When it comes to health care, there’s a tendency to think in reactive terms—people often seek help when something goes wrong. But for women, whose bodies experience constant shifts from puberty to menopause and beyond, waiting for symptoms to appear is like trying to fix a roof after the storm. Preventive care isn’t an optional luxury; it’s the foundation of long-term wellness. It’s about staying ahead of disease, protecting future fertility, safeguarding mental health, and addressing risk factors before they spiral into life-altering conditions.
Women face unique health challenges that require equally unique attention. From hormonal fluctuations and reproductive needs to higher risks of certain diseases like autoimmune disorders and osteoporosis, preventive care can mean the difference between a life of health and one defined by chronic conditions. And yet, countless women skip routine screenings, delay visits, or ignore symptoms because they’re too busy caring for others, burdened by costs, or unsure what to prioritize. That’s why understanding—and acting on—the critical importance of preventive care isn’t just a personal issue; it’s a societal imperative.
Understanding the Female Body’s Complexity
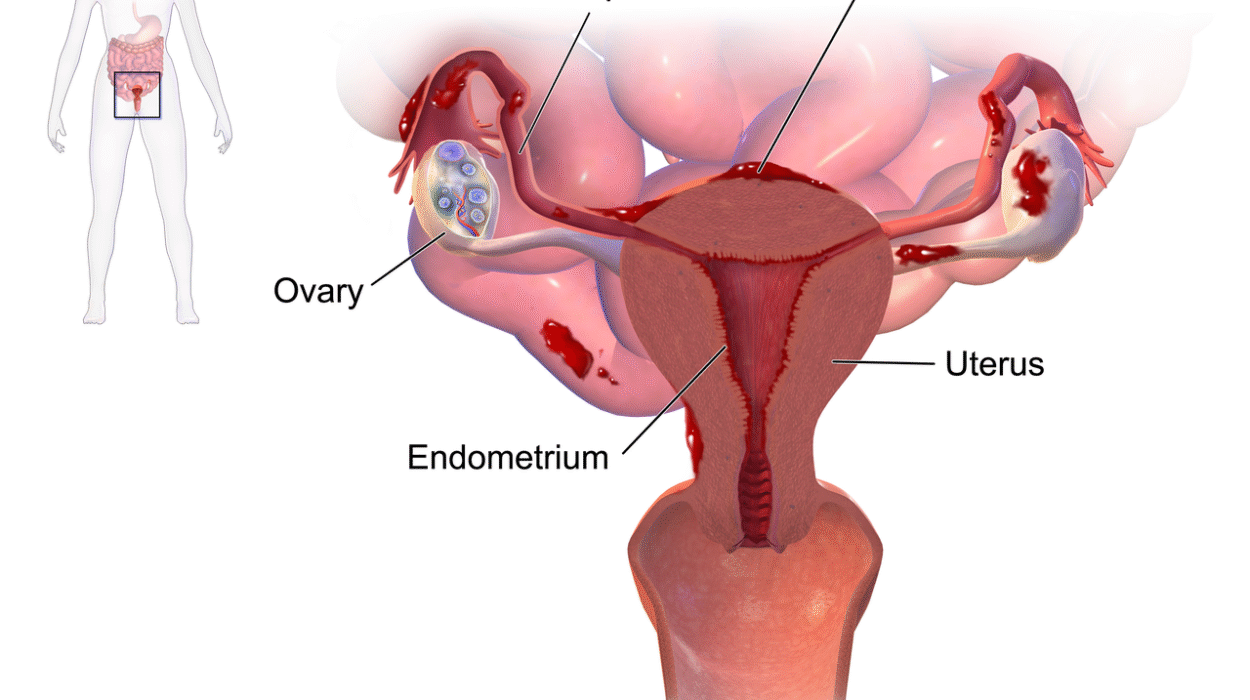
The human body is a marvel of biology, but the female body operates with a complexity that makes early detection and proactive care essential. From the onset of menstruation, a woman’s health is shaped by cycles and changes that influence not just fertility but cardiovascular health, bone density, and even mental well-being.
Hormones play a central role here. Estrogen, for example, is often thought of as just a reproductive hormone, but it affects everything from the skin to the brain to the heart. When hormonal imbalances occur—whether from polycystic ovary syndrome (PCOS), thyroid disorders, or menopause—they ripple across multiple systems. Preventive care offers a lens through which these disruptions can be monitored and managed before they wreak havoc.
Furthermore, women’s reproductive organs are home to some of the most common cancers—breast, cervical, ovarian, and uterine—and these often develop silently. The only defense is vigilance: regular pap smears, breast exams, and pelvic ultrasounds can catch issues in their earliest, most treatable stages. It’s not alarmist to say that preventive care saves lives. It’s a fact backed by decades of medical research.
The Cost of Delay: When Prevention Becomes Reaction
For many women, the first time they learn about an underlying health condition is during a crisis. A sudden collapse leads to the discovery of a heart condition. Unbearable pelvic pain finally results in a diagnosis of endometriosis. A routine pregnancy checkup uncovers dangerously high blood pressure. These moments of revelation are often met with disbelief: “Why didn’t I know sooner?” The truth is, the body whispers before it screams.
Preventive care exists to listen to those whispers. It’s not just about tests and bloodwork—it’s about building a long-term relationship with a healthcare provider who understands your personal baseline, who can notice subtle changes, and who works with you to mitigate risk. Skipping these visits might seem harmless in the short term, but over time, the consequences compound. Conditions that are easily treatable in their early stages—like pre-diabetes or precancerous cells—can become chronic, expensive, and even life-threatening if neglected.
The cost isn’t only personal. Society bears the burden too. Treating late-stage disease is far more expensive than preventing it. When women get sick, the ripple effects extend to families, workplaces, and entire communities. Children lose caregivers. Jobs lose leaders. Generations inherit the legacy of missed opportunities and preventable pain.
A Lifelong Approach to Wellness
Preventive care is not a one-time event or a single doctor’s visit. It’s a lifelong commitment, one that evolves with each phase of a woman’s life. In adolescence, it may begin with menstrual education and HPV vaccination. In the 20s and 30s, it includes reproductive planning, mental health support, and screenings for sexually transmitted infections. The 40s and 50s usher in mammograms, cholesterol checks, and perimenopausal care. Beyond that, bone density scans, heart health assessments, and cognitive screenings become essential.
Each decade brings its own health milestones and risks, which means care must be tailored to meet changing needs. What works for a college athlete navigating birth control may not suit a perimenopausal mother juggling work and caregiving. That’s why a personalized, proactive approach is so crucial. Preventive care allows for continuity, helping women track their health across time and make informed decisions that protect not just their current selves, but their future ones.
Mental Health Is Preventive Health
While physical health often takes center stage in medical care, mental health is a cornerstone of preventive wellness that can’t be ignored—especially for women, who are statistically more likely to experience depression, anxiety, PTSD, and eating disorders. Hormonal shifts play a major role here, but so do social and cultural factors: the pressure to balance work, family, appearance, and performance creates a toxic brew that can erode mental well-being over time.
Routine screenings for anxiety and depression, open conversations about stress and burnout, and access to therapy and support groups should be part of any preventive care plan. A woman’s mental health isn’t separate from her physical health—it shapes her ability to exercise, eat well, sleep, and advocate for her own needs. When mental health is neglected, everything else unravels. But when it’s supported, a woman’s resilience becomes her greatest asset.
Preventive mental health care means catching postpartum depression before it becomes debilitating. It means recognizing the early signs of burnout in caregivers. It means having providers who ask not just “How are your labs?” but also “How are you sleeping? How are you coping?” These conversations are as life-saving as any blood test.
Reproductive Autonomy and Preventive Power
Reproductive health is one of the most intimate and vital aspects of women’s health care. Yet it’s also one of the most politicized and misunderstood. Preventive care provides the foundation for reproductive autonomy—empowering women to understand their bodies, make informed choices about contraception, plan for (or prevent) pregnancy, and detect gynecological issues early.
Annual pelvic exams, pap smears, and STI screenings are more than routine—they’re protective. They catch infections before they spread, identify precancerous changes in the cervix, and open the door for early intervention. Contraceptive counseling, fertility assessments, and menstrual tracking all fall under the umbrella of preventive care, offering women the tools they need to shape their reproductive futures on their own terms.
This is not just about health—it’s about freedom. When women have access to consistent, evidence-based preventive reproductive care, they gain control over one of the most powerful aspects of their lives: their ability to create, avoid, or time pregnancy. And with that control comes greater economic stability, stronger partnerships, and healthier children.
Barriers to Access: The Hidden Cost of Inaction
Despite its importance, preventive care remains out of reach for far too many women. Financial barriers are a major obstacle—insurance may not cover certain screenings, or women may be uninsured altogether. Even when services are available, time, childcare, transportation, and language barriers can prevent women from seeking care. And then there’s the issue of trust.
Many women—particularly women of color, LGBTQ+ women, disabled women, and those from low-income communities—have had negative experiences with the healthcare system. They may feel unheard, dismissed, or disrespected. This creates a reluctance to seek care until absolutely necessary, which undermines the entire purpose of prevention.
Solving these issues requires more than outreach; it demands systemic change. Clinics must be accessible, affordable, and culturally competent. Healthcare providers must be trained to recognize bias, listen without judgment, and treat every patient with dignity. Policies must support paid leave for medical appointments, expand insurance coverage, and prioritize preventive services as essential, not optional.
Technology, Innovation, and the Future of Prevention
As the healthcare landscape evolves, so too do the tools available for preventive care. Wearable technology can now track menstrual cycles, detect irregular heart rhythms, and even predict stress levels. At-home tests make it easier to check hormone levels, fertility markers, and vitamin deficiencies. Telemedicine opens doors for rural women, busy moms, and those with limited mobility.
Genetic screening is also transforming the world of preventive care. Women can now assess their risk for diseases like breast cancer (via BRCA mutations), colon cancer, and more—allowing for earlier interventions or even preventative surgeries. The future of medicine is personalized, and preventive care is at the heart of it.
But technology is only as good as the system that delivers it. Data must be protected. Tools must be accurate and accessible. And women must be educated about how to interpret results, follow up appropriately, and navigate the options available to them. Technology can empower, but only if it is used to close gaps rather than widen them.
Empowerment Through Education
One of the most powerful tools in preventive care is education. When women understand their bodies, recognize warning signs, and know their options, they become active participants in their own health journey. This isn’t about memorizing medical terminology—it’s about creating a culture of health literacy that starts early and spans a lifetime.
Too often, girls grow up with shame, fear, or misinformation about their own anatomy. They may not know what a pap smear is or why breast self-exams matter. They may assume painful periods are normal or ignore signs of depression because no one ever told them otherwise. Preventive care begins with conversation, and those conversations need to happen in homes, schools, clinics, and communities.
When a woman walks into a doctor’s office knowing what to ask, what to expect, and how to follow through, she is not just a patient—she is an advocate. And when women advocate for themselves, families flourish, communities strengthen, and futures transform.
A Call to Action: Prevention Is Power
Preventive care is not a passive process. It requires action—appointments scheduled, questions asked, blood drawn, screenings done. It takes time, courage, and sometimes a fight to be taken seriously. But it is a fight worth having. Because behind every preventive visit is a woman who’s choosing to honor her body, her life, and her future.
Health is not something that simply happens to us. It is built, step by step, through the choices we make and the systems we create. For women, preventive care is both shield and sword—protecting against illness and empowering against inequality. It is personal and political. Scientific and spiritual. Routine and revolutionary.
The next time you think of skipping that checkup, delaying that mammogram, or ignoring that nagging symptom, remember this: Your health is your birthright. And preventive care is how you claim it.