Diabetes is not merely a condition defined by blood sugar levels; it is a silent storm that reshapes lives, influences health in ways seen and unseen, and often leaves women uniquely vulnerable. While the disease affects both men and women, the challenges it poses to women’s health are distinct, profound, and at times, life-altering. For millions of women worldwide, diabetes intertwines with hormonal changes, reproductive health, pregnancy, and long-term risks such as heart disease and osteoporosis.
To understand diabetes in women is to uncover a story of resilience, biology, and empowerment—a story where knowledge can save lives and where prevention and care can transform futures. This article will take you on a comprehensive journey into the science of diabetes, its unique risks for women, the pathways of prevention, and the strategies for blood sugar control that empower women to live not just longer but healthier lives.
What Is Diabetes?
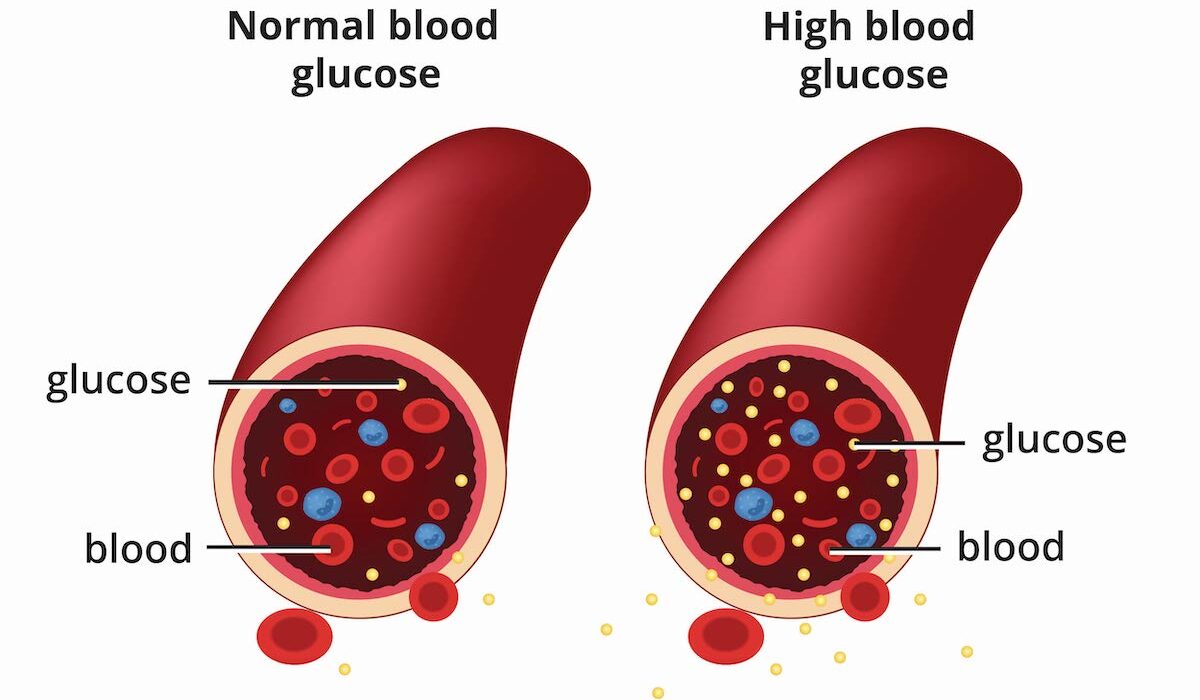
At its core, diabetes is a metabolic disorder characterized by elevated blood glucose levels. It results from either insufficient production of insulin, ineffective use of insulin by the body’s cells, or a combination of both. Insulin, produced by the pancreas, acts as the key that unlocks cells to allow glucose—derived from food—to enter and provide energy. Without proper insulin function, glucose accumulates in the blood, leading to hyperglycemia.
There are several types of diabetes:
- Type 1 diabetes, an autoimmune condition where the body’s immune system attacks insulin-producing beta cells in the pancreas.
- Type 2 diabetes, the most common form, where the body becomes resistant to insulin or does not produce enough.
- Gestational diabetes, which develops during pregnancy but increases the risk of type 2 diabetes later in life.
Though men and women can develop any of these, the impact on women’s health often carries unique complications, particularly in reproductive and cardiovascular health.
Why Women Face Unique Risks
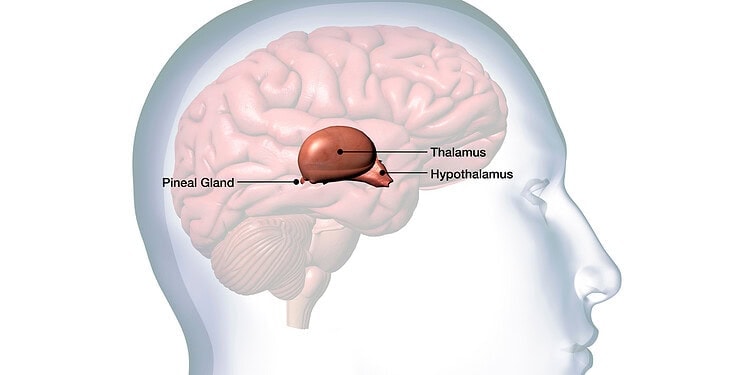
Women live in bodies guided not just by glucose and insulin but also by the ebb and flow of hormones such as estrogen and progesterone. These hormones influence how glucose is metabolized, how fat is stored, and how insulin works. This biological difference partly explains why women often experience diabetes differently than men.
For instance, fluctuations in hormones during menstrual cycles can affect insulin sensitivity, making blood sugar control more complicated. Pregnancy can further complicate this balance, while menopause often leads to weight gain and increased insulin resistance. Beyond hormones, social and cultural factors also play a role—women may face greater barriers to healthcare access, or may prioritize family care over self-care, delaying diagnosis or treatment.
The result is a health landscape where diabetes in women requires tailored attention and deeper understanding.
The Hidden Face of Type 2 Diabetes in Women
Type 2 diabetes often develops silently. Many women live with undiagnosed diabetes for years, experiencing symptoms that can be subtle or mistaken for other conditions: fatigue, increased thirst, frequent urination, blurred vision, or slow-healing wounds. By the time diagnosis occurs, complications may already have begun.
Women with type 2 diabetes face nearly double the risk of heart disease compared to men with the same condition. They also face a higher likelihood of developing complications such as kidney disease, eye damage, and neuropathy. In addition, polycystic ovary syndrome (PCOS), a common hormonal disorder in women, increases the risk of insulin resistance and type 2 diabetes, often affecting women in their reproductive years.
Gestational Diabetes: A Double Burden
Pregnancy is often described as a miraculous transformation, but for many women it also brings hidden risks. Gestational diabetes develops when pregnancy hormones interfere with the body’s ability to use insulin effectively. This condition usually resolves after birth, but its consequences ripple far beyond pregnancy.
Women who develop gestational diabetes are at increased risk of complications such as high blood pressure, preeclampsia, and the need for cesarean delivery. Babies born to mothers with gestational diabetes may be larger than average, face birth complications, or have an increased risk of obesity and type 2 diabetes later in life. For the mother, the condition signals a significantly higher chance of developing type 2 diabetes in the future.
This dual impact—on mother and child—makes gestational diabetes a crucial area where prevention, monitoring, and timely intervention can change outcomes for generations.
Diabetes, Hormones, and Women’s Bodies
The intricate relationship between diabetes and women’s hormones cannot be overstated. Throughout a woman’s life, hormonal shifts intersect with glucose metabolism in complex ways:
- Menstrual cycles often cause fluctuations in blood sugar, with some women experiencing higher levels before menstruation due to progesterone-related insulin resistance.
- Pregnancy alters metabolism to support fetal development, but also challenges insulin function, sometimes tipping the balance into gestational diabetes.
- Menopause brings declining estrogen levels, which often lead to weight gain, abdominal fat accumulation, and increased insulin resistance—all factors that exacerbate diabetes risk.
These transitions highlight why diabetes care for women cannot be one-size-fits-all; it must be adapted to each life stage, with sensitivity to the unique biological realities women face.
Long-Term Complications in Women with Diabetes
The complications of uncontrolled diabetes are serious for all people, but they strike women with particular severity. Cardiovascular disease is the leading cause of death in women with diabetes, and the risk is greater than in men with the condition. Stroke, heart attacks, and peripheral vascular disease occur more frequently and often with worse outcomes.
Beyond the heart, diabetes can affect:
- Kidneys, leading to chronic kidney disease or even kidney failure.
- Eyes, causing retinopathy, cataracts, and blindness.
- Nerves, resulting in neuropathy that causes pain, tingling, or numbness, particularly in the feet.
- Bones, increasing the risk of osteoporosis and fractures.
- Reproductive health, leading to irregular cycles, fertility challenges, and complications during pregnancy.
For women, these complications are not only medical but deeply personal—affecting quality of life, independence, and emotional well-being.
Emotional and Mental Health Dimensions
The story of diabetes in women is not only physiological but also psychological. Living with a chronic condition requires constant vigilance: checking blood sugar, planning meals, monitoring medications. This burden often leads to stress, anxiety, and depression.
Women may experience a greater emotional toll due to social expectations of caregiving and perfection, which can exacerbate feelings of guilt or inadequacy when blood sugar control feels elusive. Stigma around weight and body image, often linked with type 2 diabetes, adds another layer of emotional strain.
Understanding these mental health dimensions is essential, because effective diabetes care must nurture both body and mind.
Prevention: Building a Shield Against Diabetes
The good news is that diabetes—particularly type 2 and gestational diabetes—can often be prevented or delayed. Prevention is not about perfection but about building habits that empower women to protect their health.
Regular physical activity, balanced nutrition, weight management, and stress reduction form the foundation of prevention. For women at risk due to PCOS, family history, or prior gestational diabetes, early screening and lifestyle adjustments are critical.
Preventive care also involves routine check-ups, blood glucose testing, and conversations with healthcare providers about risk factors unique to women. Knowledge becomes a shield—arming women with the tools to make informed choices that protect their future.
Nutrition and Women’s Blood Sugar Control
Food is not only fuel but also medicine. For women with diabetes, nutrition plays a central role in managing blood sugar and reducing complications. A diet rich in whole grains, lean proteins, vegetables, fruits, and healthy fats supports stable glucose levels. Portion control and mindful eating prevent spikes and crashes.
Women often face cultural and practical barriers in this arena—managing family meals, navigating social expectations, or juggling busy schedules. Yet small, consistent changes—choosing water over sugary drinks, adding fiber-rich foods, or preparing balanced snacks—can make a profound difference.
It is not about deprivation but empowerment—discovering how food choices can strengthen, rather than weaken, health.
Physical Activity: The Body’s Natural Medicine
Exercise is one of the most powerful tools for blood sugar control. Physical activity increases insulin sensitivity, helps regulate weight, and strengthens the heart. For women, exercise also boosts bone density, improves mood, and reduces stress—factors especially important across life stages such as menopause.
Activities need not be extreme. Brisk walking, cycling, yoga, or even dancing in the living room can provide benefits. What matters most is consistency and finding joy in movement. When exercise becomes a celebration of what the body can do, rather than a punishment for what it cannot, it transforms into a sustainable part of life.
Medical Care and Women-Centered Treatment
Effective diabetes care requires more than medication—it requires care tailored to women’s unique needs. This includes reproductive counseling, pregnancy planning, menopause management, and attention to mental health.
Medications such as metformin, insulin, or newer therapies like GLP-1 receptor agonists play a critical role, but they must be combined with lifestyle support and personalized monitoring. Women also benefit from education about how medications may interact with hormonal changes or pregnancy.
Healthcare systems must listen to women, not dismiss their concerns, and provide culturally sensitive, gender-specific care that addresses both physical and emotional dimensions.
The Role of Community and Support
No woman should face diabetes alone. Community—whether through family, friends, peer groups, or online networks—provides strength, encouragement, and accountability. Support systems reduce isolation, empower women to share strategies, and remind them that their struggles are not theirs alone.
Healthcare professionals, too, form part of this community, offering guidance and compassion. Together, these networks transform diabetes from an isolating burden into a shared journey.
Research and the Future of Women’s Diabetes Care
The future of diabetes care for women is bright with possibilities. Advances in continuous glucose monitoring, wearable technology, and artificial intelligence are making blood sugar management more precise and less intrusive. Personalized medicine—tailored to genetics, lifestyle, and hormones—promises to revolutionize prevention and treatment.
Research is increasingly recognizing the importance of studying sex differences in diabetes. By understanding how diabetes uniquely affects women, science can develop strategies that are more effective, inclusive, and compassionate.
Conclusion: Empowering Women Through Knowledge and Care
Diabetes is not just a condition—it is a crossroads where biology, lifestyle, and society intersect. For women, it brings unique challenges, from reproductive health to long-term complications, but also unique opportunities for prevention and empowerment.
By understanding the risks, embracing prevention, and mastering blood sugar control, women can rewrite the story of diabetes. They can transform fear into resilience, uncertainty into knowledge, and vulnerability into strength.
Every woman deserves not just to survive with diabetes but to thrive. With science, compassion, and empowerment, the silent storm of diabetes can be weathered, and women everywhere can reclaim their health and their future.