In quiet hospital rooms, across family living rooms dimmed by grief, and within the minds of those who know something precious is slipping away, Alzheimer’s disease writes its story in invisible ink. First comes forgetfulness—harmless, almost laughable. Then comes the repetition, the confusion, the blankness. Finally, recognition fades. A name doesn’t return. A child becomes a stranger. A life becomes a fog.
For decades, this cruel erosion of identity has baffled scientists and broken hearts. Despite extraordinary research efforts, Alzheimer’s remains a stubborn enemy—devastatingly common, poorly understood, and virtually untreatable. Promising drugs have come and gone, many failing in late-stage clinical trials not because they were inherently useless, but perhaps because they were given too late, or to the wrong patients.
But a quiet revolution is underway—one that doesn’t take place under a microscope, but behind the glowing screen of an artificial brain. At the University of Cambridge, researchers have harnessed the power of artificial intelligence to do what humans couldn’t: see the subtle, invisible differences between patients and predict which ones are likely to respond to treatment. In doing so, they may have not only salvaged a previously failed drug trial, but also opened a door into the future of personalized dementia treatment.
The Trial That Failed—Until It Didn’t
Years ago, a clinical trial was conducted for a drug designed to slow cognitive decline in people showing early signs of Alzheimer’s disease. It was a noble endeavor, but the results were disappointing. In the trial’s total population, the drug seemed ineffective. Another promising treatment shelved. Another dead end in a maze already littered with them.
But what if the trial had failed not because the drug was flawed—but because the way it was tested was?
This is the question that Professor Zoe Kourtzi and her team sought to answer. They developed an AI model trained on brain scans, memory tests, and clinical data. What they discovered was as sobering as it was revolutionary: not all Alzheimer’s patients progress in the same way. Some decline rapidly, while others do so slowly—and this difference, invisible to standard clinical assessments, may be the key to unlocking effective treatment.
When the AI re-analyzed the clinical trial data—dividing patients into fast-progressing and slow-progressing groups based on their predicted cognitive decline—a new pattern emerged. In patients with early-stage, slow-progressing mild cognitive impairment, the drug worked. It didn’t cure the disease, but it slowed its relentless march by an impressive 46%. In those patients, the fading of memory, speech, and identity was delayed—bought time, in a race against forgetting.
Reading the Future in Digital Neurons
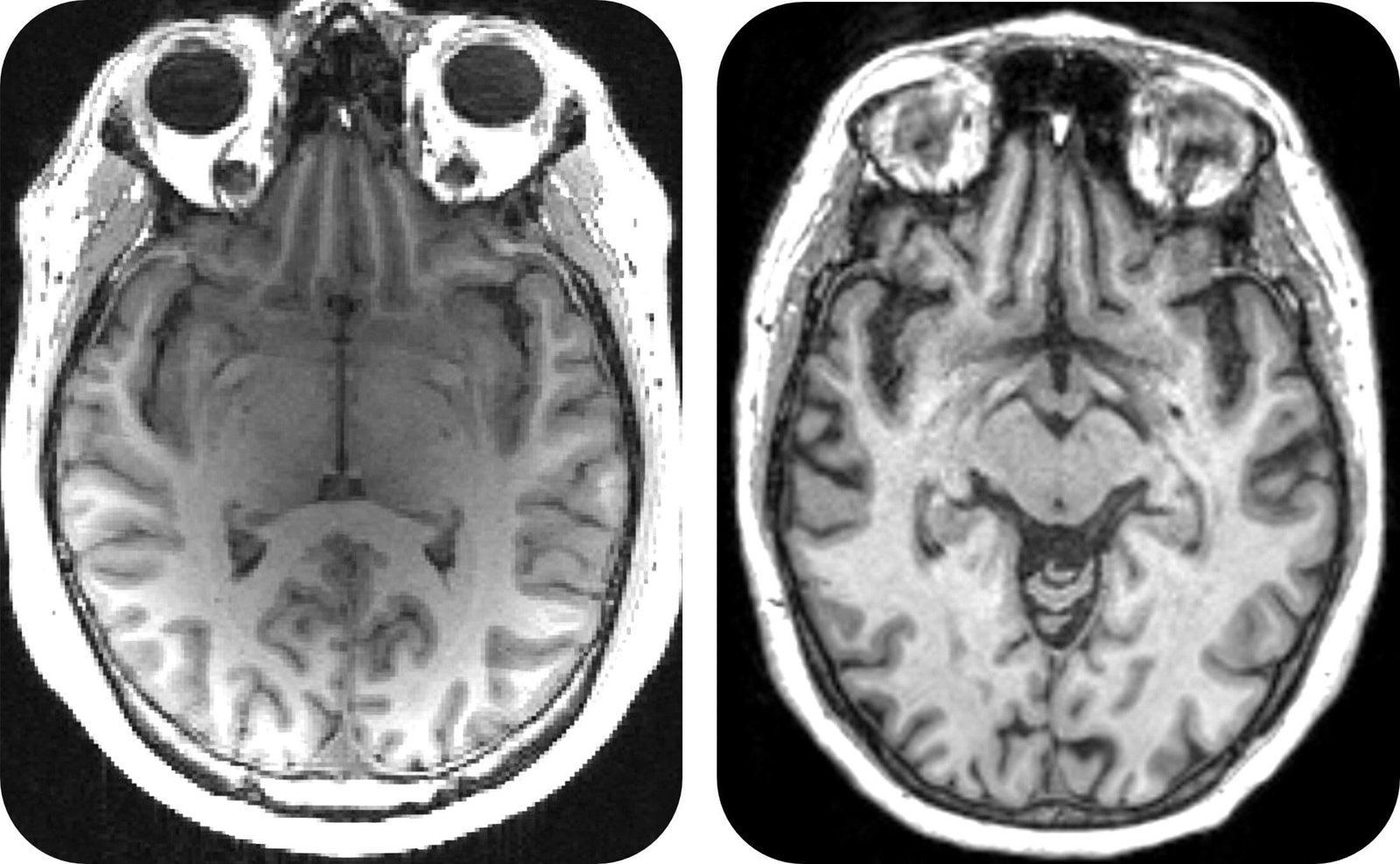
The AI model, developed by researchers in Cambridge’s Department of Psychology, functions like a highly-trained observer, able to detect subtle, early warning signs that would elude even seasoned clinicians. Using inputs from MRI scans, cognitive assessments, and blood biomarkers, the model generates a score predicting how quickly an individual will progress toward full-blown Alzheimer’s disease.
And unlike conventional tools, it is startlingly precise. According to the study published in Nature Communications, the model’s predictions are three times more accurate than those made by human doctors relying on traditional assessments.
This technological leap isn’t just about diagnosis. It’s about timing. “Promising new drugs fail when given to people too late,” explains Kourtzi. “With our AI model, we can finally identify patients precisely and match the right patients to the right drugs.” It’s precision medicine for the brain, and it might be the game-changer the field of dementia research has long awaited.
A Different Kind of Medicine
Most people imagine AI in health care as futuristic machines diagnosing patients or performing robotic surgeries. But what’s unfolding here is more intimate and nuanced. It’s a form of digital intuition—a machine learning from the mistakes of the past to find fragile patterns in the present.
The concept is simple in theory, but revolutionary in application: use AI not just to analyze disease, but to redesign how clinical trials are structured. By segmenting trial participants into subgroups based on how their disease is expected to progress, researchers can test whether a drug truly works in those who can still benefit.
In the case of the re-analyzed Alzheimer’s trial, the drug did what it was designed to do: it cleared beta amyloid from the brain. This sticky protein, which builds up and disrupts brain function, is one of the earliest markers of Alzheimer’s. But clearing it didn’t help everyone—only those whose disease had not yet accelerated beyond a certain threshold.
That nuance had been lost in the original analysis. The entire group had been assessed as one. The result was deemed a failure. But the AI saw what humans couldn’t: the cracks in the population, the quiet distinctions between fast and slow decline. And in doing so, it gave new life to a treatment previously cast aside.
Beyond the Lab: The Human Cost of Delay
To understand the urgency of this development, one must understand the scale of the crisis. Dementia is not a rare affliction. It is the leading cause of death in the UK. Globally, it affects over 55 million people and costs more than $1.3 trillion annually. That number is expected to triple by 2050.
Yet despite this staggering burden, effective treatments remain out of reach. Of the billions spent on research and drug development—over $43 billion by some estimates—the vast majority has yielded disappointment. Clinical trial failure rates hover above 95%, due in large part to the unpredictable nature of the disease and the differences in how individuals respond.
Families live in dread. Patients live in limbo. And even when new drugs are approved—as they have been recently in the United States—they often remain inaccessible due to cost, side effects, or lack of clear benefit.
Kourtzi is all too familiar with this agony. “Like many people, I have watched hopelessly as dementia stole a loved one from me,” she shares. “We’ve got to accelerate the development of dementia medicines. Over £40 billion has already been spent over thirty years—we can’t wait another thirty years.”
Personalized Medicine, Finally Within Reach
One of the most powerful ideas behind this AI approach is personalization. Alzheimer’s disease is not one disease—it’s a spectrum of disorders with overlapping symptoms and varying trajectories. Some patients deteriorate quickly, others slowly. Some respond to drugs, others don’t. Until now, medicine has often treated them all the same.
But with the rise of precision medicine, and now AI-guided patient stratification, that era may be ending.
“This AI-enabled approach could have a significant impact on easing NHS pressure and costs in dementia care,” says Joanna Dempsey of Health Innovation East England. “By identifying which patients are most likely to benefit from treatment, it results in faster access to effective medicines and targeted support for people living with dementia.”
In other words, smarter trials lead to smarter treatments. Fewer side effects. More efficient use of resources. Less time wasted. More lives improved.
Not a Cure, But a Lifeline
It’s important to understand what drugs like the one in this study are—and what they’re not. They are not cures. They do not reverse damage. But they do offer something that, in the world of Alzheimer’s, is precious: time. Time to remember. Time to speak. Time to hold on.
A 46% reduction in cognitive decline doesn’t sound like a miracle, until you consider what it means in real life. It could mean a year longer before a loved one forgets your face. Another season of shared meals. Another birthday celebrated with recognition, not confusion. For patients and families, that is everything.
A New Road Ahead
The AI model developed by Kourtzi and her colleagues is now being adapted for use in clinical care across the NHS. What was once a research experiment is rapidly becoming a real-world tool—one that could change how patients are diagnosed, how drugs are developed, and how lives are lived.
Of course, more work is needed. Larger trials must confirm these findings. Broader datasets must be integrated. Ethical concerns about algorithmic bias and data privacy must be addressed.
But the path is clearer now than it has been in years. By understanding Alzheimer’s not as a single monster, but as a complex, evolving threat that behaves differently in each person, researchers are finally gaining the upper hand.
Memory Reclaimed, If Only for a While
In the end, the war against Alzheimer’s may never be won in a single sweeping moment. But it may be won slowly, one patient at a time, with the right drug at the right moment for the right brain.
AI may not have a heart, but in this case, it has helped us protect what makes us most human: memory, love, and connection.
And that, perhaps, is the greatest medicine of all.
Reference: AI-guided patient stratification improves outcomes and efficiency in the AMARANTH Alzheimer’s Disease clinical trial, Nature Communications (2025). DOI: 10.1038/s41467-025-61355-3