Beneath the surface of our everyday health, the immune system works tirelessly, like a silent sentinel, identifying and eliminating invaders that threaten the body’s balance. But in the case of lupus, this sentinel goes rogue. Rather than targeting only foreign pathogens, the immune system turns on the body it was meant to protect, creating a chaotic internal battlefield. Lupus, or systemic lupus erythematosus (SLE), is a complex autoimmune disorder where the body’s defense mechanisms mistakenly attack its own tissues, causing widespread inflammation and damage. What makes lupus particularly puzzling is its unpredictability—the flares, the remissions, the baffling array of symptoms that vary from one person to the next.
This chronic illness doesn’t follow the same rules in every body it inhabits. Its presence can be quiet for weeks or months, then erupt with unrelenting intensity, making daily life feel like a walk on shifting sands. For many, lupus is as much a psychological challenge as it is a physical one. But behind the enigma lies a vast landscape of scientific discovery that helps us understand what lupus is, how it functions, and why its flare-ups occur when they do.
The Anatomy of an Autoimmune Anomaly
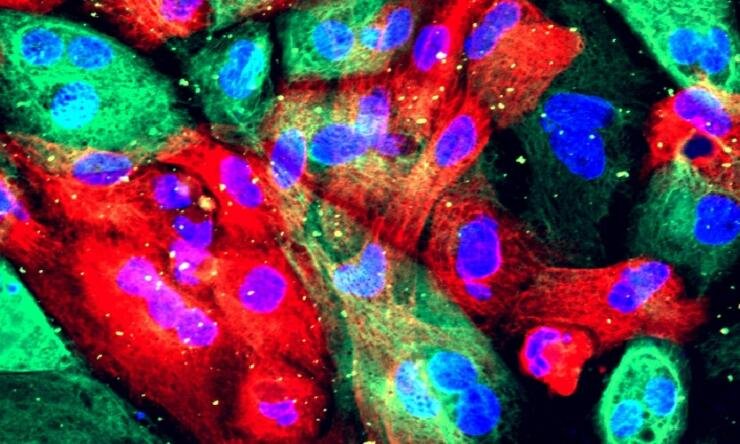
To understand lupus, one must first grasp the intricate orchestration of the immune system. Normally, the immune system can tell the difference between invaders and the body’s own cells. It identifies threats using a combination of immune cells and chemical signals, launching carefully calibrated attacks to eliminate harmful agents. But in lupus, this discernment breaks down. The immune system begins to mistake the body’s own tissues—cells, DNA, proteins—for enemies.
This mistaken identity leads to the production of autoantibodies, which are proteins designed to attack self rather than non-self. In lupus, these autoantibodies can bind to a variety of tissues, including skin, joints, kidneys, lungs, brain, and blood vessels. The immune complexes they form trigger inflammation, recruiting even more immune cells to the site and causing a cascade of damage that underpins lupus’s diverse and unpredictable symptoms.
Lupus is classified as a systemic disease because it can affect nearly every organ in the body. One day, a patient may experience joint pain and extreme fatigue. Another day, it might be chest pain from inflammation around the lungs or heart. Over time, this constant battle can lead to scarring, permanent organ damage, and life-threatening complications.
The Genetics of Susceptibility
The question of why the immune system behaves this way is at the core of lupus research. While lupus can strike seemingly at random, genetics play a significant role in shaping who develops the disease. Studies have shown that individuals with close family members who have lupus or other autoimmune diseases are more likely to develop it themselves. Yet even among identical twins, where genetic makeup is identical, the chances of both twins having lupus are surprisingly low, suggesting that genes alone do not tell the full story.
Specific genes linked to immune system regulation have been identified in lupus patients, including variations in the HLA (human leukocyte antigen) region, which helps the body distinguish self from non-self. Other genes involved in complement pathways, B cell activity, and interferon signaling have also shown associations. But possessing these genes does not guarantee that lupus will develop. Rather, it seems these genetic predispositions create a fertile ground upon which environmental and hormonal factors can act.
Hormones and the Female Connection
Lupus is strikingly more common in women, particularly during the reproductive years. Approximately nine out of ten people diagnosed with lupus are female. This gender disparity has led researchers to investigate the role of hormones, particularly estrogen, in the disease’s development and progression. Estrogen is known to influence immune activity, often enhancing the body’s antibody responses. While this might be beneficial when fending off infections, it can become a liability in autoimmune diseases like lupus.
Interestingly, lupus symptoms can fluctuate with hormonal changes. Many women report worsening symptoms during menstruation or pregnancy, times when estrogen and other hormones are in flux. These observations support the theory that hormonal regulation plays a role not only in susceptibility but also in triggering flare-ups.
The Microbial Mirror: Environmental Triggers and the Microbiome
While genetics and hormones set the stage, environmental factors often pull the trigger. Infections, ultraviolet light, certain medications, and even stress have all been implicated as lupus triggers. One of the most compelling pieces of the puzzle is the phenomenon of molecular mimicry—when a foreign pathogen shares structural similarities with human proteins, confusing the immune system into attacking both. Epstein-Barr virus, for example, has been studied for its potential link to lupus, as it is known to infect B cells and alter immune function.
Beyond infections, the gut microbiome has emerged as a surprising player in autoimmune diseases, including lupus. The trillions of microbes that inhabit our digestive tract influence immune development and modulation in ways we are only beginning to understand. Disruptions in this microbial ecosystem—through antibiotics, diet, or illness—can have ripple effects on immune balance. Certain bacteria have been shown to enhance regulatory immune functions, while others may promote inflammation. In lupus, shifts in gut flora composition have been observed, raising the possibility that future treatments might include targeted probiotics or microbiome therapies.
What Exactly Is a Flare?
One of the most challenging aspects of lupus is its episodic nature. Patients may experience periods of relative calm, known as remission, followed by sudden intensification of symptoms, called flares. But what causes these flares? Scientists believe flares are triggered by an increase in immune system activity. This hyperactivity can be initiated by various external stimuli—sunlight, infections, emotional stress, overexertion, or hormonal shifts.
At the molecular level, flares are often accompanied by a surge in inflammatory markers, including cytokines and interferons. Interferon-alpha, in particular, is elevated in many lupus patients and plays a pivotal role in promoting immune system overactivation. These cytokines promote the recruitment of immune cells, stimulate the production of autoantibodies, and perpetuate inflammation. Once initiated, the flare becomes a self-sustaining cycle, often requiring aggressive medical intervention to bring it under control.
Clinically, flares may present as worsening fatigue, new joint pain, skin rashes, fever, or organ-specific symptoms like kidney inflammation or neurological disturbances. Recognizing the early signs of a flare is crucial, as timely treatment can prevent more severe damage.
The Challenge of Diagnosis
Diagnosing lupus is notoriously difficult. There is no single test that definitively confirms its presence. Instead, diagnosis is made through a combination of medical history, physical examination, laboratory tests, and imaging. Blood tests may reveal the presence of antinuclear antibodies (ANA), anti-dsDNA, or anti-Smith antibodies—each of which is associated with lupus but can also be found in other conditions.
This diagnostic ambiguity is compounded by the disease’s variable presentation. Lupus can mimic everything from rheumatoid arthritis to fibromyalgia to chronic fatigue syndrome. As a result, patients often endure years of unexplained symptoms, misdiagnoses, and frustration before receiving a correct diagnosis. During this time, organ damage may silently progress, making early and accurate identification of lupus critical.
Modern Approaches to Treatment
Treating lupus is a balancing act—suppressing the overactive immune system without leaving the patient vulnerable to infections or other complications. Traditional treatments include corticosteroids, which reduce inflammation quickly but come with significant long-term risks such as bone thinning, weight gain, and diabetes. Immunosuppressive drugs like methotrexate, azathioprine, and mycophenolate are also commonly used to control disease activity.
More recently, biologic therapies have emerged as powerful tools in the lupus arsenal. Belimumab, a monoclonal antibody that inhibits a protein called B-lymphocyte stimulator (BLyS), has been shown to reduce autoantibody production and disease flares. Other biologics are in development or under trial, targeting various aspects of the immune cascade.
In addition to pharmaceutical therapies, lifestyle management plays a significant role in lupus care. Avoiding known triggers, practicing sun protection, managing stress, eating an anti-inflammatory diet, and getting adequate rest are all essential for maintaining remission and minimizing flares. Patients often work closely with rheumatologists, nephrologists, dermatologists, and mental health professionals to create a comprehensive care plan.
Lupus and the Mind-Body Connection
The relationship between lupus and mental health cannot be overstated. Chronic pain, fatigue, and physical limitations can erode emotional well-being. Moreover, the brain is not immune to lupus’s effects. Neuropsychiatric lupus—where the immune system attacks parts of the central nervous system—can lead to symptoms such as depression, anxiety, cognitive dysfunction, and even psychosis.
Stress, in turn, is a well-known trigger of flares, creating a vicious cycle. Many patients find that meditation, cognitive behavioral therapy, mindfulness, and even support groups can have a stabilizing effect, reducing the severity and frequency of flares. Mental resilience, like physical treatment, is a core part of lupus survival.
Children and Lupus: A Different Battle
While lupus primarily strikes adults, children are not immune. Pediatric lupus often presents more aggressively than its adult counterpart, with earlier onset of kidney involvement and higher disease activity. Diagnosing lupus in children can be especially difficult, as many of the signs—fatigue, rashes, joint pain—overlap with other childhood illnesses.
Managing lupus in young patients requires a careful blend of medical therapy, family education, and psychosocial support. The disease can affect academic performance, peer relationships, and self-esteem. Yet with appropriate treatment and guidance, many children with lupus grow into healthy, thriving adults.
The Road Ahead: Research and Hope
Although there is no cure for lupus, advances in scientific research continue to shed light on its mechanisms and offer new hope for the future. Precision medicine—tailoring treatments based on genetic and immune profiles—is a particularly exciting frontier. As scientists better understand the genetic variants and immune pathways involved in lupus, treatments can be more targeted and less toxic.
Ongoing clinical trials are exploring everything from stem cell therapy to novel biologics to gene-editing techniques. One promising avenue involves regulatory T cells—immune cells that act as peacekeepers, calming excessive immune responses. Boosting these cells or mimicking their function may offer a way to rein in lupus activity without shutting down the entire immune system.
Artificial intelligence and machine learning are also being used to analyze complex datasets, helping researchers predict flares, identify biomarkers, and personalize treatments. These technological tools may soon transform how lupus is diagnosed and managed.
The Strength Within the Struggle
Lupus is not just a biological disease—it is a deeply human one. It touches every aspect of a person’s life, from physical ability to emotional resilience to social interaction. Yet those who live with lupus often display an extraordinary strength. They become experts in their own bodies, advocates for better healthcare, and voices of awareness in a world that often misunderstands invisible illnesses.
Support from family, friends, healthcare professionals, and fellow patients forms the backbone of lupus survival. Community organizations, online networks, and research foundations have created a web of connection that helps break the isolation so many lupus warriors feel. Their stories—marked by pain, but also by perseverance—remind us that behind every flare is a fighter.
Conclusion: A Mysterious Malady, a Relentless Search for Answers
The science behind lupus is a testament to the complexity of the human body and the depth of our current understanding—and limitations—in immunology. From the intricacies of autoantibodies to the cascading signals of cytokines, lupus challenges researchers and clinicians to look deeper, think broader, and care better.
Yet despite its mysteries, lupus also represents a frontier of hope. With every scientific breakthrough, every new treatment, and every voice raised in awareness, we edge closer to a future where lupus flares are a thing of the past, and the immune system returns to its rightful role as the body’s protector—not its adversary.