Imagine waking up every day knowing that the muscles in your body are slowly, inexorably weakening. Your legs might not support you as they once did. Climbing stairs becomes an ordeal, lifting even a cup of water can become a challenge. Muscular dystrophy is not a single disease but a group of genetic disorders united by a devastating characteristic: progressive muscle wasting. For those who suffer from it, the very tissue that powers their movements, their posture, their breath, and sometimes even their heartbeat, is being quietly and relentlessly torn down by a genetic betrayal.
At the heart of this biological tragedy lies the mystery of causation. What exactly triggers this merciless decline? Why does the body’s most powerful tissue crumble instead of grow stronger? To answer these questions, we must dive deep into the molecular mechanisms of life itself, navigate the corridors of human inheritance, and explore the fragile blueprint written into every cell.
Understanding the Muscle’s Machinery
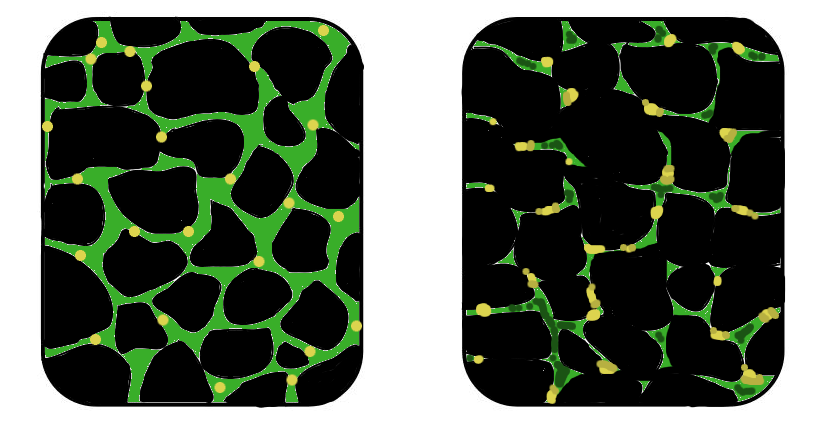
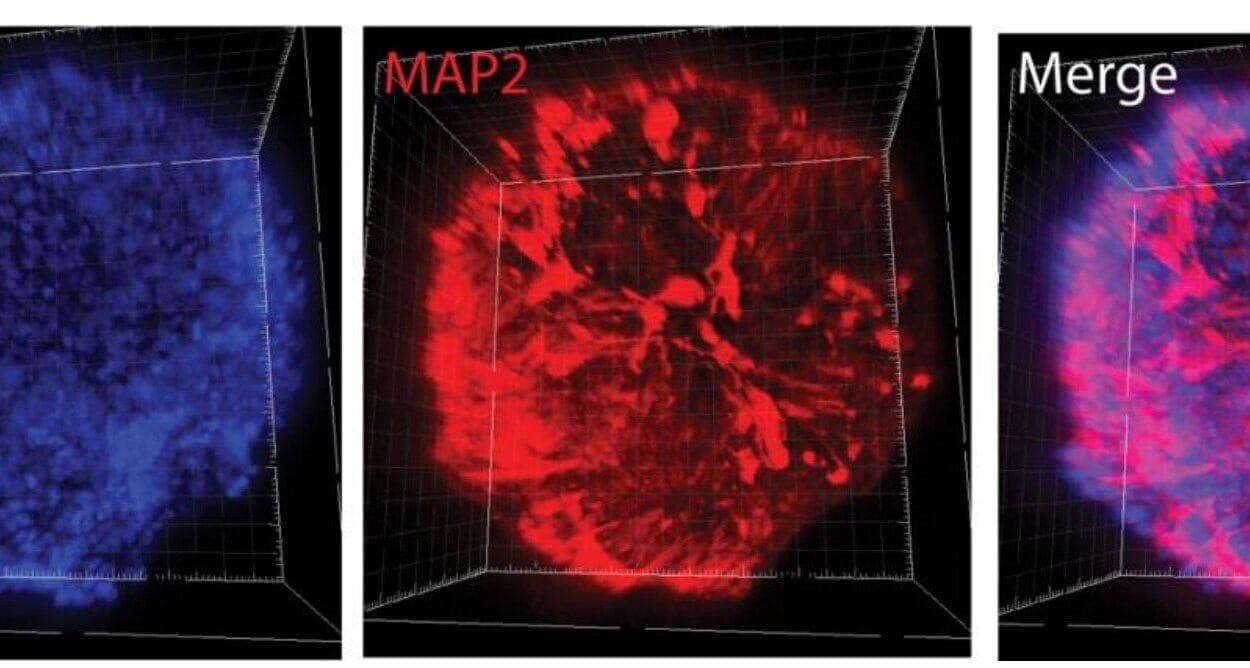
To truly grasp what causes muscular dystrophy, we must first understand what muscles are and how they function. Human muscles are marvels of biological engineering. Composed primarily of fibers made from muscle cells called myocytes, these tissues contract and relax in coordinated patterns to move the body. Embedded within these cells is a complex latticework of proteins that connect the internal scaffolding of the cell to its external environment, creating a mechanical bridge that translates neural signals into movement.
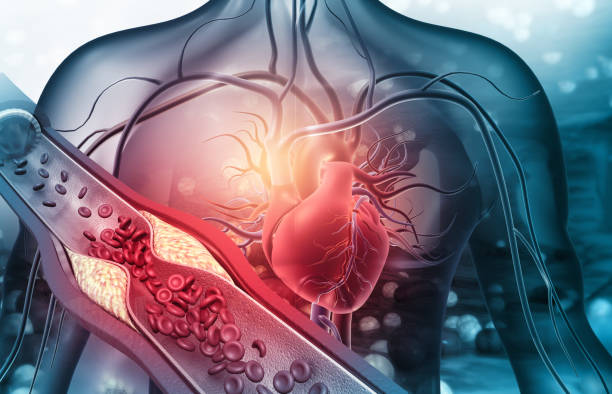
One of the most critical of these proteins is dystrophin, a kind of molecular shock absorber that protects muscle fibers from the damage of repeated contractions. Think of dystrophin as the rubber padding between your body and the concrete of physical stress. Without it, every step, every lift, every beat of the heart becomes a strain the muscles can’t withstand. And this is precisely where muscular dystrophy begins—in the genetic codes that produce or fail to produce this vital protein.
Genes as Architects: The Role of DNA in Muscular Health
Muscular dystrophy is, at its core, a genetic disease. Our DNA carries the instructions to build proteins, the building blocks of every cell. These instructions are organized into genes. When a gene responsible for producing a key muscle protein is faulty—through mutation or deletion—the body either produces a malformed protein or none at all. Over time, without that protein to support and stabilize muscle fibers, the muscles weaken, break down, and are replaced by fat and fibrous tissue.
In many types of muscular dystrophy, such as Duchenne and Becker, the genetic defect lies in the DMD gene, which provides instructions for making dystrophin. Duchenne muscular dystrophy, the most severe and common form in children, is caused by mutations that entirely prevent the production of functional dystrophin. Without this protein, muscles degenerate rapidly, often leading to loss of ambulation in early adolescence and life-threatening complications by adulthood.
Becker muscular dystrophy, though also caused by DMD gene mutations, tends to be milder. That’s because the mutations allow for the production of a shorter but still partially functional form of dystrophin. The difference between Duchenne and Becker isn’t a matter of different genes—it’s a matter of how severely the gene has been damaged. These variations, large and small, across the genome lead to the many forms of muscular dystrophy, each with its own timeline, severity, and symptoms.
Inherited or Spontaneous: The Genetic Lottery
The tragedy of muscular dystrophy often begins before a child is even born. It is a disease inherited through the generations, passed from parent to child via defective genes. Some forms are X-linked, meaning the defective gene is found on the X chromosome. Since males have only one X chromosome, they are far more likely to develop these forms when they inherit a single defective gene from their mother. Females, having two X chromosomes, are usually carriers—protected by the presence of one normal gene.
In Duchenne and Becker muscular dystrophy, this X-linked pattern dominates. Carrier mothers often show no symptoms, but they can pass the defective gene to their children. Sons who inherit it will likely suffer the disease. Daughters who inherit it become carriers themselves.
However, not all cases are inherited. Sometimes, mutations occur spontaneously during the formation of reproductive cells or early embryonic development. These are called de novo mutations. When this happens, a child can develop muscular dystrophy even if there’s no known family history. This genetic unpredictability can shock families and confound diagnosis, underscoring how fragile our genetic code can be.
Different Genes, Different Dystrophies
While Duchenne and Becker dystrophies are the most well-known, they are just two members of a larger family. Each form of muscular dystrophy is caused by mutations in different genes, each responsible for different structural proteins in muscle cells.
In limb-girdle muscular dystrophy, a diverse group of disorders affecting the hip and shoulder muscles, mutations can occur in any one of several genes. Some of these genes code for proteins that help anchor muscle cells to the extracellular matrix—a network that stabilizes tissue. When these proteins are missing or defective, the result is muscle wasting centered in the limbs.
Facioscapulohumeral muscular dystrophy, a condition that begins with weakness in the facial and shoulder muscles, has a more complex cause. Instead of a single gene mutation, it involves an unusual contraction in a stretch of DNA called D4Z4 on chromosome 4. This leads to the inappropriate activation of a gene that is normally silent in muscle tissue. The result is a toxic gain-of-function where the gene produces a protein that actively damages the muscle.
Myotonic dystrophy, another distinct form, is caused by the expansion of repeated sequences of DNA in specific genes. These expansions interfere with the processing of RNA and disrupt many cellular processes, leading to muscle weakness, stiffness, and multisystem complications. Unlike many other forms, it is inherited in an autosomal dominant fashion, meaning a single copy of the defective gene from either parent is enough to cause the disease.
The Domino Effect: How a Single Mutation Wreaks Havoc
What makes muscular dystrophy especially cruel is how a single point of failure in the genetic code can unleash a chain reaction of destruction. The absence of one protein doesn’t just weaken a cell—it makes it vulnerable. Every time the muscle contracts, microscopic tears form in the cell membrane. Without proteins like dystrophin to patch these tears or stabilize the structure, the cell leaks essential materials and takes in damaging molecules like calcium ions.
The result is cellular chaos. Calcium overload activates enzymes that degrade proteins. The cell’s energy factories—mitochondria—become dysfunctional. The immune system is summoned, interpreting the damage as injury. But this response, meant to heal, becomes destructive. Inflammation floods the tissue, causing further damage. The body tries to repair the damage by forming scar tissue, but in doing so, it replaces healthy muscle with stiff, fibrous matter.
This process repeats itself endlessly. The stronger a muscle contracts, the more it injures itself. The very effort to live—moving, walking, breathing—accelerates the disease.
Genetic Testing: Reading the Fault Lines in DNA
Because the causes of muscular dystrophy are rooted in the genes, diagnosis increasingly depends on genetic testing. Decades ago, doctors had to rely on symptoms, family history, and muscle biopsies to make a diagnosis. Today, a simple blood test can scan for known mutations across many genes, identifying the specific type of muscular dystrophy with remarkable accuracy.
Genetic testing also offers something even more powerful: the ability to identify carriers. Mothers who carry the defective gene can be identified before they ever conceive. In some cases, prenatal testing can determine whether a fetus has inherited the mutation, offering families the ability to plan and prepare.
Still, the complexity of our genome means that not all mutations are easily found. Some are novel, never seen before in science. Others may lie in non-coding regions of DNA, affecting gene expression in subtle ways. This is why muscular dystrophy research continues to evolve, as scientists develop more advanced tools to read and interpret the genetic code.
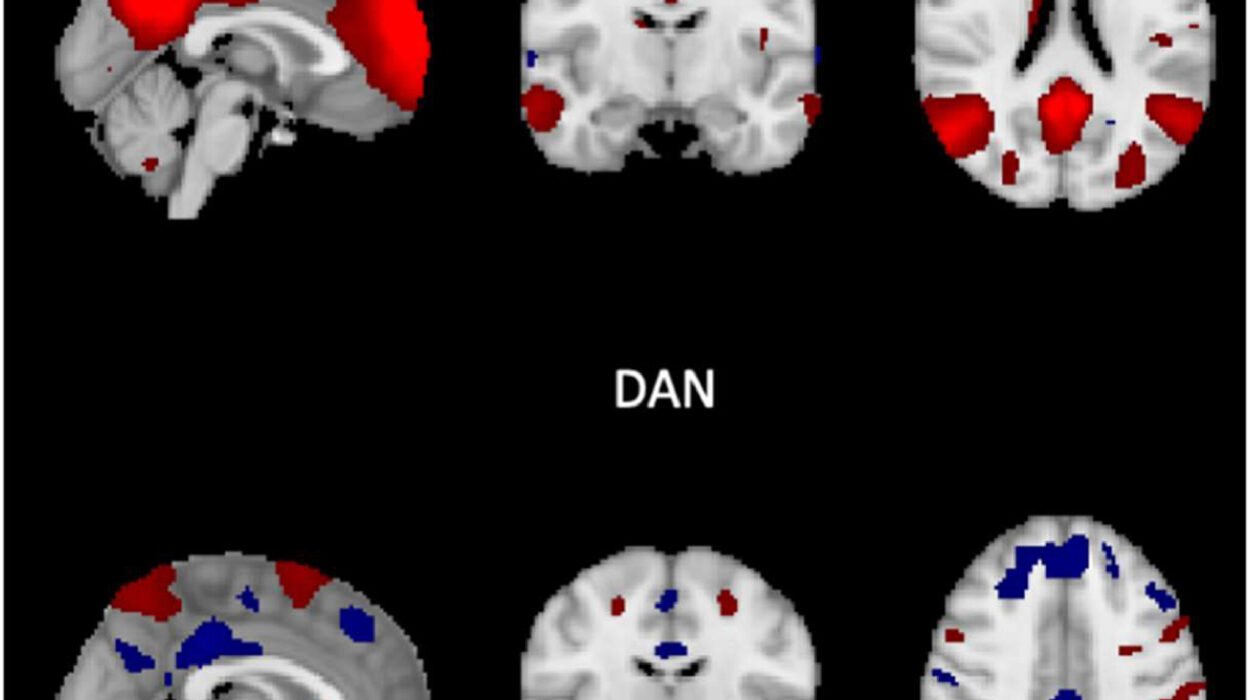
The Emerging Role of Epigenetics
In recent years, attention has turned to epigenetics—the chemical modifications that regulate gene activity without changing the underlying DNA sequence. Epigenetic markers act like switches and dimmers, turning genes on or off, or modulating their intensity. In some forms of muscular dystrophy, such as facioscapulohumeral dystrophy, it’s not the gene itself that’s mutated, but the way it’s epigenetically regulated.
Environmental factors, aging, and even stress can influence these epigenetic signals, meaning that even identical genetic mutations might lead to different disease outcomes in different people. Understanding epigenetics opens the door to new treatment strategies that don’t just replace defective genes but aim to correct their regulation.
Gene Therapy and the Future of Muscle Medicine
Knowing what causes muscular dystrophy has inspired a global scientific quest to fix it at the root. Gene therapy, once a science-fiction dream, is now a reality. In 2023, the U.S. Food and Drug Administration approved the first gene therapy for Duchenne muscular dystrophy. This treatment delivers a shortened version of the dystrophin gene to muscle cells using a virus engineered to be harmless.
This isn’t a cure—yet. But it’s a monumental step. Gene therapy aims to restore production of dystrophin where there was none. Other techniques, like CRISPR gene editing, promise the ability to correct mutations directly within the DNA. Though still experimental, these approaches offer a glimpse into a future where the genetic errors that cause muscular dystrophy could be permanently erased.
Stem cell therapies, exon skipping drugs, and molecular treatments are also in development. Each targets a different part of the disease process, from stabilizing muscle fibers to reducing inflammation to compensating for missing proteins. What they all have in common is their foundation in the science of causation. You can’t fix what you don’t understand.
Conclusion: Beyond the Code
Muscular dystrophy is caused by mutations in the genes that build and sustain our muscles, but its story is far more than a tale of DNA. It is a story of biology’s fragility, of how the body’s most basic structures can betray us, and of how scientific understanding can offer hope even in the face of devastation.
We now know that muscular dystrophy begins with a mistake in the genetic blueprint, a single letter out of place, a page torn from the manual of life. But we also know that with knowledge comes power—the power to diagnose earlier, to treat more effectively, and, perhaps one day, to cure.
As we continue to explore the causes of muscular dystrophy, we are not just unlocking the secrets of muscle. We are also confronting the limits of human biology and the promise of human ingenuity. Because within every cell that falters lies the potential for healing. And within every patient’s story lies a challenge to science: to rewrite the code, to restore the strength, and to return to the body what it was once denied.