDD), are clear examples of how cyclical hormone changes can disrupt mental health. Women with PMDD experience intense mood swings, depression, irritability, and anxiety during the luteal phase of their cycle. These aren’t just “bad moods”—they are neurochemical reactions to hormonal shifts that can be debilitating.
Postpartum depression is another window into hormonal vulnerability. After childbirth, estrogen and progesterone levels crash dramatically, and for some women, this triggers profound mood changes. Combined with sleep deprivation, identity shifts, and physical recovery, this hormonal cliff can lead to anxiety, depression, and even psychosis.
It’s no accident that women are nearly twice as likely as men to be diagnosed with depression. Hormonal flux plays a significant, often underappreciated role in mental health across a woman’s lifespan.
Fertility, Pregnancy, and the Hormonal Miracle
When a woman becomes pregnant, her body undergoes the most hormonally intense transformation of her life. Human chorionic gonadotropin (hCG), progesterone, estrogen, prolactin, and relaxin flood the system, reprogramming nearly every organ to support new life.
Estrogen and progesterone levels skyrocket, supporting fetal development and reshaping the mother’s body. Blood volume doubles, the immune system is modulated to protect the fetus, and the brain itself changes—shrinking slightly to improve maternal instinct and emotional attunement.
These hormonal changes are not always euphoric. Morning sickness, fatigue, insomnia, and mood swings can be intense. Later in pregnancy, relaxin loosens ligaments in preparation for childbirth but can lead to joint pain and instability. Prolactin prepares the breasts for lactation, while oxytocin plays a starring role in labor and emotional bonding after birth.
Pregnancy also provides unique insight into how hormones shape long-term health. Some women with autoimmune diseases like rheumatoid arthritis find their symptoms disappear during pregnancy, only to return postpartum. Others may develop gestational diabetes or thyroid disorders, revealing latent vulnerabilities triggered by hormonal stress.
Thyroid Health: The Hidden Hormonal Regulator
Often overlooked, the thyroid gland plays a pivotal role in a woman’s hormonal ecosystem. Thyroid hormones regulate metabolism, heart rate, temperature, and energy levels. When thyroid function is off balance—either too slow (hypothyroidism) or too fast (hyperthyroidism)—the entire hormonal system is affected.
Women are up to ten times more likely than men to experience thyroid disorders, especially during times of hormonal upheaval like puberty, pregnancy, and menopause. Symptoms of thyroid dysfunction often mimic other issues: fatigue, weight changes, depression, hair loss, and irregular periods. As a result, many women suffer silently for years before getting a proper diagnosis.
Thyroid hormones also influence fertility. An underactive thyroid can interfere with ovulation, while an overactive one can lead to miscarriages or premature birth. The thyroid’s relationship with the reproductive system is intimate and constant, yet it’s rarely the first place doctors look when women report fatigue or mood changes.
Polycystic Ovary Syndrome: The Hormonal Puzzle
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders affecting women, impacting up to 1 in 10 of reproductive age. It’s a condition of hormonal imbalance characterized by irregular periods, excess androgens (male hormones), and polycystic ovaries.
PCOS is not just a fertility issue; it’s a full-body hormonal disorder with ripple effects across metabolic health. Women with PCOS often struggle with insulin resistance, weight gain, acne, and hair growth in unwanted places. The psychological toll can be severe—anxiety, depression, and body image issues are common.
While the exact cause of PCOS is still not fully understood, it is clear that insulin, testosterone, and inflammation play major roles. Lifestyle changes and medications can help manage symptoms, but because it presents differently in every woman, it often goes undiagnosed or misunderstood.
Perimenopause and Menopause: The Long Goodbye
The transition to menopause—known as perimenopause—is perhaps the most unpredictable hormonal phase of a woman’s life. It can begin in a woman’s 40s, sometimes earlier, and last several years. During this time, estrogen and progesterone levels fluctuate wildly, periods become irregular, and symptoms like hot flashes, night sweats, insomnia, brain fog, and mood swings become common.
This hormonal rollercoaster can feel like a betrayal of the body. One week you feel normal; the next, your skin is dry, your joints ache, and you’re sobbing over a commercial. Sleep becomes elusive, libido plummets, and metabolism slows to a crawl. For many women, perimenopause is more challenging than menopause itself.
When menopause finally arrives—defined as 12 months without a menstrual period—estrogen levels settle at a new, lower baseline. The reproductive years are officially over, but the influence of hormones continues.
Estrogen is a protector—it guards the heart, bones, and brain. After menopause, the risk of osteoporosis, cardiovascular disease, and cognitive decline increases. Understanding this shift is critical to managing long-term health.
Hormones and Sexual Health: More Than Desire
Sexual health is intricately tied to hormones. Estrogen keeps vaginal tissues elastic and lubricated, supports libido, and maintains blood flow to the pelvic region. Testosterone, although often labeled a “male” hormone, plays a key role in female sexual desire and orgasmic function.
During the menstrual cycle, libido tends to rise around ovulation due to increased estrogen and testosterone. After childbirth or during breastfeeding, estrogen levels drop, often resulting in vaginal dryness and discomfort. In menopause, declining hormones can lead to painful intercourse, decreased sensitivity, and loss of libido.
These changes are not just physical—they affect emotional intimacy, self-esteem, and relationships. Yet sexual health in women is often sidelined or stigmatized. Hormone therapy, lubricants, pelvic floor therapy, and open communication can all help women navigate these changes and reclaim their sexual well-being.
The Hormonal Link to Disease and Aging
Hormones are central to many of the chronic conditions that disproportionately affect women. Estrogen plays a dual role in breast cancer—it can both protect against and contribute to its development depending on the context. Conditions like fibroids and endometriosis are also fueled by hormonal imbalances.
Insulin resistance—a key hormonal player in type 2 diabetes—is closely linked to PCOS, weight gain, and inflammation. Cortisol, the stress hormone, disrupts other hormonal systems when chronically elevated, leading to burnout, poor sleep, and impaired immunity.
Even aging itself is shaped by hormones. As estrogen declines, collagen production slows, skin loses elasticity, and bones become fragile. Muscle mass and metabolic rate decrease. But aging does not have to be synonymous with decline. Lifestyle choices, diet, exercise, stress management, and hormone therapy can all support vibrant health well into the golden years.
Balancing the Scales: Supporting Hormonal Health
Hormonal balance doesn’t mean flatlining your levels; it means achieving a dynamic equilibrium that supports your life stage, needs, and goals. Nutrition plays a foundational role—healthy fats, fiber, antioxidants, and phytoestrogens can help regulate estrogen and reduce inflammation. Exercise helps balance insulin and cortisol while boosting mood-enhancing endorphins. Sleep is non-negotiable; even one night of poor rest can throw off your entire hormonal rhythm.
Stress management is perhaps the most underestimated tool for hormonal health. Chronic stress elevates cortisol, disrupts the menstrual cycle, and impairs thyroid function. Practices like mindfulness, yoga, and deep breathing are not indulgences—they are biochemical interventions.
Functional medicine, bioidentical hormones, and holistic approaches offer new pathways to understanding and treating hormonal imbalances. But the most important step is awareness. When women understand how their bodies work, they become powerful advocates for their health.
Conclusion: Your Hormones, Your Power
Hormones are not villains to be battled or mysteries to be feared. They are exquisite, complex, and powerful forces that shape every facet of a woman’s health. From puberty to menopause and beyond, they act as both mirrors and messengers, revealing what the body needs and when.
Women deserve more than the outdated trope of being “hormonal.” They deserve respect for the physiological complexity they live with every day. They deserve healthcare that listens, education that empowers, and tools that help them thrive.
To understand your hormones is to understand your power. And in that understanding lies the key to vitality, balance, and lifelong well-being.