Depression is not just sadness—it is a smothering fog that dims the senses, drains vitality, and hollows out the mind. It steals away joy, purpose, and connection. Despite growing awareness and expanding treatment options, the condition continues to haunt hundreds of millions across the globe. According to the World Health Organization, approximately 5% of the global population is currently battling depression. But behind this average lies an often-overlooked and heartbreaking reality: for many individuals, depression becomes a stubborn, unrelenting monster—resistant to even the most advanced treatments.
Treatment-resistant depression (TRD), as the name implies, occurs when a person does not respond to at least two different classes of antidepressants. This condition can persist for years, leaving patients in limbo, cycling through medications, therapies, and lifestyle changes without lasting relief. For these individuals, conventional psychiatry begins to look like a broken promise. But in recent years, a surprising new class of compounds has emerged from the shadows of neuroscience: neurosteroids—natural molecules produced by the brain itself—offering new hope where everything else has failed.
Beyond the Serotonin Era: A Shift in the Scientific Paradigm
For decades, the primary biological theory behind depression focused on a deficiency in neurotransmitters like serotonin, norepinephrine, and dopamine. The logic was simple: if these chemicals regulate mood, then boosting their levels should relieve depression. This led to the rise of medications such as SSRIs and SNRIs, which act by increasing the availability of these neurotransmitters in the brain.
Yet despite their widespread use, these drugs have limitations. For many patients, they take weeks to begin working—if they work at all. Side effects like weight gain, emotional numbness, sexual dysfunction, and insomnia are common. Even worse, up to one-third of individuals with depression never achieve full remission. For this group, the monoamine hypothesis—the foundation of modern antidepressant therapy—seems inadequate.
That’s where neurosteroids enter the picture, not just as new treatments, but as evidence of a broader, more intricate understanding of the brain. They challenge the prevailing theories and open doors to fundamentally different therapeutic strategies.
Neurosteroids: The Brain’s Ancient Alchemy
Neurosteroids are a class of steroid molecules that are synthesized in the brain from cholesterol or steroidal precursors. Unlike hormones like cortisol or testosterone, which are produced primarily by peripheral glands and act systemically, neurosteroids act locally within the brain. Their roles are subtle, powerful, and underappreciated—until now.
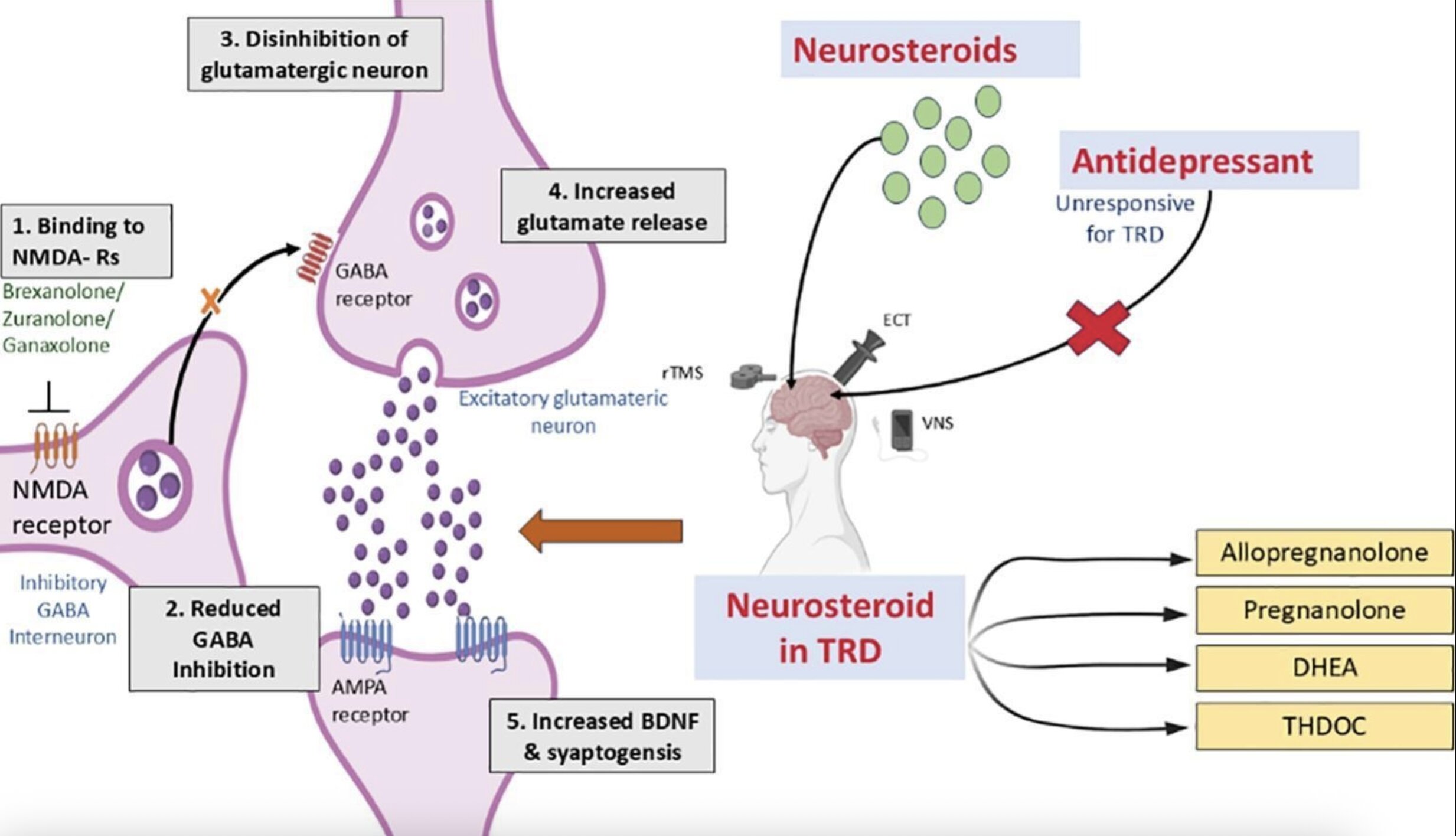
These molecules affect the function of neurotransmitter systems, including gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) receptors. These are not minor players: GABA is the brain’s primary inhibitory neurotransmitter, helping to calm neural activity and promote emotional stability, while NMDA receptors play a central role in learning, memory, and synaptic plasticity—the ability of neurons to form and reshape connections.
One particularly compelling neurosteroid is allopregnanolone, a potent GABA_A receptor modulator. It’s synthesized in response to stress and fluctuates with hormonal changes, particularly in women. The clinical implications are striking: fluctuations in allopregnanolone have been linked to postpartum depression, premenstrual dysphoric disorder, and severe mood swings during menopause.
Unlike traditional antidepressants, which attempt to tweak brain chemistry indirectly over time, neurosteroids act quickly and at multiple levels. They modulate the brain’s stress-response systems, reduce neuroinflammation, and promote neurogenesis and synaptic repair. This makes them uniquely suited to treat depression that has resisted other interventions.
The Breakthrough: Brexanolone and Beyond
In 2019, the U.S. Food and Drug Administration approved brexanolone, an intravenous formulation of allopregnanolone, for the treatment of postpartum depression (PPD)—a severe form of depression that affects women after childbirth. This marked a watershed moment in psychiatry: the first approval of a neurosteroid-based treatment for depression, and the first targeted treatment specifically for PPD.
Brexanolone works fast—within 60 hours in some cases—and provides lasting relief after just one administration. Its mechanism of action differs completely from standard antidepressants. Rather than altering serotonin or norepinephrine levels, it enhances GABAergic inhibition and restores disrupted neurochemical networks in the brain.
But brexanolone is not without drawbacks. It requires a 60-hour infusion under strict medical supervision, making it expensive and logistically challenging. Its approval, however, has galvanized research into more practical alternatives, including oral neurosteroid analogs like zuranolone, currently undergoing clinical trials with promising results.
The New Frontier: Neuroplasticity and the HPA Axis
Beyond symptom relief, neurosteroids seem to restore core biological functions that are impaired in chronic depression. Two of the most exciting effects involve neuroplasticity and the hypothalamic-pituitary-adrenal (HPA) axis.
Depression is often associated with decreased neuroplasticity—the brain’s ability to adapt, rewire, and heal itself. Chronic stress, a key factor in many depressive episodes, floods the brain with cortisol, shrinking the hippocampus (a center for memory and emotion) and weakening synaptic connections. Neurosteroids, especially allopregnanolone and pregnenolone, counteract these effects. They stimulate the formation of new neurons, repair damaged circuits, and strengthen the very architecture of thought and emotion.
At the same time, neurosteroids regulate the HPA axis, the command center of the brain’s stress response. In people with depression, this system often becomes dysregulated, leading to persistent anxiety, sleep disturbances, and feelings of despair. By recalibrating the HPA axis and reducing its overactivation, neurosteroids help restore the body’s natural stress-coping mechanisms.
A Review from India: Synthesizing the Evidence
In a recent publication in Neuroscience, researchers from Smt. Kishoritai Bhoyar College of Pharmacy in India—Krutika Nagpurkar, Pratik Ghive, and colleagues—delved deep into the science and promise of neurosteroids for treatment-resistant depression. They reviewed both animal studies and clinical trials involving compounds such as allopregnanolone, pregnenolone, and dehydroepiandrosterone (DHEA).
Their review emphasized the multi-target nature of neurosteroids. Unlike traditional drugs that modulate a single neurotransmitter, neurosteroids act broadly and rapidly. They enhance inhibitory signaling via GABA, regulate excitatory activity via NMDA, calm the stress response via the HPA axis, and stimulate the growth of new brain cells.
Notably, animal models of chronic stress—a common stand-in for depression in laboratory studies—show marked improvements in behavior and brain structure when treated with neurosteroids. These findings are echoed in human trials, where neurosteroids produced fast-acting and sustained antidepressant effects in individuals who had failed to respond to standard treatments.
Nagpurkar and her team argue that neurosteroids represent a paradigm shift—not just a new class of drugs, but a new way of understanding and addressing the biology of depression.
The Future of Neurosteroid Therapy
Despite the excitement, neurosteroid research is still in its early days. While brexanolone and related compounds offer proof-of-concept, many questions remain. How safe are neurosteroids with long-term use? How do their effects vary across age, sex, and hormonal states? Can they be combined with existing therapies to enhance outcomes?
Researchers are also exploring synthetic neurosteroid analogs—molecules designed to mimic the effects of natural neurosteroids but with better absorption, stability, and affordability. Drugs like zuranolone are currently being tested in large-scale clinical trials for a range of conditions, including major depressive disorder (MDD), PPD, and even bipolar depression.
At the same time, scientists are exploring whether neurosteroids could help with other mental health conditions linked to stress and neurochemical imbalance, such as anxiety disorders, post-traumatic stress disorder (PTSD), and schizophrenia.
A Glimpse into a New Era
For too long, psychiatry has relied on a limited toolkit, with treatments that work for some but not for all. The discovery and harnessing of neurosteroids represent more than just a new option—they offer a vision of personalized, biologically grounded care that responds to the brain’s complex needs in real time.
Depression may never be fully eradicated. But for those who have suffered in silence, for whom every day is a struggle against a relentless, invisible weight, neurosteroids offer something medicine rarely promises: hope backed by biology.
As we stand at the edge of a new era in neuroscience and mental health, one thing is clear—our brains have been carrying the seeds of healing all along. Now, we are finally learning how to listen.
Reference: Krutika Nagpurkar et al, Neurosteroids as emerging therapeutics for treatment-resistant depression: Mechanisms and clinical potential, Neuroscience (2025). DOI: 10.1016/j.neuroscience.2025.05.022.