If you could peek behind the curtain of your daily moods, your sleep quality, your metabolism, your menstrual cycle, your skin, and even your appetite, you’d discover a world of microscopic chemical messengers busily running the show. These unsung heroes are hormones—tiny molecules that wield enormous power. They travel through your bloodstream, acting as internal messengers between organs, tissues, and cells, orchestrating nearly every function in the body.
For women, hormones aren’t just a biological afterthought—they’re center stage, involved in everything from puberty to pregnancy, from energy to emotional balance, and from sex drive to skin clarity. Yet, they’re often misunderstood, underestimated, or treated as nuisances only noticed when things go haywire. But hormones aren’t villains; they’re intricate parts of your biology with a deeply human story. Understanding them is the first step in reclaiming your health, your mood, and maybe even your peace of mind.
A Symphony of Signals
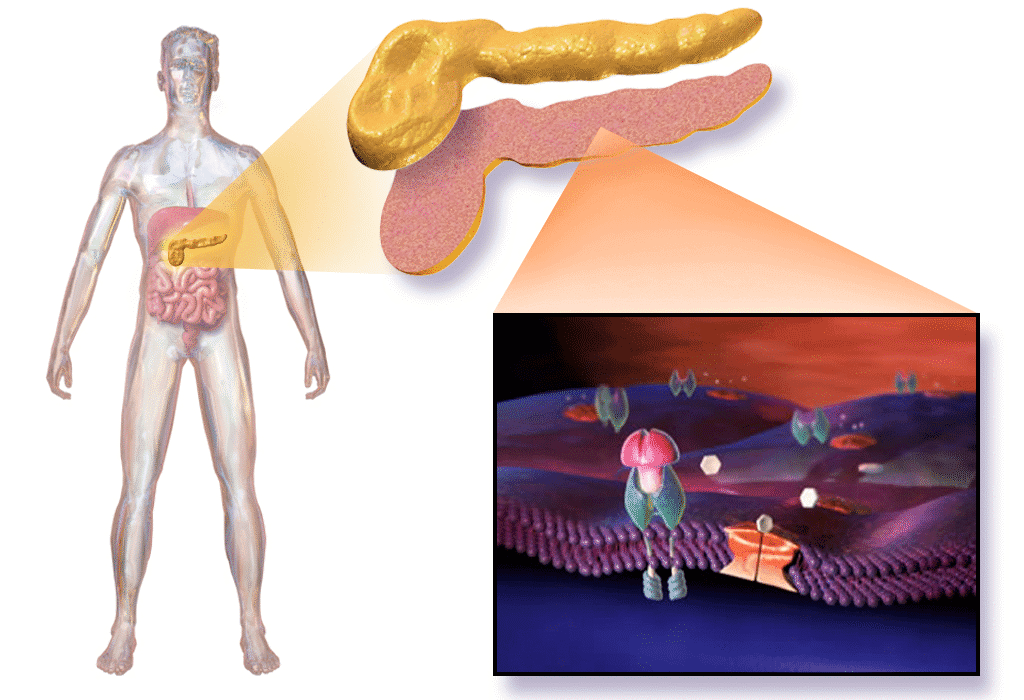
Think of your body as a vast orchestra, and your hormones as the conductors. Each one plays a specific role, and together, they must stay in sync for the music—your health—to sound right. The primary conductors come from glands within your endocrine system. The pituitary gland, thyroid, adrenal glands, pancreas, and ovaries are all key players, working together with astonishing precision.
These glands release hormones into your bloodstream, guiding everything from how fast your heart beats to when your next menstrual cycle begins. And while men have hormones too, women’s hormonal systems are more dynamic and cyclical. This rhythmic ebb and flow is beautiful, essential, and—yes—sometimes maddening. The female hormonal landscape isn’t static. It’s in constant dialogue with life’s stages: puberty, menstruation, pregnancy, perimenopause, and menopause.
The Hormonal Blueprint of Womanhood
From the moment a female embryo develops in the womb, hormones begin laying the foundation for the complex biological processes that define womanhood. Estrogen and progesterone—the two star players of the female reproductive system—begin their influence long before puberty arrives. But it’s during adolescence that hormones step onto center stage, triggering the profound transformations of puberty: breast development, menstrual cycles, pubic hair, and emotional changes that often feel seismic.
Estrogen, often dubbed the “female hormone,” is not just about reproduction. It helps regulate mood, keeps bones strong, protects the heart, and even influences skin elasticity and brain function. Progesterone, meanwhile, is the calming counterpart, working closely with estrogen to maintain balance. It prepares the body for pregnancy, helps regulate sleep, and has a soothing effect on the nervous system.
But estrogen and progesterone don’t work alone. Testosterone—yes, women have it too—plays a role in muscle strength, libido, and cognitive sharpness. Then there’s cortisol, the stress hormone; insulin, the blood sugar regulator; and thyroid hormones, which keep your metabolism humming. The point is, hormones don’t exist in silos. They’re interconnected in a delicate web, each influencing the others.
The Monthly Cycle: A Hormonal Dance
Every month, a woman’s body engages in a complex, choreographed performance called the menstrual cycle. This isn’t just about ovulation or periods; it’s about a dynamic hormonal dance that affects mood, appetite, energy, and even how your brain processes information.
The cycle begins with menstruation, as estrogen and progesterone levels drop and the uterine lining sheds. As the new cycle starts, estrogen rises, bringing with it a sense of vitality and confidence for many women. Mid-cycle, a surge in luteinizing hormone (LH) triggers ovulation—the release of an egg. Progesterone then takes the lead in the second half of the cycle, calming the body and preparing it for a potential pregnancy. If fertilization doesn’t occur, hormone levels dip, and the cycle begins anew.
This cycle influences much more than reproductive ability. It can affect sleep patterns, immune function, skin clarity, and even your ability to tolerate stress. Understanding the phases of your hormonal cycle is like having a roadmap to your body—one that can help you optimize your work, workouts, and self-care.
Hormonal Imbalances: When the Signals Go Wrong
While the hormonal system is exquisitely designed, it’s also vulnerable. Modern life—with its chronic stress, processed foods, lack of sleep, and environmental toxins—can throw hormonal harmony into disarray. And when hormones go out of balance, the symptoms can be confusing, frustrating, and deeply disruptive.
Hormonal imbalances can present in many ways: irregular periods, intense PMS, fatigue, acne, anxiety, weight gain, hair thinning, brain fog, or low libido. Because hormones are interconnected, a disruption in one can create a domino effect. For instance, high stress can cause elevated cortisol, which then disrupts progesterone, leading to cycle irregularity or sleep issues. Insulin resistance can affect testosterone levels, triggering symptoms like acne or excess facial hair, as seen in conditions like polycystic ovary syndrome (PCOS).
What makes hormonal imbalances tricky is that they often masquerade as other conditions—or worse, they’re dismissed as “normal” parts of womanhood. But feeling exhausted, moody, or in pain isn’t normal. It’s a sign your body is trying to tell you something.
PCOS, Endometriosis, and Other Hormonal Conditions
Some women experience more chronic and severe forms of hormonal disruption, often due to underlying medical conditions. PCOS is one of the most common, affecting up to 10% of women of reproductive age. It’s marked by irregular periods, elevated androgens (male hormones), and cysts on the ovaries. Women with PCOS often experience insulin resistance, weight gain, acne, and fertility challenges.
Endometriosis is another hormone-sensitive condition where tissue similar to the uterine lining grows outside the uterus, leading to pain, heavy periods, and sometimes infertility. While its root causes are still being studied, estrogen dominance plays a significant role.
Thyroid disorders—whether it’s hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid)—are also common in women, particularly during times of hormonal transition like pregnancy or perimenopause. These conditions can lead to fatigue, depression, weight changes, and more.
Understanding and managing these conditions often requires a multi-faceted approach: hormonal testing, lifestyle adjustments, and sometimes medication. But most importantly, it requires being heard, understood, and empowered with information.
Hormones Through the Decades
Hormonal health evolves with age, and each decade brings its own set of shifts and surprises. In your 20s and 30s, your hormones are typically at their peak. Fertility is at its highest, but so is the susceptibility to issues like PMS, PCOS, and stress-related imbalances. The focus during this time is often on cycle regulation, fertility awareness, and stress management.
Your 40s usher in the beginning of hormonal fluctuations associated with perimenopause. Estrogen and progesterone start to decline, and their imbalance can cause mood swings, irregular periods, sleep disturbances, and hot flashes. Perimenopause can last anywhere from a few years to a decade, making it one of the most misunderstood stages in a woman’s life.
By the time menopause officially sets in—defined as twelve months without a period—estrogen and progesterone are at their lowest levels. This hormonal drop can affect everything from bone density to vaginal health to memory. But menopause isn’t an ending. It’s a hormonal recalibration. With the right support, this stage can be one of liberation, strength, and self-discovery.
The Mind-Body-Hormone Connection
One of the most fascinating aspects of hormones is how deeply they intertwine with mental health. The stereotype of the “hormonal woman” is not only offensive—it’s misleading. Hormones don’t make women irrational; they make them biologically responsive to their internal and external environments.
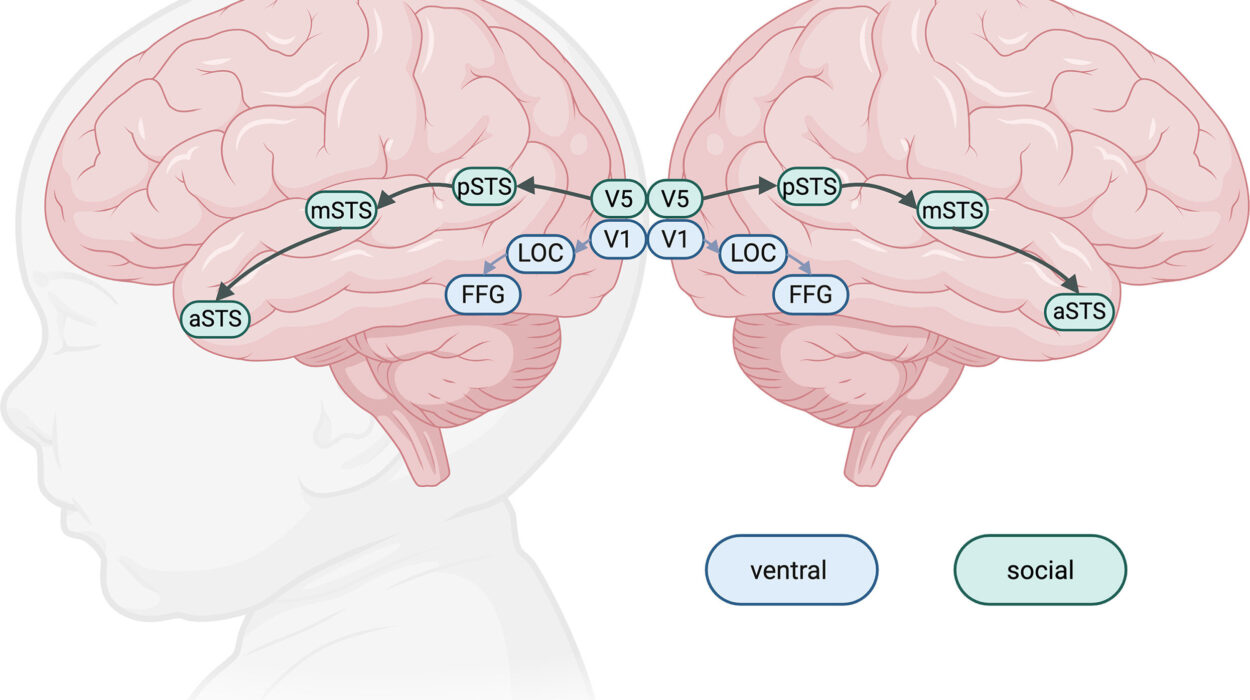
Estrogen and progesterone both have profound effects on the brain. Estrogen boosts serotonin and dopamine, two neurotransmitters associated with happiness and motivation. Progesterone, when in balance, has a calming, anti-anxiety effect. But when these hormones swing—like in PMS, postpartum, or perimenopause—the result can be mood disorders, anxiety, or depression.
Women are also more prone to anxiety and depression during times of hormonal transition. Postpartum depression is not a character flaw—it’s a hormonal crash. Premenstrual dysphoric disorder (PMDD), a severe form of PMS, is rooted in sensitivity to natural hormonal changes. Recognizing these conditions as biological, not emotional weaknesses, is crucial for proper support and treatment.
Lifestyle and Hormonal Harmony
The good news is that lifestyle plays a powerful role in hormone health. Nutrition, sleep, stress management, and movement aren’t just wellness buzzwords—they’re hormone regulators.
A diet rich in whole foods, healthy fats, fiber, and antioxidants supports liver function (which helps detox excess estrogen), blood sugar balance (key for insulin and testosterone), and gut health (which is now known to influence estrogen levels via the estrobolome—gut bacteria that metabolize estrogen).
Sleep is another cornerstone. Hormones like melatonin, cortisol, and growth hormone all follow circadian rhythms. Poor sleep disrupts this natural flow, leading to weight gain, mood issues, and fatigue.
Stress is perhaps the most potent hormone disruptor. Chronic stress leads to elevated cortisol, which suppresses reproductive hormones, disrupts thyroid function, and creates a cascade of imbalances. Practices like mindfulness, deep breathing, and even simply saying no can have tangible hormonal benefits.
Hormone Testing and Medical Support
Despite their central role in health, hormones are notoriously under-tested and poorly understood in mainstream medicine. Too often, women are told their symptoms are “just stress” or “just getting older.” But comprehensive hormone testing—whether through blood, saliva, or urine—can provide invaluable insights.
Testing can assess levels of estrogen, progesterone, testosterone, DHEA, cortisol, insulin, thyroid hormones, and more. It can uncover imbalances, track patterns, and help tailor treatment. In some cases, hormone replacement therapy (HRT), bioidentical hormones, or targeted supplements may be recommended. But these interventions should always be individualized and guided by a knowledgeable practitioner.
Reclaiming the Hormone Conversation
For too long, hormonal health has been shrouded in mystery, stigma, or simplification. Women have been taught to fear their hormones or suffer through their fluctuations. But knowledge is power. Understanding your hormonal rhythms isn’t about controlling your body—it’s about working with it.
Talking openly about hormones, tracking your cycle, asking for the right tests, and demanding holistic care are acts of self-advocacy. So is listening to your body and honoring what it tells you. Whether you’re navigating your first period or your last, pregnant or not, hormonally sensitive or in balance—your hormones are speaking. Learning their language is one of the most empowering things you can do for your health.
The Future of Female Hormone Health
As awareness grows, the future of women’s hormonal health is looking brighter. Research is expanding, and new diagnostic tools are emerging. From wearable fertility trackers to AI-driven hormone apps, technology is helping women connect the dots between their symptoms and their cycles.
But perhaps the most powerful shift is cultural. More women are sharing their stories. More practitioners are specializing in female hormone health. More attention is being paid to the female body not just as a reproductive system, but as a whole, dynamic, intelligent ecosystem.
The truth is, hormones matter. They matter deeply. They’re not just about menstruation or menopause. They’re about vitality, creativity, intimacy, cognition, and longevity. And when women understand their hormones, they don’t just feel better—they reclaim their power.