When a person loses a limb, the body visibly changes, but the mind often refuses to let go. Amputees frequently describe a haunting sensation: an itch in a missing hand, pain in an absent foot, or the urge to flex fingers that are no longer there. This phenomenon, known as phantom limb sensation, has puzzled scientists and doctors for centuries. How can the brain insist on feeling a limb that no longer exists?
For decades, neuroscientists believed they had the answer. The dominant theory argued that once a limb was amputated, the brain would reorganize itself, allowing neighboring regions to take over the “silent” territory that once corresponded to the lost limb. For example, since the area of the brain that processes the face sits near the hand region, scientists assumed that after amputation, the face map would spread into the hand’s territory.
But now, new research from scientists in the UK and US is rewriting that story. Their findings, published in Nature Neuroscience, suggest that the brain’s body map is far more stable—and stubborn—than we ever realized.
The Brain’s Map of the Body
Inside the brain lies the somatosensory cortex, a strip of tissue that contains a remarkable map of the human body. Each region corresponds to a specific body part: the toes, the fingers, the lips. This map doesn’t look like the body we see in a mirror. Instead, it is distorted, with large areas devoted to sensitive regions like the hands and face, and smaller areas to less sensitive parts like the back.
This “map” guides how we experience touch, temperature, pain, and even our sense of where the body is in space. If you burn your finger, a precise spot in the somatosensory cortex lights up. If you stub your toe, a different spot activates. The brain, in essence, is constantly redrawing our bodily experience in real time.
But what happens to that map when part of the body disappears? That has been the enduring mystery.
A Long-Held Assumption: The Brain Rearranges Itself
The prevailing wisdom held that after amputation, the brain’s map reorganizes itself. Without input from the missing limb, neighboring regions are thought to expand and “invade” the now-unused area. This idea seemed to explain phantom sensations: perhaps the brain was being “confused” by overlapping signals.
Yet this view carried contradictions. If the brain had truly erased the hand from its map, why did amputees still feel their fingers? And why, when asked to imagine moving their missing hand, did brain scans reveal activity that looked remarkably similar to that of people with intact hands?
The answers, it turns out, required a closer look—not just at the aftermath of amputation, but at what the brain looked like before.
A Groundbreaking Experiment
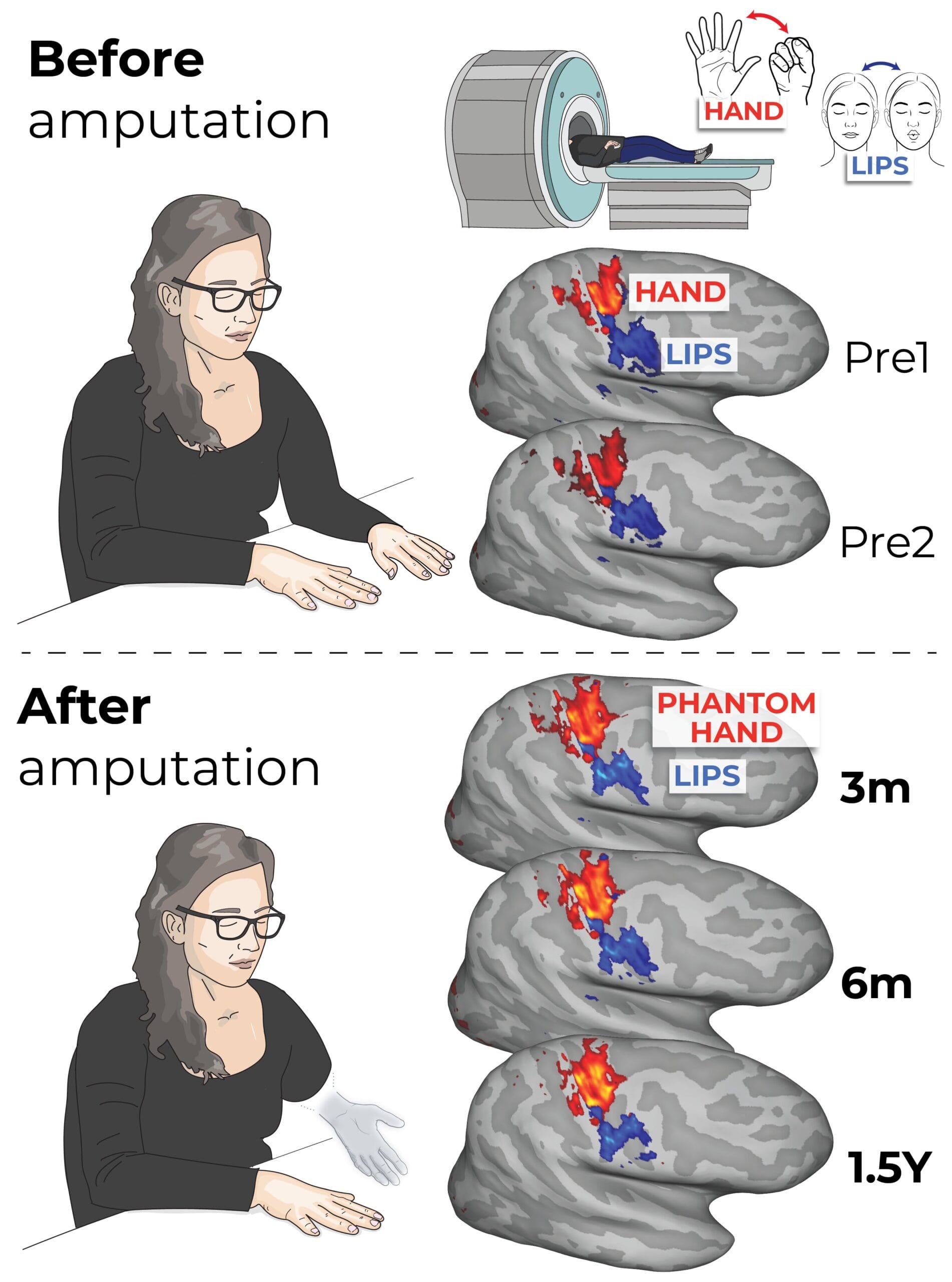
A team led by Professor Tamar Makin of the University of Cambridge and Dr. Hunter Schone of the University of Pittsburgh designed an ambitious study. For the first time, they scanned the brains of individuals both before and after amputation.
Three patients awaiting hand amputations due to medical reasons were recruited. Before surgery, while lying inside an fMRI scanner, they were asked to move their fingers one by one and to purse their lips. This allowed researchers to build a detailed map of how each participant’s brain represented their hand and face.
Then, months after the amputations, the participants returned. This time, they were asked to purse their lips again and to imagine moving their missing fingers. The scans revealed something astonishing: the brain maps of the hands remained nearly identical to those from before amputation. Even years later, the “ghost” of the hand lingered in the brain, untouched by the loss of the limb.
Professor Makin described the result as “jaw-dropping.” The brain’s representation of the missing hand had not faded, and the neighboring face map had not encroached. The once-assumed reorganization simply wasn’t happening.
The Persistence of Phantom Limbs
This discovery helps explain why phantom limb sensations are so vivid. The brain still carries a complete and active blueprint of the missing body part. It continues to “light up” as though the limb were still attached. The brain doesn’t seem to know—or perhaps refuses to accept—that the hand is gone.
For amputees who live with phantom pain, this insight offers both comfort and challenge. Comfort, because the pain isn’t “imaginary”—it’s rooted in real, persistent brain activity. Challenge, because it means traditional treatments aimed at “retraining” the brain’s maps may be addressing the wrong problem altogether.
Why the Old Model Was Wrong
Why did earlier studies suggest reorganization? The answer lies in how those experiments were designed. Many relied on stimulating the body after amputation and using a “winner takes all” approach: whichever part activated a brain region most strongly was assumed to “own” it.
But brain maps are not cleanly divided. Signals from one finger often spill into the region of another. Without the hand present to provide its input, neighboring signals appeared stronger, leading researchers to mistakenly conclude they had taken over. The new study shows that the underlying map remains intact—it’s just waiting, silently, for its lost partner.
A New Path for Treatment
The findings carry profound implications for how we treat phantom limb pain and how we design future prosthetics.
Phantom limb pain arises not because the brain map is gone, but because severed nerves in the residual limb continue to send disorganized, noisy signals. Without their natural targets—the muscles, skin, and receptors of the hand—these nerves misfire. This storm of signals creates the painful illusion of a missing hand in distress.
Some of the most promising treatments now involve surgical innovations, such as grafting the nerves into nearby muscles or skin, giving them new “homes” and reducing chaotic firing. One of the participants in the study who underwent this type of procedure reported that her pain disappeared entirely.
A Hopeful Future for Prosthetics
The research also suggests exciting possibilities for advanced prosthetics. If the brain’s hand map survives intact, then in theory, a robotic hand controlled by neural interfaces could be mapped seamlessly onto it. The brain doesn’t need to “learn” a new system—it still remembers the old one.
As Dr. Chris Baker of the National Institutes of Mental Health explained, “If the brain rewired itself after amputation, these technologies would fail.” But since the maps remain stable, brain-computer interfaces can tap directly into them, potentially restoring movement and sensation in unprecedented ways.
Imagine a prosthetic hand not only moving on command but also relaying texture, shape, and temperature back to the brain—allowing an amputee to feel a warm cup of coffee, the smoothness of glass, or the softness of fabric. That future is now closer than ever.
The Brain That Refuses to Forget
What this research ultimately reveals is the stubborn loyalty of the human brain. Even when the body is altered, the mind holds onto its blueprint, as though refusing to accept loss. The hand may be gone, but in the silent folds of the cortex, it endures.
This resilience may be frustrating for those living with phantom pain, but it is also profoundly hopeful. It means the self is never truly erased; it waits, dormant, for reconnection.
As Dr. Schone reflected, “Now that we’ve shown these maps are stable, we can move into the next frontier—restoring the rich, qualitative aspects of sensation. Even after limb loss, the brain holds onto the body, waiting for us to reconnect.”
More information: Schone, HR et al. Stable Cortical Body Maps Before and After Arm Amputation, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-02037-7