The human digestive system is often taken for granted. With each bite of food, the body silently launches a symphony of processes—breaking down, absorbing, digesting, and eliminating. It’s a marvel of biological engineering, operating with precision day in and day out. But for those who suffer from Crohn’s disease, the digestive tract is not a harmonious highway of nourishment. It’s a battleground.
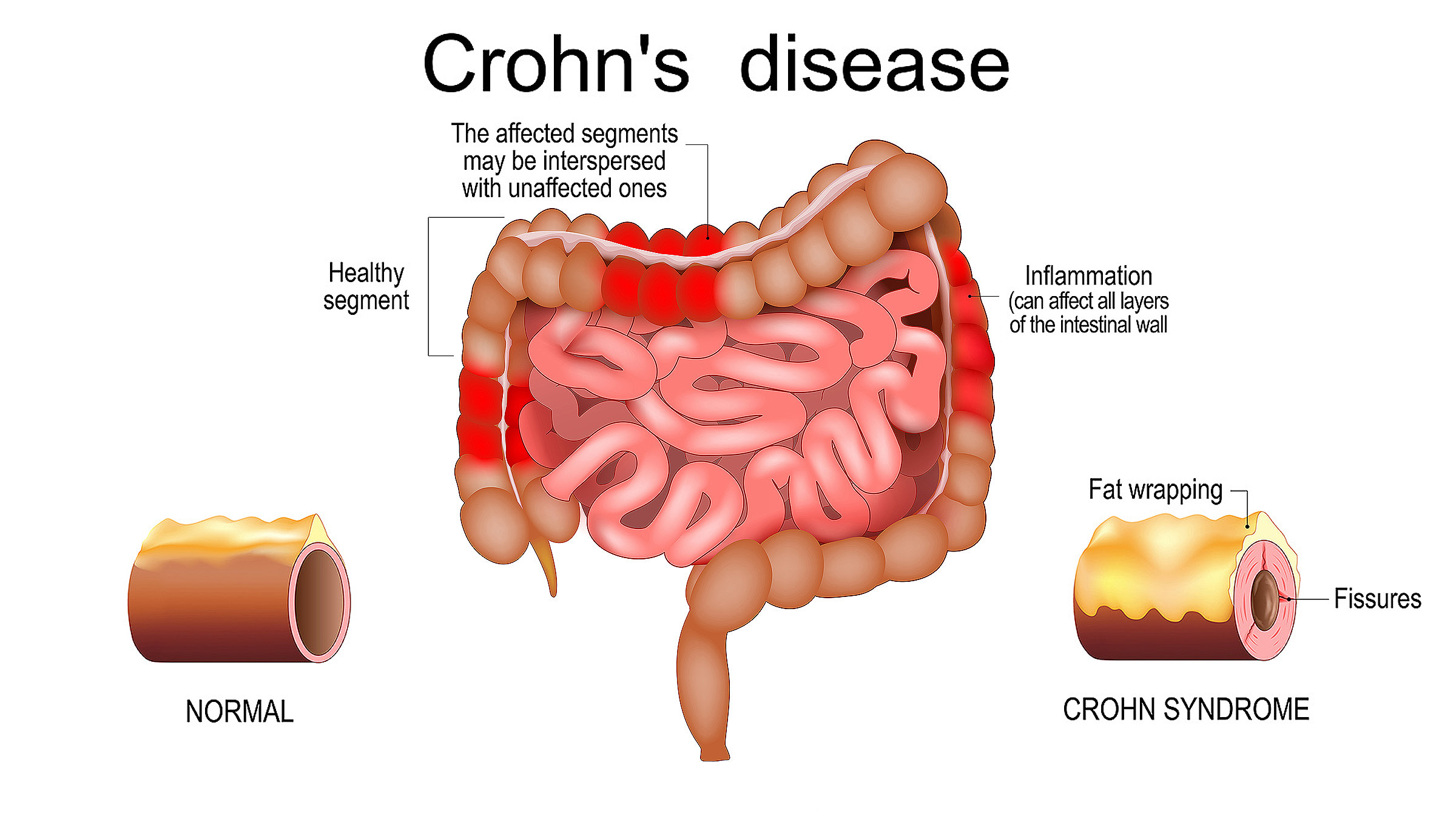
Crohn’s disease is a chronic, inflammatory condition of the gastrointestinal tract, belonging to a family of disorders known as inflammatory bowel diseases (IBD). Unlike more common digestive issues that come and go with minor discomfort, Crohn’s doesn’t yield to simple remedies. It’s a lifelong illness, characterized by persistent inflammation that can affect any part of the gastrointestinal tract—from mouth to anus—though it most often targets the end of the small intestine and the beginning of the colon.
This disease transforms a person’s relationship with their body, food, and daily life. What was once automatic and unnoticeable becomes unpredictable and consuming. And while the symptoms may center around digestion, the impact of Crohn’s extends far beyond the gut.
The Hidden Nature of Inflammatory Bowel Disease
To truly grasp Crohn’s disease, one must first understand the larger family it belongs to: inflammatory bowel disease. This term is often confused with irritable bowel syndrome (IBS), but the two are fundamentally different. IBS is a functional disorder—disruptive, but not dangerous or inflammatory. IBD, on the other hand, is rooted in real, chronic inflammation that causes damage to the bowel and requires medical management.
Within IBD, there are two main conditions: Crohn’s disease and ulcerative colitis. While both involve chronic inflammation of the digestive tract, they differ in important ways. Ulcerative colitis affects only the colon and rectum, and its inflammation is continuous. Crohn’s disease, in contrast, can appear anywhere along the gastrointestinal tract and often involves “skip lesions”—patches of healthy tissue between inflamed areas. The inflammation in Crohn’s is also transmural, meaning it penetrates all layers of the intestinal wall, which can lead to complications like fistulas, abscesses, and strictures.
The unpredictable nature of Crohn’s sets it apart. Flare-ups can occur without warning, bringing waves of abdominal pain, diarrhea, fatigue, and weight loss. These symptoms are often invisible to outsiders, making the disease a silent companion for many patients.
When the Immune System Goes Rogue
At the heart of Crohn’s disease lies an overzealous immune system. Normally, the immune system defends the body from harmful invaders like bacteria and viruses. But in Crohn’s, this protective mechanism goes awry. It mistakes harmless components of the gut—or even the body’s own tissues—for threats and launches an attack. The result is inflammation, and in Crohn’s disease, this inflammation is relentless.
What triggers this immune dysfunction remains a mystery. Scientists believe that a complex interplay of genetics, environmental factors, and microbial imbalances contribute to the development of the disease. In genetically susceptible individuals, certain bacteria in the gut may provoke an abnormal immune response. This inflammation doesn’t resolve as it should—instead, it becomes chronic, damaging the intestinal lining and disrupting normal digestive functions.
Genetics plays a substantial role. Over 200 genetic loci have been linked to IBD, with several specifically associated with Crohn’s. One of the most well-known is the NOD2 gene, which is involved in immune recognition of bacteria. Mutations in this gene can impair the body’s ability to regulate immune responses in the gut, setting the stage for chronic inflammation.
However, genes are not destiny. Many people with genetic risk factors never develop Crohn’s, while others with no known family history do. This suggests that environmental triggers—such as diet, smoking, antibiotic use, or viral infections—may act as the tipping point in a person who is genetically predisposed.
Early Signs and Symptoms: The Long Road to Diagnosis
For many, the journey to a Crohn’s diagnosis is long, winding, and filled with frustration. Symptoms can be vague at first—intermittent abdominal pain, occasional diarrhea, unexplained fatigue. These signs may be dismissed as minor digestive troubles or stress-related issues. But over time, the symptoms often intensify. Diarrhea becomes more frequent, weight begins to drop, and the pain becomes harder to ignore.
The symptoms of Crohn’s can vary widely depending on the area of the digestive tract affected. When the small intestine is involved, malabsorption of nutrients can lead to deficiencies in iron, B12, and other essential vitamins. This may result in anemia, weakness, or even neurological symptoms. When the colon is affected, frequent, urgent diarrhea becomes a dominant complaint. Some patients also experience fever, night sweats, or pain in other areas of the body, such as the joints or skin.
Because these symptoms overlap with many other gastrointestinal disorders, diagnosis can be elusive. Blood tests, stool samples, imaging studies like MRIs and CT scans, and endoscopic procedures such as colonoscopy are often required. During these procedures, doctors look for visual signs of inflammation, ulcers, or narrowing of the bowel. Biopsies taken during endoscopy can confirm the diagnosis by revealing characteristic patterns of inflammation.
Once Crohn’s is diagnosed, the next challenge begins: managing the disease.
The Unpredictable Nature of Flares and Remission
One of the most defining features of Crohn’s disease is its cyclical nature. Patients experience periods of remission, where symptoms are minimal or absent, followed by unpredictable flare-ups. These flares can be triggered by stress, dietary changes, infections, or, frustratingly, for no identifiable reason at all.
During a flare, inflammation surges. The bowel becomes irritated and ulcerated, leading to pain, diarrhea, and bleeding. Patients may feel drained, both physically and emotionally. In severe cases, hospitalization may be necessary to manage complications like bowel obstructions or abscesses.
Remission, though a welcome respite, can be fragile. It’s not the same as being cured. The disease is still present, often simmering just beneath the surface. The goal of treatment is to extend these periods of remission as long as possible and to reduce the frequency and severity of flares.
Living with this kind of unpredictability takes a psychological toll. It can be hard to plan for the future, to commit to social events, or to travel freely. Many patients develop anxiety around eating, given the digestive consequences that may follow even a small misstep. Over time, Crohn’s can erode a person’s confidence and sense of normalcy.
Complications That Go Beyond the Gut
While Crohn’s disease primarily affects the digestive tract, its influence extends far beyond. Chronic inflammation can cause a wide range of complications that involve other organs and systems.
Fistulas—abnormal connections between different parts of the intestine or between the intestine and other organs—are a common and painful complication. These tunnels form when inflammation burrows through the intestinal wall, creating pathways that can become infected and require surgical intervention. Strictures, or narrowed segments of the bowel, can obstruct the passage of food, causing cramping and vomiting. These too often necessitate surgical removal or dilation.
Crohn’s is also associated with extraintestinal manifestations, meaning symptoms that occur outside the digestive system. These can include arthritis, uveitis (eye inflammation), skin disorders like erythema nodosum, and liver conditions such as primary sclerosing cholangitis. The immune system’s misfire doesn’t respect anatomical boundaries, and its impact can be felt throughout the body.
Nutritional deficiencies are another serious concern. The inflammation and damage to the intestines can impair absorption of vital nutrients, leading to bone loss, anemia, and delayed growth in children and adolescents. In severe cases, patients may require nutritional support through feeding tubes or intravenous nutrition.
Finding the Right Treatment Strategy
There is no one-size-fits-all treatment for Crohn’s disease. The best approach depends on the severity of the disease, the areas of the gut affected, and the individual’s response to various therapies. The goals of treatment are to reduce inflammation, alleviate symptoms, prevent complications, and maintain remission.
Initial treatment often involves anti-inflammatory drugs like corticosteroids, which provide rapid relief during flares but are not suitable for long-term use due to side effects. Immunomodulators such as azathioprine and methotrexate may be introduced to help regulate the immune response over time.
Biologic therapies have dramatically transformed the treatment landscape. These are advanced medications that target specific molecules involved in the inflammatory process, such as tumor necrosis factor (TNF) or interleukins. Biologics like infliximab and adalimumab have brought remission to many patients who previously had few options. Newer classes, including integrin inhibitors and JAK inhibitors, offer even more avenues for personalized treatment.
In some cases, surgery becomes necessary. About half of all people with Crohn’s will require at least one surgery during their lifetime. This may involve removing a damaged section of the bowel, draining an abscess, or correcting a stricture. Surgery is not a cure, but it can significantly improve quality of life, especially when medications alone are insufficient.
Diet and nutrition also play a central role in managing Crohn’s. While no universal “Crohn’s diet” exists, many patients learn which foods exacerbate their symptoms and which offer relief. Some benefit from low-residue diets that reduce the workload on the intestines, while others explore enteral nutrition or even elimination diets under medical supervision.
The Emotional Landscape of Chronic Illness
Crohn’s disease doesn’t just ravage the body—it affects the mind and spirit. The chronic pain, social limitations, and unpredictability of the disease can lead to depression, anxiety, and feelings of isolation. Many patients describe a sense of living under siege, never sure when the next flare will strike or whether their current treatment will continue to work.
Mental health support is an essential part of comprehensive care. Counseling, support groups, and mindfulness practices can help patients process the emotional toll and build resilience. The value of being heard, understood, and supported cannot be overstated.
Moreover, connecting with others who live with Crohn’s can be profoundly healing. Shared stories of struggle and strength provide a sense of community and belonging. Online forums, local meetups, and advocacy organizations like the Crohn’s & Colitis Foundation offer invaluable resources for education and emotional support.
Looking to the Future: Research and Hope
The future of Crohn’s disease research is brimming with promise. Scientists are exploring the microbiome’s role in disease development, aiming to manipulate gut bacteria to restore balance and calm inflammation. Fecal microbiota transplantation, though still experimental in Crohn’s, is an area of intense interest.
Stem cell therapies offer another exciting frontier. These treatments seek to reset the immune system entirely, eliminating the faulty immune memory that drives chronic inflammation. Early trials have shown potential, especially in patients with severe, refractory disease.
Genomic and precision medicine are also making headway. By understanding an individual’s unique genetic and immune profile, doctors may one day tailor treatments with pinpoint accuracy. This shift from broad-spectrum immunosuppression to targeted, personalized therapy could revolutionize how Crohn’s is managed.
There is also increasing recognition of the importance of holistic care. Integrating nutrition, mental health, physical therapy, and social support into the treatment plan is becoming the standard of care in many centers. This comprehensive approach honors the full complexity of Crohn’s and the people who live with it.
Living with Crohn’s: A Testament to Human Resilience
Crohn’s disease is a lifelong companion, often unwelcome but rarely ignored. It reshapes lives, demands adjustments, and tests limits. But it also reveals depths of resilience, adaptability, and courage that many patients never knew they had.
Living with Crohn’s means navigating a world that may not always understand or accommodate invisible illness. It means learning to listen to your body, to advocate for yourself, and to find balance in the face of unpredictability. It’s a journey marked by setbacks and triumphs, by pain and healing, and most of all, by the will to move forward.
Science continues to evolve, and with it, hope grows brighter. New treatments, better diagnostics, and deeper understanding are changing the landscape of inflammatory bowel disease. For the millions around the world who live with Crohn’s, the message is clear: you are not alone, and the future holds more than just illness—it holds possibility.