In the global race to cure genetic diseases, gene editing has long been hailed as the miracle scalpel of modern medicine. With the precision of CRISPR-Cas9 and the design flexibility of AAV6 viral vectors, scientists have moved tantalizingly close to correcting the very mutations that lie at the heart of inherited blood disorders. But in a surprising and critical twist, researchers at the San Raffaele Telethon Institute for Gene Therapy (SR-Tiget) in Milan have now uncovered a biological catch: this genetic surgery may prematurely age the very cells it aims to save.
In a groundbreaking study published in Cell Reports Medicine, a team led by Dr. Raffaella Di Micco and Dr. Luigi Naldini has revealed that editing blood-forming stem cells using CRISPR-Cas9 and AAV6 triggers a powerful storm of cellular distress. Rather than quietly correcting a gene mutation and resuming normal function, a significant portion of these stem cells responds by slipping into a senescence-like state—a state of biological limbo that curtails their regenerative powers and potentially undermines the entire therapeutic outcome.
This isn’t just a minor speed bump on the road to gene therapy. It’s a fundamental insight into how sophisticated molecular interventions interact with complex human biology—and a call to rethink how we engineer cells for medicine.
The Gene Editing Dream Meets a Cellular Reality
Gene editing is, in many ways, the ultimate scientific power fantasy: find the flaw in DNA, rewrite it, and fix the disease at its root. In the case of homology-directed repair (HDR)—a strategy that uses a donor DNA template to precisely patch a genetic mutation—the approach has shown enormous promise, especially for hematopoietic stem and progenitor cells (HSPCs).
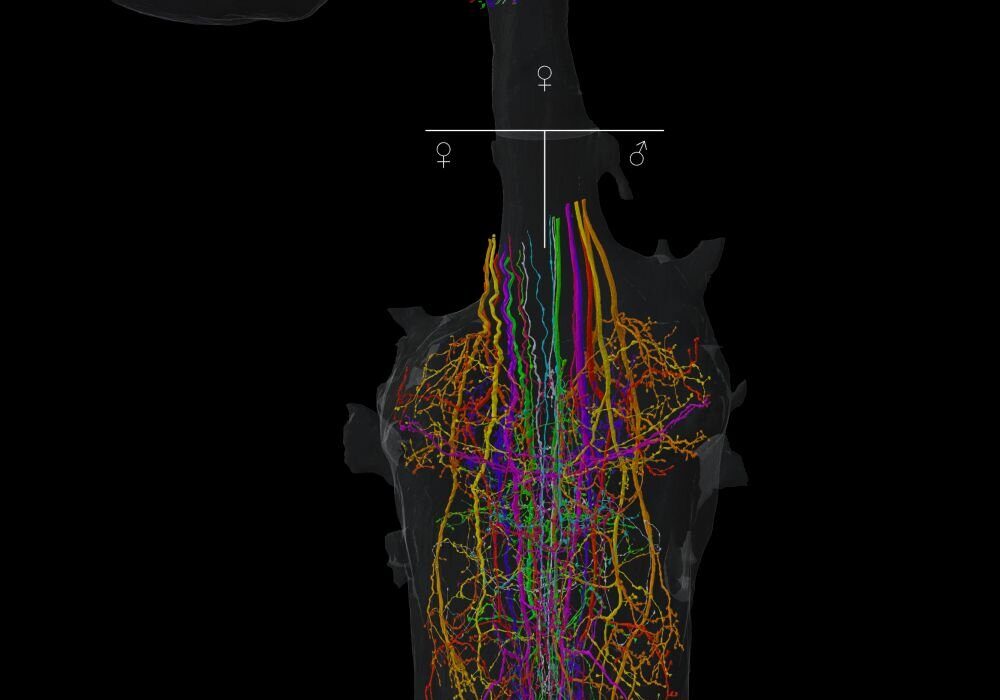
These multipotent cells reside in the bone marrow and are responsible for continuously replenishing all types of blood cells throughout life. For diseases like sickle cell anemia, severe combined immunodeficiency (SCID), or Fanconi anemia, editing these cells could offer a lifelong cure. The logic is simple: fix the DNA in the stem cell, and every new blood cell it produces will carry the corrected version.
But logic often collides with biological nuance.
For years, scientists observed that edited HSPCs often struggled to engraft and expand effectively in preclinical models. The editing itself seemed to dampen their “stemness”—their ability to self-renew and differentiate over time. What was sapping their vitality?
Senescence: The Silent Saboteur
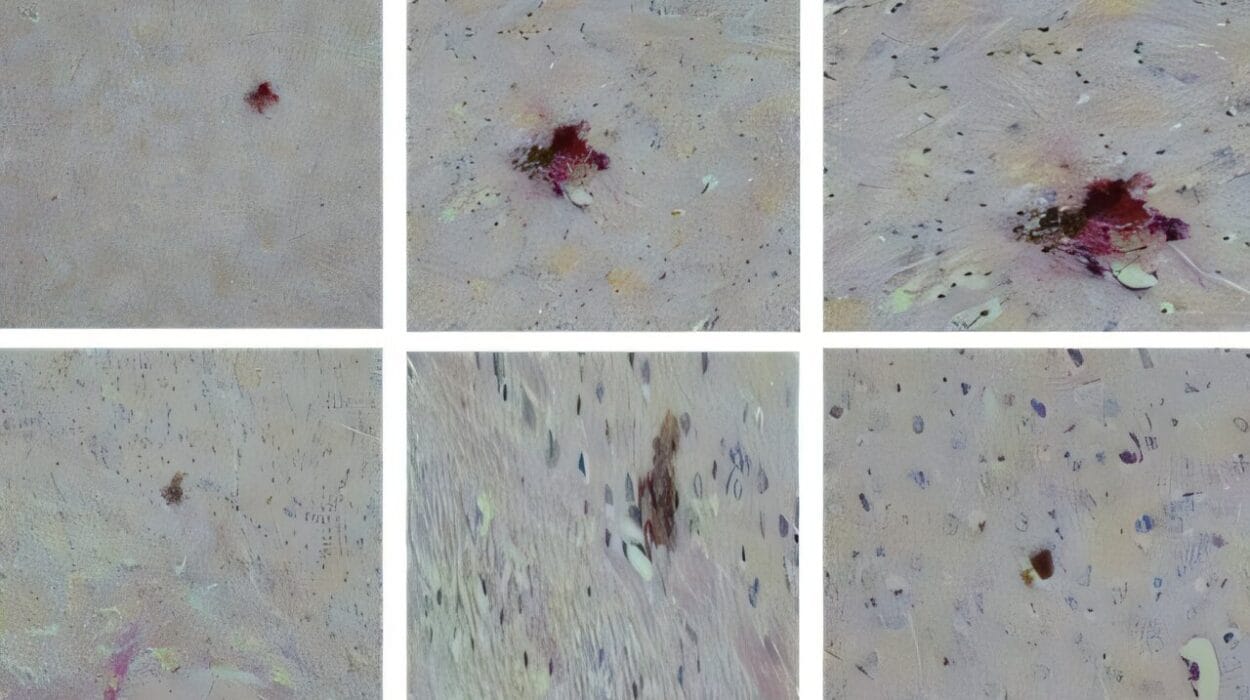
Dr. Di Micco’s team discovered the answer hiding in plain sight: cellular senescence.
Senescence is a kind of biological burnout. Triggered by DNA damage, oxidative stress, or oncogenic signals, it represents the cell’s decision to stop dividing—forever. It’s a protective measure, originally evolved to prevent damaged cells from becoming cancerous. But in the context of gene therapy, it turns out to be a major complication.
Using highly sensitive molecular tools, the SR-Tiget scientists found that CRISPR-Cas9-induced DNA breaks, especially when combined with AAV6 delivery of the DNA repair template, activate two major stress response pathways: p53—the cell’s master damage sensor—and the IL-1/NF-κB inflammatory axis. These pathways, once triggered, act like cellular fire alarms. The result is an HSPC that no longer feels safe to divide. It stays alive but enters a quiescent, inflammation-soaked state—a senescent-like limbo that limits its regenerative potential.
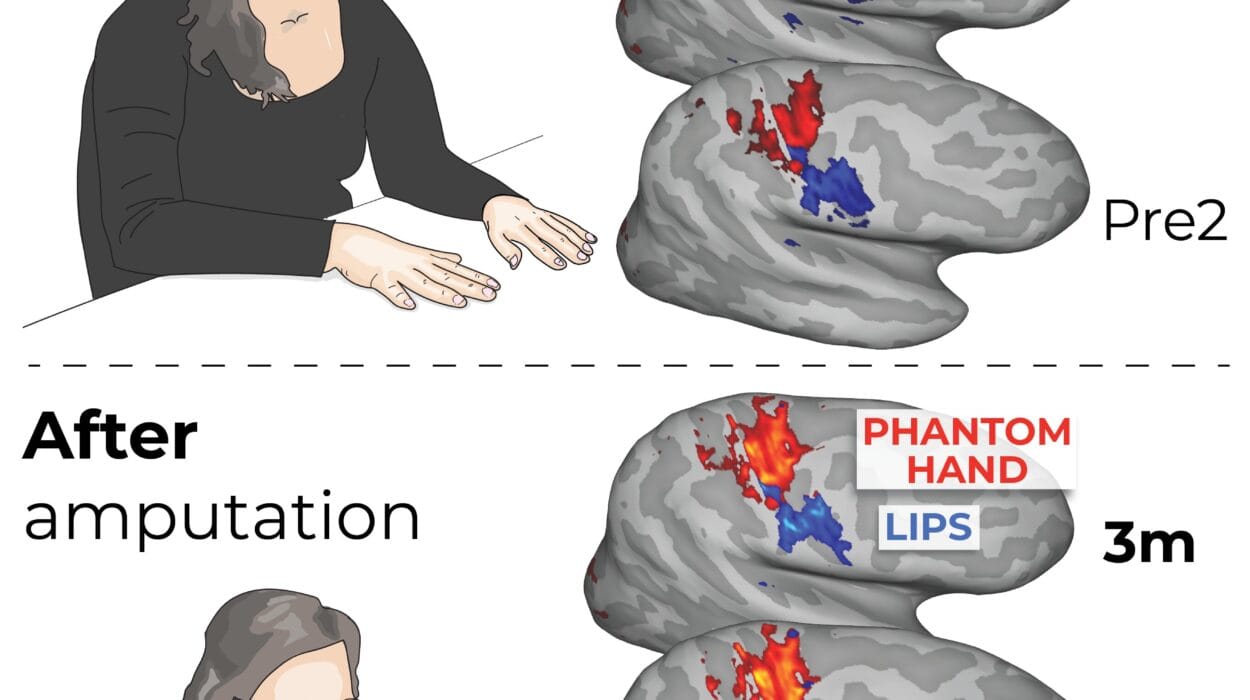
What’s more, these responses weren’t fleeting. As Dr. Anastasia Conti, first author of the study, explains: “We were surprised by the persistence of senescence-like features even months after transplantation. These cells retain a memory of the editing event—it’s not just a temporary stress reaction.”
In other words, these edited cells don’t simply “get over it.” They carry the scars of their reprogramming attempt like a trauma, long after the editing machinery has left the scene.
The Consequences: A Diminished Blood Factory
The implications are significant. In a healthy bone marrow transplant, a relatively small number of donor HSPCs can reconstitute the entire blood and immune system of a recipient. But if a sizable fraction of edited HSPCs become senescent, the transplant’s regenerative capacity becomes bottlenecked. The risk is not just poor engraftment—it’s also a loss of diversity, or oligoclonality, which increases the chance that one rogue edited cell could dominate and potentially acquire further mutations.
For gene therapy to be safe and durable, the edited cells must behave like natural stem cells: robust, regenerative, and long-lived. But senescence throws a wrench into that ideal. The very act of editing—when done aggressively or imprecisely—can make the stem cell less of a stem cell.
The Rescue Plan: Interrupting Inflammation and P53 Signaling
Rather than accept this as an unavoidable trade-off, the researchers went on the offensive.
They designed two complementary strategies to interrupt the senescence cascade: one aimed at temporarily disabling p53, and the other focused on dampening the inflammatory response, specifically via IL-1 signaling.
The p53 approach is not without risks. While inhibiting p53 temporarily allows cells to bypass the immediate DNA damage checkpoint—thereby reducing senescence markers—it can also open the door to uncontrolled cell division and genomic instability. p53, after all, is one of the cell’s most powerful tumor suppressors.
The more promising option turned out to be Anakinra, a clinically approved IL-1 receptor antagonist already used to treat rheumatoid arthritis and autoinflammatory syndromes. By blocking IL-1, the team was able to significantly reduce senescence features in edited HSPCs—without increasing genotoxic side effects. In fact, Anakinra appeared to offer a double benefit: it not only preserved stem cell function but also reduced the frequency of large DNA deletions and chromosomal translocations that sometimes arise after editing.
As Dr. Conti noted: “Anakinra provides a safer profile than p53 inhibition. It suppresses the inflammatory signals without tampering with the core DNA damage response machinery.”
The result? Edited stem cells that looked and behaved much more like their unedited counterparts—able to engraft, regenerate, and populate the blood system with diverse and healthy lineages in long-term animal models.
Redesigning the Blueprint for Gene Therapy
The implications of this research ripple far beyond the walls of the SR-Tiget lab. It provides an explanatory framework for some of the disappointing results seen in early clinical trials using HDR-based gene editing in HSPCs. In cases where patients experienced suboptimal engraftment or declining levels of gene-corrected cells over time, it’s possible that underlying senescence was quietly sabotaging the outcome.
Dr. Di Micco reflects on this with urgency: “Our study helps explain why editing sometimes fails, even when the molecular targeting is precise. It’s not enough to look at editing efficiency. We need to understand how the cell is reacting to the editing process at a functional level.”
By incorporating anti-inflammatory strategies like Anakinra into the editing protocol—either pre-treatment or during ex vivo cell manipulation—clinicians may be able to significantly boost the effectiveness of gene therapy for a wide range of inherited diseases. This could be particularly game-changing for conditions that require long-term correction, such as primary immunodeficiencies, beta-thalassemia, or bone marrow failure syndromes, where even a small number of healthy, edited stem cells can mean the difference between health and lifelong illness.
A New Paradigm: Biology-Informed Engineering
The SR-Tiget findings represent a subtle but profound shift in how we think about gene therapy—not just as an engineering challenge, but as a biological one. It’s a reminder that stem cells are not machines, and DNA editing is not a clean cut. There are echoes, ripple effects, and feedback loops. What we do to a cell in a petri dish can echo in a patient’s body for months or years.
By embracing this complexity—and using it as a guide—scientists are building smarter, safer therapies. The goal is not just to fix a gene, but to do so in a way that preserves the cell’s identity, vitality, and future potential.
This is precision medicine in its truest sense: not just precise targeting, but precise care.
Looking Ahead: The Future of Stem Cell Gene Editing
While CRISPR-Cas9 remains a powerful tool, its combination with AAV6 vectors and HDR-based repair templates must now be reevaluated in light of these findings. Future protocols may need to include real-time monitoring of inflammatory markers, short-term use of senescence inhibitors, and more gentle delivery systems to minimize cellular stress.
Moreover, the “memory” of editing—a concept rarely discussed before—raises questions about long-term epigenetic changes and how these might affect the durability of the therapy or the risk of complications years down the line. Understanding and managing this cellular memory may be the next great frontier in regenerative medicine.
As science moves toward base editing, prime editing, and other non-cutting gene editing methods, the lessons from this research remain vital. Any intervention that touches the genome must now be seen not just through the lens of accuracy, but through the lens of biological consequences.
The Takeaway: Engineering with Empathy
The CRISPR revolution taught us that we could rewrite the code of life. This study reminds us that we must also listen to the cell’s response.
Gene editing is not a silent operation—it’s a dialogue, a negotiation between scientific ambition and cellular resilience. And if we want that dialogue to end in healing, we must learn to speak the language of biology, not just the syntax of DNA.
In the end, saving a life may come down not just to what we change in the genome—but how we care for the cell that carries it.
Reference: Senescence and inflammation are unintended adverse consequences of CRISPR-Cas9/AAV6 mediated gene editing in hematopoietic stem cells, Cell Reports Medicine (2025). DOI: 10.1016/j.xcrm.2025.102157. www.cell.com/cell-reports-medi … 2666-3791(25)00230-7