Deep within the chest, millions of tiny, grape-like clusters called alveoli perform the silent miracle of life. These air sacs serve as the essential gateway where oxygen enters the blood and carbon dioxide departs, but they also stand as a fragile front line. They are the barrier against every inhaled virus and bacteria, the site of a microscopic war between the human body and invaders like the flu or tuberculosis. For years, scientists have struggled to watch this battle unfold in real-time, but a team of researchers at the Francis Crick Institute, in collaboration with AlveoliX, has now succeeded in shrinking this vast biological battlefield onto a single, plastic chip.
This is not just any laboratory model; it represents the first human lung-on-chip created using stem cells taken from only one person. In the past, these devices were a patchwork of biology—constructed from a mixture of patient-derived cells and commercially available ones. This “Frankenstein” approach meant the chips could never truly replicate how a specific individual’s body might handle a disease. By ensuring every cell on the chip is genetically identical, researchers have moved closer to a future of personalized medicine, where a patient’s own biology can be tested for its unique vulnerabilities and strengths before a single pill is ever swallowed.
The Breath of Life in a Miniature World
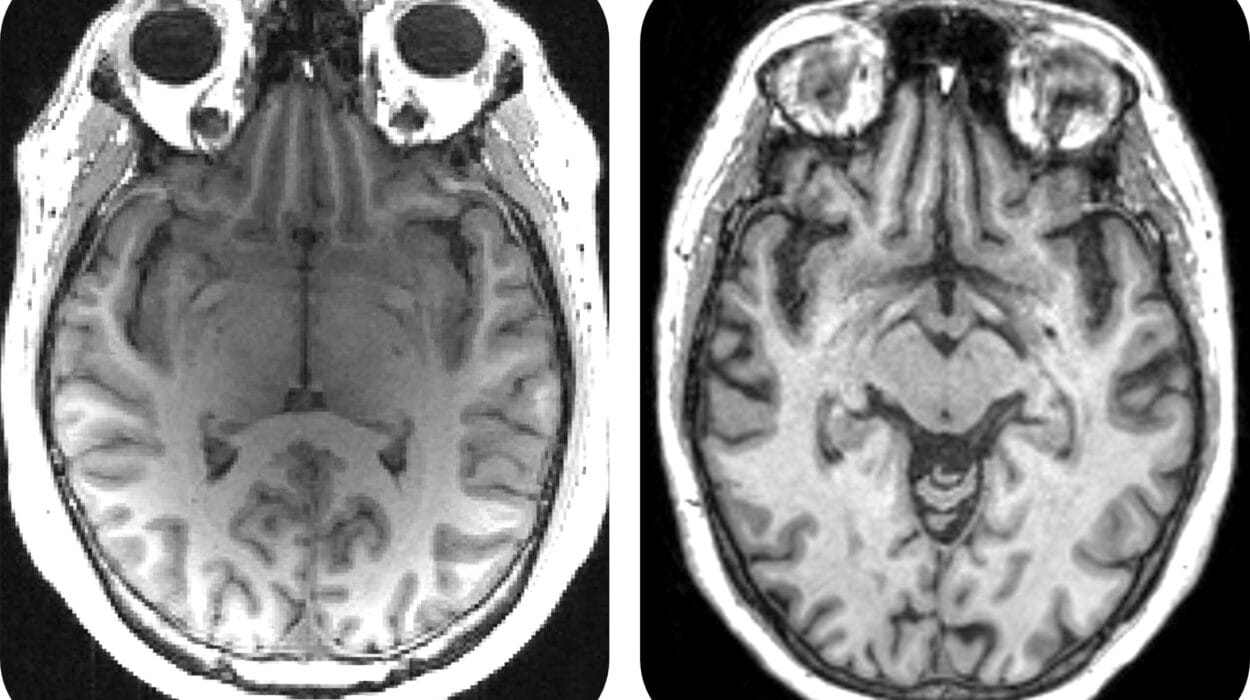
To build this miniature lung, the team turned to the incredible potential of human-induced pluripotent stem cells. These are biological master keys, capable of transforming into virtually any cell in the human body. Using a specific protocol developed in their lab, the researchers guided these stem cells to become the specialized building blocks of the lung: type I and II alveolar epithelial cells, which form the lining of the air sacs, and vascular endothelial cells, which make up the tiny blood vessels.
These cells were then carefully arranged on a incredibly thin membrane within a device designed by the biotechnology company AlveoliX. One side of the membrane represented the air-filled space of the lung, while the other represented the blood-filled vessels. But a lung that does not move is not a lung at all. To truly simulate the human experience, AlveoliX developed specialized machines that impose rhythmic, three-dimensional stretching forces on the barrier. This mimics the physical expansion and contraction of breathing.
This mechanical “breath” turned out to be more than just a visual simulation; it fundamentally changed how the cells behaved. Under the influence of these stretching forces, the cells began to develop microvilli. These tiny, finger-like projections increase the surface area of the lung, a key feature of healthy alveolar cells. By recreating the physical environment of the chest, the scientists didn’t just build a model of a lung; they coaxed the cells into acting as they would inside a living, breathing human being.
The First Salvo of an Invisible War
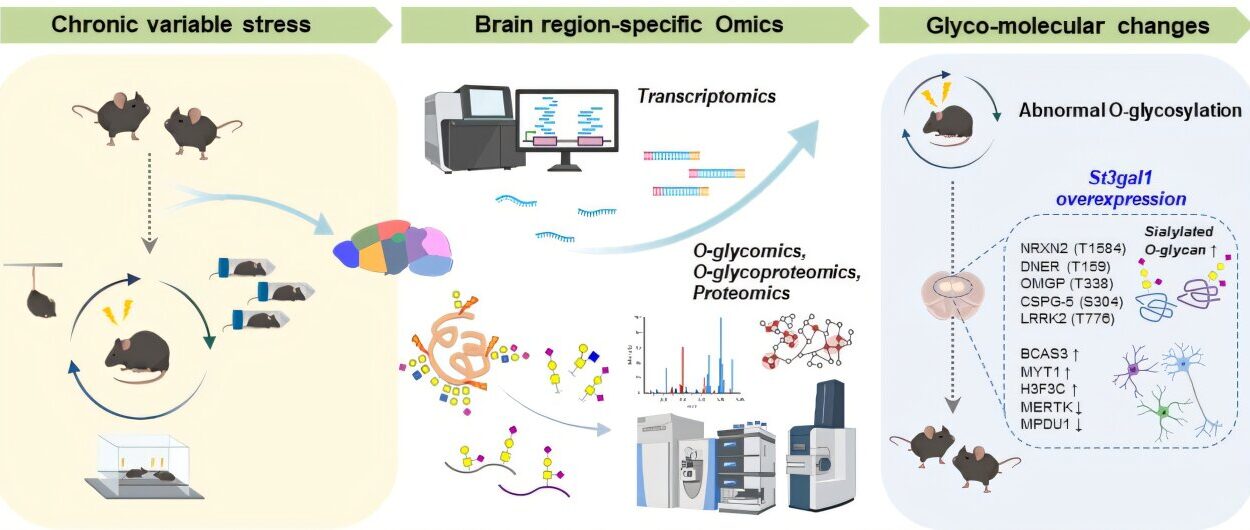
Once the architecture of the lung was established, the researchers introduced the soldiers of the immune system: macrophages. These immune cells were also grown from the same donor’s stem cells, ensuring that the entire system remained genetically unified. With the stage set, the team introduced the enemy—the bacteria that causes tuberculosis, or TB.
TB is a notoriously patient killer. It moves slowly, often hiding within the body for months before the first cough or fever appears. Because of this slow progression, the very earliest moments of infection have long remained a mystery to doctors. “TB is a slow-moving disease, with months between infection and the development of symptoms, so there’s an increasing need to understand what’s happening in the unseen early stages,” explains Jakson Luk, Postdoctoral Fellow at the Crick and the study’s first author.
By watching the chip, the researchers were able to witness the infection’s opening moves. They observed the macrophages rushing to the site of the bacteria, forming large clusters. Within these clusters, a grim transformation took place: necrotic cores began to form. These were groups of dead macrophages in the center of the cluster, surrounded by a ring of living ones. It was a visual representation of the body’s attempt to wall off the infection, a battle that eventually took its toll on the lung itself. Five days after the infection began, the barriers between the epithelial and endothelial cells collapsed. The air sac function had broken down, proving that the chip could accurately mimic the destructive power of the disease.
A Mirror for Human Biology
The success of this genetically unified lung-on-chip marks a significant shift in how we study human health. For a long time, researchers have relied on animal models to understand disease, but animals are not humans. They have different lung anatomies, different immune cell makeups, and their diseases often develop in ways that don’t match our own experience.
Max Gutierrez, Principal Group Leader at the Crick and senior author of the study, emphasizes the necessity of this shift. “Given the increasing need for non-animal technologies, organ-on-chip approaches are becoming ever more important to recreate human systems, avoiding differences in lung anatomy, makeup of immune cells and disease development between animals and humans,” he notes.
By using cells from a single individual, the researchers can now create mirrors of specific people. “Composed of entirely genetically identical cells, the chips could be built from stem cells from people with particular genetic mutations,” Gutierrez says. “This would allow us to understand how infections like TB will impact an individual and test the effectiveness of treatments like antibiotics.” This means that instead of a “one size fits all” approach to medicine, doctors could one day test a variety of drugs on a patient’s “chip” to see which one works best for their specific genetic makeup.
Why This Research Matters
The development of the first single-donor lung-on-chip is a milestone because it offers a holistic, accurate, and human-specific lens through which to view respiratory health. It allows scientists to peer into the “unseen” stages of infection, providing a bridge between the moment a bacterium is inhaled and the moment a person falls ill.
The implications of this work extend far beyond tuberculosis. As Jakson Luk points out, “We were successfully able to mimic these initial events in TB progression, giving a holistic picture of how different lung cells respond to infections. We’re excited that the new model could be applied to a huge range of research, such as other respiratory infections or lung cancer, and we’re now looking at refining the chip by incorporating other important cell types.”
Ultimately, this research matters because it provides a way to study human disease without the limitations of animal models or the inaccuracies of mixed-cell cultures. It brings the complexity of the human body into a controlled laboratory setting, offering a new path for discovering treatments for the world’s most stubborn infections and paving the way for a new era of personalized, individual-focused medicine.
More information: Chak Hon Luk et al, Autologous human iPSC-derived Alveolus-on-Chip reveals early pathological events of M. tuberculosis infection, Science Advances (2026). DOI: 10.1126/sciadv.aea9874. www.science.org/doi/10.1126/sciadv.aea9874