For millions around the world, the simple acts of walking, opening a jar, or gripping a pen can feel like daunting tasks due to joint pain. When stiffness in the knees becomes a morning ritual or swelling in the hands turns routine chores into challenges, the culprit is often arthritis. But while arthritis is commonly referred to as a single condition, it is actually an umbrella term that encompasses over a hundred different diseases. Among them, two of the most prevalent—and most frequently confused—are rheumatoid arthritis and osteoarthritis.
To the untrained eye, they may seem like twins, dressed in similar symptoms of joint pain, stiffness, and swelling. But beneath the surface, these two conditions tell very different stories. One is a tale of mechanical wear and tear, the other of immune system betrayal. Knowing which type of arthritis you’re dealing with is not merely a matter of terminology—it affects treatment decisions, prognosis, and how life must be adapted around it. To understand these diseases fully, one must dive deep into the inner workings of the body, where cartilage meets bone, and where immune cells can become misguided warriors.
The Body’s Architectural Framework
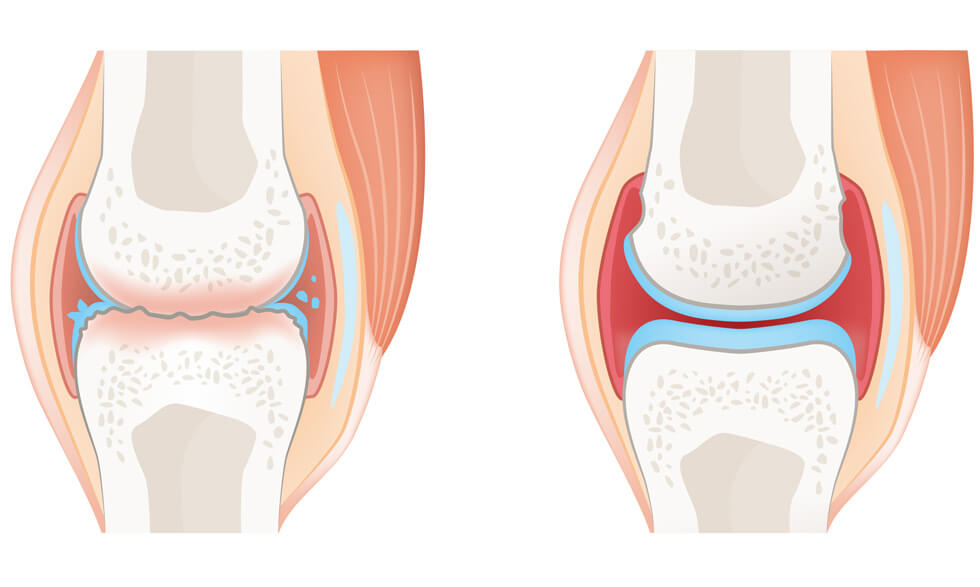
Joints are engineering marvels—fluid, mobile connections that allow bones to move with ease and precision. Each joint is cushioned by cartilage, a slick tissue that minimizes friction and acts as a shock absorber. Around the joint lies the synovium, a soft lining that produces synovial fluid to lubricate movement. Ligaments hold the bones together, while muscles contract and stretch to enable motion.
When everything works in harmony, joints operate with an effortless grace. But when arthritis enters the scene, this harmony begins to unravel. In osteoarthritis, the deterioration of cartilage leads to bone grinding on bone. In rheumatoid arthritis, the very synovium that keeps joints fluid becomes inflamed, thickened, and destructive. Though the pain may feel similar, the damage comes from radically different places.
Rheumatoid Arthritis: The Body’s Civil War
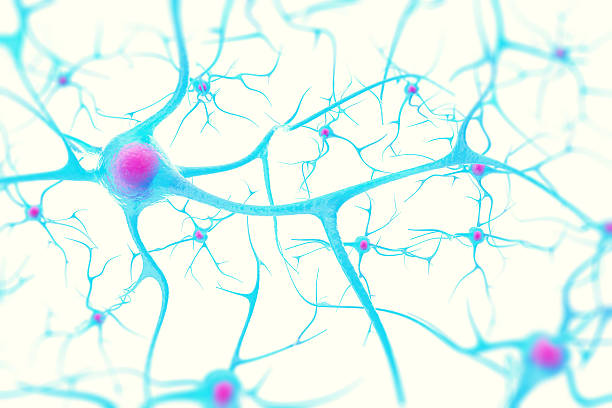
Rheumatoid arthritis is not just a joint disease—it is an autoimmune condition. In RA, the body’s immune system, which is supposed to protect against infections and invaders, turns against its own tissues. Specifically, it targets the synovium, the lining of the joints. This misguided attack leads to chronic inflammation, which thickens the synovium and damages cartilage and bone.
What makes RA particularly insidious is that it often affects joints symmetrically. If one hand is swollen and painful, the other likely is too. This symmetry is a telltale sign of autoimmune involvement. Over time, if left unchecked, RA can lead to joint deformities, bone erosion, and severe disability.
But RA doesn’t stop at the joints. It is a systemic disease, meaning it can affect other organs, including the eyes, lungs, heart, and even blood vessels. Fatigue, low-grade fever, and malaise often accompany joint symptoms. It’s as if the immune system has declared war on the entire body, not just the knees or hands.
Osteoarthritis: The Toll of Time and Use
Unlike RA, osteoarthritis is a mechanical issue. Often described as “wear and tear” arthritis, OA develops when the cartilage that cushions joints gradually breaks down. Without this protective layer, bones begin to rub against each other, leading to pain, swelling, and loss of movement. The process is usually slow and progressive, and the damage is irreversible.
OA typically starts in one joint and may remain localized. It is more likely to affect weight-bearing joints like the hips, knees, and spine, though fingers and thumbs are also common targets. Unlike the symmetrical pattern of RA, OA tends to be unilateral or confined to specific areas of stress and strain.
Age is the most significant risk factor for OA, but it’s not the only one. Repetitive motion, previous joint injuries, obesity, and genetics all play a role in who develops this form of arthritis. While RA can strike at any age, OA tends to creep in later in life, often as a companion to aging.
When Mornings Speak Loudest
One of the first signs that something is amiss in the joints is morning stiffness. But even this seemingly simple symptom reveals the contrasting nature of RA and OA. In rheumatoid arthritis, morning stiffness is prolonged—lasting an hour or more—and can be so intense that patients find themselves immobilized. It often eases with activity as the joints “warm up,” but the lingering fatigue remains.
In osteoarthritis, stiffness is typically shorter-lived, usually less than thirty minutes, and often returns at the end of the day after periods of use. The pain in OA is more mechanical; it worsens with activity and improves with rest. In RA, the opposite is often true—activity can help relieve stiffness and pain, at least temporarily.
Understanding the quality and timing of symptoms can provide valuable clues. In a clinical setting, doctors listen carefully to these descriptions, using them alongside physical exams and diagnostic tests to distinguish between the two diseases.
Markers in the Blood and Shadows on the X-Ray
The laboratory and imaging tests used to diagnose arthritis are like fingerprints—they don’t always tell the whole story, but they can confirm suspicions. In rheumatoid arthritis, blood tests often reveal the presence of specific antibodies, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP). Elevated inflammatory markers like ESR and CRP suggest systemic inflammation.
Imaging in RA might show joint erosion and narrowing, especially in smaller joints of the hands and feet. In early RA, soft tissue swelling may be the only visible change. In osteoarthritis, X-rays typically reveal joint space narrowing due to cartilage loss, the presence of bone spurs (osteophytes), and sclerosis of bone underneath the cartilage.
MRI and ultrasound offer even more sensitive ways to detect inflammation and joint damage, especially in the early stages of disease. Yet, diagnosis remains a puzzle, requiring pieces from symptoms, history, blood, and images to fit together into a coherent picture.
The Tale of Two Treatments
Once a diagnosis is made, the paths of treatment diverge sharply. For rheumatoid arthritis, the goal is to tame the immune system and reduce inflammation before permanent damage is done. This often involves disease-modifying antirheumatic drugs (DMARDs) like methotrexate, as well as biologics that target specific immune pathways.
Biologics have revolutionized RA treatment, offering hope where little existed before. Medications like adalimumab, etanercept, and tocilizumab block key players in the inflammatory cascade. These drugs can slow or even halt joint damage if started early. But they also come with risks, particularly increased susceptibility to infections, and require careful monitoring.
In contrast, osteoarthritis treatment focuses more on managing symptoms and preserving joint function. There are no medications that can stop the progression of OA, so the strategy leans heavily on pain relief, lifestyle changes, and physical therapy. Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, topical treatments, and corticosteroid injections are frequently used.
In advanced cases, when joint destruction becomes severe, surgery may be necessary. Joint replacement, especially in the hips and knees, has become a common and highly successful intervention in OA. While surgery can also be a last resort in RA, the emphasis is more often on early medical management to prevent reaching that point.
The Emotional Landscape
Both RA and OA exact a toll that extends far beyond the physical. Chronic pain, fatigue, and limited mobility can lead to frustration, anxiety, and depression. For people with RA, the unpredictability of flares and the knowledge that their immune system is attacking them can foster a sense of betrayal by their own bodies.
Osteoarthritis, though slower to progress, brings its own emotional burden. The gradual loss of independence, the inability to perform once-simple tasks, and the fear of a future defined by pain can weigh heavily on patients. Relationships can be strained, employment may be affected, and quality of life often diminishes.
Support systems are crucial. Whether through family, friends, or arthritis support groups, emotional resilience is often built through connection and shared experience. Education is empowering, allowing patients to better advocate for themselves and make informed decisions about their care.
The Research Frontier
While both diseases remain incurable, research is advancing rapidly. In rheumatoid arthritis, the focus is on identifying biomarkers that can predict disease course and response to treatment. The hope is to tailor therapies to the individual, minimizing trial and error.
Scientists are also investigating the genetic and environmental triggers of RA, hoping to unlock what sets the immune system on its destructive path. The microbiome has emerged as a promising area of interest, with studies suggesting that gut bacteria may influence immune function in surprising ways.
In osteoarthritis, researchers are exploring regenerative medicine, including stem cell therapy and tissue engineering, to repair damaged cartilage. Advances in imaging and biomechanics are also providing new insights into how joints degrade and how interventions can be more precisely targeted.
Lifestyle medicine is gaining ground in both conditions, with growing recognition that diet, exercise, sleep, and stress management are not just supportive measures, but central to long-term outcomes.
Looking Ahead: Life After Diagnosis
Being diagnosed with arthritis—whether rheumatoid or osteoarthritis—marks the beginning of a journey, not the end. It is a journey that will involve adaptation, perseverance, and moments of both triumph and frustration. But it is not one that must be walked alone.
In recent years, the arthritis community has grown stronger and more connected. Online forums, advocacy organizations, and medical advances have transformed what was once an isolating experience into a more navigable path. Patients today have more options, more information, and more hope than ever before.
Understanding the difference between rheumatoid arthritis and osteoarthritis is about more than labels. It’s about recognizing the unique challenges each presents, the different ways they impact lives, and the specific strategies needed to live well with them. By illuminating those differences, we open the door to better care, greater empathy, and ultimately, better lives for those who live with these chronic conditions.