For many women, a doctor’s visit is a mixed bag of relief and reluctance. There’s the hope of answers, the possibility of healing—but also the anxiety of baring intimate details to a near-stranger in a sterile room under fluorescent lights. Even with the best intentions, many women leave medical appointments with questions unanswered, symptoms minimized, or worse, dismissed. And the truth is: it’s not your fault.
Talking to your doctor about women’s health issues shouldn’t feel like navigating a maze. But it often does, especially when those issues are deeply personal—menstrual irregularities, sexual health, hormonal fluctuations, fertility struggles, menopause symptoms, or concerns about breast and pelvic health. Each of these topics touches not just on the physical but on the emotional and social dimensions of being a woman.
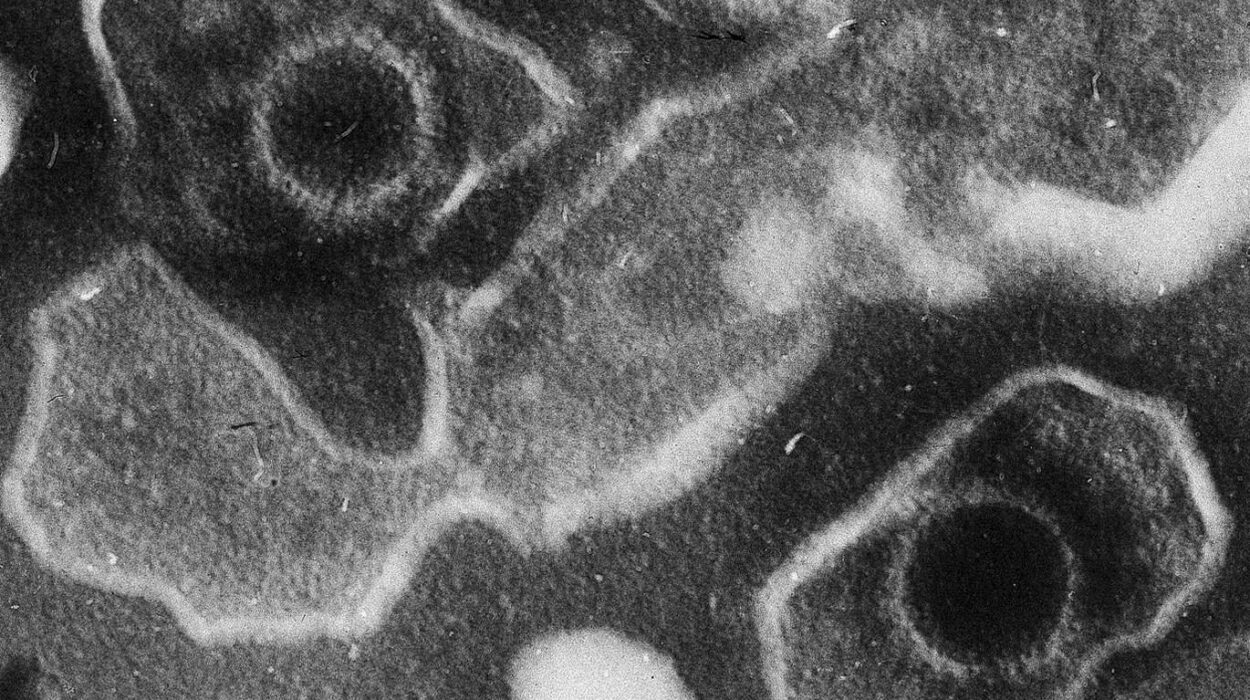
So why is it still so hard to talk about them? Part of the challenge lies in systemic gaps—research that’s only recently begun to focus more fully on female biology, doctors not always trained to listen with the kind of nuance women’s health demands, or the cultural scripts that have taught generations of women to downplay pain or put others first.
But here’s the good news: you can reclaim your voice in the exam room. You can build a partnership with your healthcare provider that centers your experiences, your instincts, and your concerns. It all begins with knowing how to talk about women’s health in a way that feels empowering, not overwhelming.
The Silent Epidemic of Being Dismissed
One of the most common experiences among women seeking care for health issues—particularly those involving chronic pain, fatigue, or reproductive symptoms—is being dismissed. Studies have consistently shown that women’s symptoms are more likely to be underestimated by doctors, especially when there’s no immediate or visible cause.
A woman may go to her doctor complaining of pelvic pain and be told it’s “just stress” or “normal for your age.” Another might describe debilitating periods only to be advised to take ibuprofen and wait it out. Others find their complaints are quickly funneled into catch-all diagnoses like “anxiety” without thorough investigation.
These experiences aren’t just frustrating—they’re harmful. Delayed diagnoses of conditions like endometriosis, polycystic ovary syndrome (PCOS), autoimmune diseases, or thyroid disorders can lead to long-term damage, not to mention emotional exhaustion. When a woman walks out of an appointment feeling unheard, it can discourage her from seeking help again.
The ability to advocate for your own health shouldn’t be a skill you’re forced to develop. But until medicine fully catches up with the lived reality of women, being able to speak clearly, confidently, and persistently about your health is a critical form of self-care.
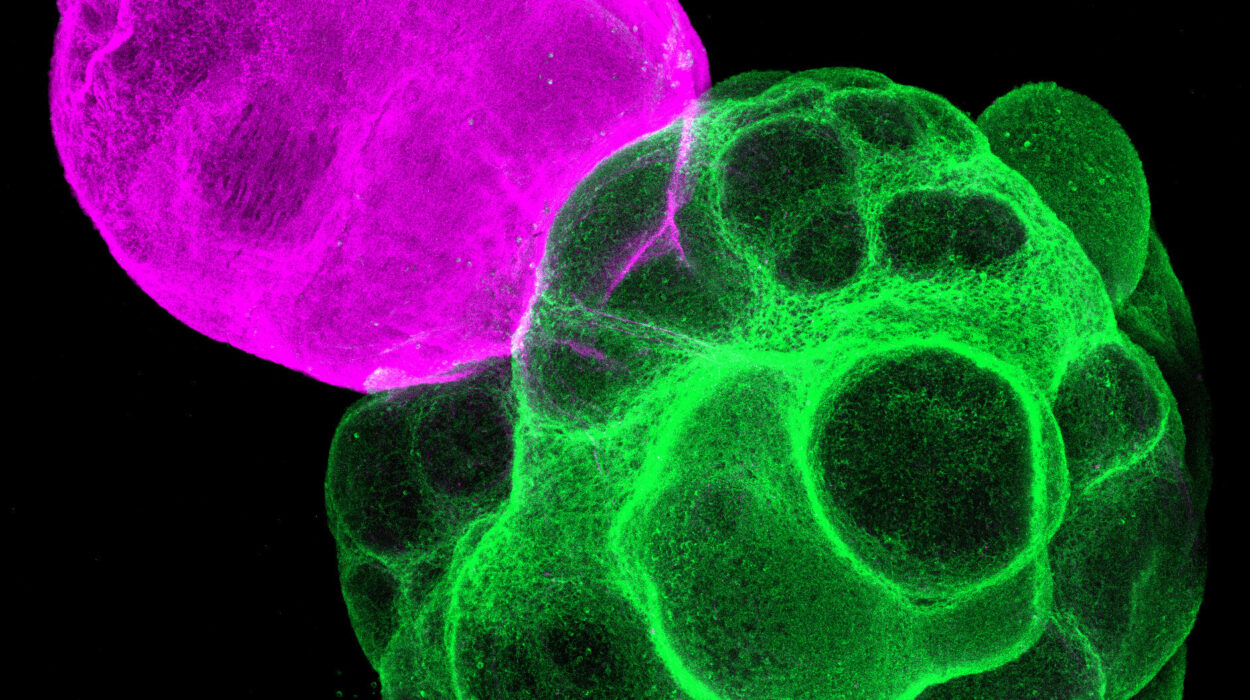
Knowing What’s Normal—And What Isn’t
A major hurdle in talking to your doctor about women’s health is simply knowing what to report. So much of women’s health exists in a fog of social taboos and half-truths. Period pain? That’s just part of being a woman. Mood swings? Must be hormones. Fatigue? Probably just being busy.
But many of the symptoms women are taught to brush off are actually signals worth exploring. Pain during sex isn’t “just part of aging.” Heavy periods that soak through multiple pads or tampons an hour aren’t something to normalize. Severe cramps that cause vomiting or make you miss work deserve investigation. Vaginal dryness, discharge changes, breast lumps, hair thinning, unexpected weight gain, skin changes—these are not mere inconveniences. They are data points your doctor needs to hear.
When you understand what your baseline is—what’s normal for your body—you become better equipped to notice when something is off. And when something is off, your voice matters. Sharing those changes clearly, even if they seem small or unrelated, gives your provider a fuller picture and a better chance of uncovering the root cause.
Preparing for the Appointment: Confidence Begins Before You Walk In
If you want your doctor to take your symptoms seriously, the first step is to take them seriously yourself. That starts long before the appointment.
Jot down your symptoms in a notebook or on your phone: when they started, how often they happen, how severe they are, and what seems to trigger or improve them. This kind of tracking is especially useful for cyclical symptoms—menstrual changes, mood fluctuations, migraines, or fatigue that follow a monthly pattern. It’s also helpful for digestive issues, headaches, joint pain, or anything that ebbs and flows.
Being able to say “I’ve had sharp pelvic pain on the left side that lasts 2–3 hours, usually mid-cycle, for the past four months” gives your doctor a clear path to investigate. It’s more powerful than saying “I get cramps sometimes.”
Also, think about what you want from the visit. Is it a diagnosis? A treatment plan? A second opinion? Knowing your own goals helps you stay focused, especially if the conversation gets sidetracked. If you’re nervous or forget things easily, bring a written list of questions or concerns. It’s not “extra”—it’s smart.
And yes, you’re allowed to bring someone with you. Whether it’s a partner, friend, or family member, a second set of ears can be invaluable, especially if you’re discussing complex or sensitive topics.
Breaking the Ice: Starting the Conversation
The first few moments of your doctor’s visit set the tone for the entire interaction. Yet many women feel pressured to stay polite, agreeable, or vague. But this isn’t a dinner party—it’s your health. If your doctor starts with “How are you?” and you automatically reply “Fine,” that’s an open door closing before it even starts.
Instead, open with honesty. Try: “I’m actually here because I’ve been feeling really off lately, and I’d like to go over some symptoms that have been worrying me.” Or, “I’ve noticed changes in my cycle that I don’t think are normal, and I’d like your input.”
Be direct but respectful. Most providers want to help, but they’re also human. They may miss things if you’re too vague. Don’t be afraid to say, “I want to talk about something that’s a little uncomfortable but important to me.” That one sentence can reset the power dynamic and make space for deeper dialogue.
Describing Symptoms Clearly and Effectively
One of the most useful things you can do in any medical conversation is learn how to describe your symptoms. Think like a detective: the more details you provide, the better your doctor can figure out what’s going on.
Start with what the symptom is, when it started, and how often it occurs. Then add how it feels, what it prevents you from doing, and what you’ve tried to relieve it. If it’s pain, describe the quality: sharp, dull, burning, cramping, stabbing? Is it constant or intermittent? Does it radiate or stay in one place?
Let’s say you’re dealing with painful intercourse. Instead of saying “Sex hurts,” say, “I’ve been having sharp pain during penetration, especially in the lower abdomen, for the past six months. It started gradually but has gotten worse. It’s affecting my relationship and making me anxious about intimacy.” That gives your doctor much more to work with.
Similarly, if you’re struggling with mood swings, frame it in terms of impact: “I’ve been feeling extremely irritable and weepy about a week before my period, and it’s making it hard to function at work or be present with my kids.”
You’re not exaggerating—you’re illuminating. Your job is to make the invisible visible.
The Emotional Side of Women’s Health
One of the most overlooked parts of any health discussion is how symptoms make you feel—not just physically, but emotionally. This is especially true for women’s health issues, which often intersect with identity, body image, sexuality, fertility, and personal history.
Don’t downplay this. If irregular periods are making you feel anxious about fertility, say so. If hormonal acne is crushing your self-esteem, let your doctor know. If vaginal dryness is making sex painful and affecting your relationship, bring it up. These things matter. They are part of your health, not separate from it.
Doctors are trained to treat conditions, but many forget that conditions live inside people. When you share the emotional weight of your experience, it helps them treat you as a whole person—not just a body with symptoms.
When the Doctor Doesn’t Listen
Unfortunately, not every doctor will meet your openness with the care and attention it deserves. If you feel rushed, dismissed, or patronized, it’s okay to push back—respectfully, but firmly.
Try saying: “I understand you’re pressed for time, but I don’t feel like my concerns are being fully heard. I’d really appreciate a few more minutes to explain.” Or, “I’ve done some research on this and I believe it’s worth exploring further. Can we talk about next steps?”
You’re not being difficult—you’re being proactive. If a doctor repeatedly interrupts you, brushes off your symptoms, or suggests it’s “all in your head,” that’s not a sign you’re being dramatic. It’s a sign that you may need a second opinion.
You are allowed to change doctors. You are allowed to ask for referrals. You are allowed to find someone who takes your health as seriously as you do.
Talking About Sex, Menstruation, and Menopause Without Shame
There are few topics more loaded than sex, menstruation, and menopause. And yet they affect nearly every woman, often in ways that are unpredictable, uncomfortable, or downright confusing.
If you’re struggling with low libido, painful sex, changes in orgasm, or feelings of disconnection during intimacy, your doctor needs to know. These symptoms could be hormonal, neurological, emotional, or side effects of medications. But they are not “just part of aging.” Nor are they trivial.
The same goes for period-related issues. Heavy bleeding, irregular cycles, skipped periods, severe PMS, or bleeding between periods—these are not merely nuisances. They can signal deeper issues and deserve proper evaluation.
Menopause, too, is often treated as a punchline in pop culture, but the reality is far more complex. Hot flashes, night sweats, mood swings, brain fog, bone loss, and vaginal changes are all valid medical concerns. Hormone replacement therapy, lifestyle interventions, and non-hormonal treatments can make a massive difference—but only if you ask.
There is no shame in any of this. These experiences are part of your biology, and bringing them into the light is a revolutionary act of self-respect.
The Role of Cultural, Racial, and Gender Bias in Women’s Health
Not all women experience the healthcare system the same way. Women of color, LGBTQ+ individuals, and those from marginalized communities often face added layers of bias and barriers to care. Studies have shown that Black women, in particular, are more likely to have their pain underestimated, their symptoms ignored, or their health concerns brushed aside.
Understanding that these biases exist isn’t about placing blame—it’s about protecting yourself. If you belong to a group that has historically been marginalized, it’s even more vital to speak clearly, document your symptoms, and advocate persistently. Allies can help—whether it’s a trusted friend in the room or a culturally competent provider who understands the nuances of your identity and experience.
You deserve care that honors your full humanity.
Making the Most of Follow-Up and Long-Term Care
Talking to your doctor about a women’s health issue isn’t a one-time event—it’s part of a longer journey. Whether you receive a diagnosis, start a treatment plan, or need ongoing monitoring, make sure you understand the next steps.
Before you leave, ask: “What are we doing next? When should I follow up? What signs should I watch for?” Take notes or ask for written instructions. If lab work is ordered, ask when and how results will be communicated. If medications are prescribed, ask about side effects, interactions, and alternatives.
And remember—your doctor works for you. If something isn’t working, speak up. If your symptoms change or worsen, check back in. If new questions arise, write them down. Health is a dynamic process, and you are the central player.
Claiming Your Seat at the Table
Women’s health deserves attention, research, funding, and respect. But until every exam room becomes a place where women are fully heard, it’s essential to bring your voice, your questions, and your determination.
Talking to your doctor about women’s health issues is not always easy—but it is always worth it. You are your own best advocate. You are not too sensitive, too anxious, too complicated, or too much.
You are exactly the expert your body has been waiting for.