Breathing is so natural that most of us hardly notice it. With every inhalation, life itself flows into our bodies; with every exhalation, we release what no longer serves us. But for millions of people living with Chronic Obstructive Pulmonary Disease (COPD), this simple act of breathing becomes a daily battle. COPD is not just a medical condition—it is a life-altering reality that affects how people move, work, sleep, and even dream.
COPD is one of the leading causes of illness and death worldwide. According to the World Health Organization (WHO), it is among the top three causes of death globally, affecting more than 300 million people. It often develops silently over decades, creeping into lives with a cough that won’t go away, shortness of breath that grows worse with time, and fatigue that makes even small tasks exhausting.
And yet, despite its prevalence and severity, COPD is still misunderstood, often underdiagnosed, and frequently underestimated. To truly grasp the burden of COPD, we must dive deeply into its causes, symptoms, diagnostic methods, treatments, and the human stories behind the medical facts.
What Exactly is COPD?
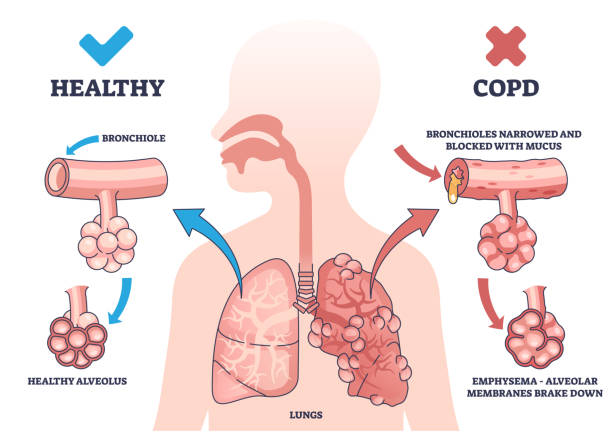
Chronic Obstructive Pulmonary Disease is not a single illness but a group of progressive lung diseases that obstruct airflow, making it increasingly difficult to breathe. The two primary conditions that fall under COPD are:
- Chronic bronchitis, where the airways become inflamed and produce excess mucus, leading to persistent cough and difficulty in clearing the air passages.
- Emphysema, where the alveoli (tiny air sacs in the lungs responsible for oxygen exchange) are damaged, reducing the surface area available for breathing.
Most people with COPD have a mixture of both conditions, though one may be more dominant than the other. What unites them is that the damage is progressive—it gets worse over time—and irreversible, though treatments can slow its progression and improve quality of life.
Causes of COPD: Why Does It Happen?
COPD does not strike at random; it develops from a combination of long-term exposure to irritants and individual susceptibility. The leading causes include:
Smoking: The Primary Culprit
Cigarette smoking is responsible for up to 90% of COPD cases in developed nations. Every puff introduces thousands of chemicals into the lungs, many of which inflame and scar delicate tissues. Over years of smoking, the body’s defense mechanisms weaken, leading to chronic airway damage.
But smoking is not the only form of tobacco linked to COPD. Pipe smoking, cigar smoking, and even secondhand smoke can contribute significantly. In some regions, exposure to smoke from burning biomass fuels for cooking and heating is a major risk factor, particularly for women.
Occupational and Environmental Exposures
Long-term exposure to dust, fumes, and chemicals in workplaces—such as in mining, construction, or agriculture—can injure the lungs. Urban air pollution, though a smaller contributor, can worsen symptoms and accelerate disease progression in those already affected.
Genetic Factors: The Role of Alpha-1 Antitrypsin Deficiency
A small but important number of people develop COPD due to a genetic disorder called Alpha-1 Antitrypsin Deficiency (AATD). Alpha-1 antitrypsin is a protein that protects the lungs from damage caused by enzymes released during inflammation. Without enough of it, lungs are vulnerable to early and aggressive forms of emphysema—even in nonsmokers.
Repeated Lung Infections in Childhood
Severe respiratory infections in early childhood can impair lung growth and resilience, increasing the risk of COPD later in life.
Aging and Declining Lung Function
As we age, lung capacity naturally declines. In people exposed to harmful irritants or with genetic predispositions, this decline can become severe enough to cross into COPD territory.
Symptoms of COPD: When Breathing Becomes a Struggle
COPD often starts quietly, with symptoms so mild they are brushed aside as “just getting older” or “a smoker’s cough.” But over time, they worsen, eroding quality of life.
The Early Signs
- Chronic cough: Often worse in the morning, sometimes dismissed as a “smoker’s cough.”
- Sputum production: Thick, often difficult-to-clear mucus.
- Shortness of breath: At first only during exertion, like climbing stairs, but later even at rest.
Progression of Symptoms
As COPD advances, symptoms become harder to ignore:
- Persistent shortness of breath, even during light activity.
- Wheezing and tightness in the chest.
- Frequent respiratory infections, like colds or the flu, which last longer and hit harder.
- Fatigue, due to the extra energy spent just to breathe.
- Unintended weight loss in advanced stages, as eating and breathing simultaneously become difficult.
Exacerbations: Sudden Worsening
One of the most frightening aspects of COPD is the exacerbation, a sudden flare-up of symptoms often triggered by infections or environmental pollutants. During an exacerbation, patients may feel as if they are suffocating, requiring urgent medical attention. Repeated exacerbations accelerate lung damage and increase the risk of death.
How is COPD Diagnosed?
Early diagnosis is crucial for slowing COPD progression, but unfortunately, many cases go undiagnosed until the disease is advanced. Diagnosis typically involves a combination of history-taking, physical examination, and specific tests.
Medical History and Physical Examination
Doctors begin by asking about smoking history, exposure to pollutants, family history of lung disease, and symptoms. A stethoscope may reveal wheezing or crackling sounds in the lungs.
Spirometry: The Gold Standard
Spirometry is a simple, non-invasive breathing test that measures how much air a person can inhale and exhale, and how quickly they can do it. It can detect COPD even before symptoms become severe. The key measurement is the FEV1/FVC ratio (Forced Expiratory Volume in 1 second / Forced Vital Capacity). A reduced ratio indicates airflow obstruction.
Imaging Tests
- Chest X-rays: Can show emphysema, though often not in early stages.
- CT scans: Provide more detailed images and can detect emphysema and other lung problems earlier.
Blood Tests
In suspected cases of Alpha-1 Antitrypsin Deficiency, blood tests can confirm the genetic condition. Arterial blood gas analysis may be used in advanced COPD to measure oxygen and carbon dioxide levels in the blood.
Treatment of COPD: Managing, Not Curing
There is no cure for COPD, but treatment can significantly improve symptoms, slow disease progression, and enhance quality of life. Management involves a combination of lifestyle changes, medications, therapies, and in severe cases, surgery.
Lifestyle Modifications: The Foundation of Treatment
- Quitting smoking: The single most important step in COPD management. Quitting at any stage slows disease progression.
- Avoiding lung irritants: Reducing exposure to pollution, dust, and workplace chemicals.
- Healthy diet and exercise: Proper nutrition supports immune function, while regular activity strengthens respiratory muscles and reduces fatigue.
Medications
Medications are the cornerstone of COPD management:
- Bronchodilators: These relax the muscles around the airways, making it easier to breathe. They may be short-acting (for quick relief) or long-acting (for maintenance).
- Inhaled corticosteroids: Reduce airway inflammation and decrease the frequency of exacerbations.
- Combination inhalers: Contain both bronchodilators and steroids for greater effect.
- Phosphodiesterase-4 inhibitors: Reduce inflammation and relax airways in severe cases.
- Antibiotics: Used during exacerbations triggered by bacterial infections.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive program involving exercise training, nutritional counseling, education, and psychological support. It empowers patients to manage their symptoms, build stamina, and reclaim aspects of daily life they may have lost.
Oxygen Therapy
For patients with low blood oxygen levels, supplemental oxygen can be life-saving. Oxygen therapy improves survival, sleep, mood, and cognitive function.
Surgical Options
In severe, carefully selected cases, surgery may be considered:
- Lung volume reduction surgery: Removing damaged areas of lung to improve breathing efficiency.
- Lung transplant: For end-stage COPD when all other treatments fail.
The Emotional and Social Impact of COPD
Beyond its physical toll, COPD carries profound emotional and social consequences. The constant breathlessness can lead to anxiety, depression, and social isolation. Activities once taken for granted—playing with grandchildren, walking to the market, or even laughing without coughing—become challenging.
Caregivers, too, often feel the strain. Families must adjust to new routines, responsibilities, and the fear of exacerbations. Psychological support, counseling, and patient support groups play a vital role in addressing this hidden burden.
Living with COPD: Finding Strength in Adversity
Despite its challenges, many people with COPD find ways to live full and meaningful lives. Advances in treatment, support networks, and self-management strategies offer hope. Pulmonary rehabilitation programs often create communities of encouragement, where patients inspire one another with stories of resilience.
Mind-body practices like yoga, breathing exercises, and meditation can also help reduce stress and improve lung function. Some patients take up new hobbies, adapt their physical activities, or focus on creative outlets. The journey may be difficult, but it can also spark profound personal growth.
Preventing COPD: A Public Health Priority
Prevention is the most effective way to combat COPD. This means reducing exposure to risk factors at both the personal and societal level:
- Strong anti-smoking campaigns and policies.
- Safer workplace environments with reduced dust and chemical exposure.
- Clean cooking fuels and better ventilation in low-income countries.
- Early detection through spirometry screening for at-risk individuals.
By focusing on prevention, societies can save millions of lives and reduce the immense economic and healthcare burdens of COPD.
The Future of COPD Treatment: Emerging Horizons
Medical science is advancing rapidly, offering new hope for COPD patients:
- Regenerative medicine: Research into stem cells may one day repair damaged lung tissue.
- Targeted therapies: Precision medicine could tailor treatments to individual genetic and molecular profiles.
- Smart inhalers and digital monitoring: Technology is helping patients track symptoms, adherence, and exacerbations in real time.
- Novel drug therapies: Ongoing trials are exploring medications that could halt or even reverse lung damage.
While a cure remains elusive, these innovations hold promise for transforming COPD care in the coming decades.
Conclusion: Redefining Life with COPD
Chronic Obstructive Pulmonary Disease is more than a medical diagnosis—it is a lived experience, one that challenges every breath. It develops quietly, progresses relentlessly, and impacts not just lungs, but lives. Yet it is not without hope. With early detection, effective treatment, lifestyle changes, and emotional support, people with COPD can slow its progression and rediscover joy in life’s moments.
To understand COPD is to understand both the fragility and resilience of human life. It reminds us that breathing—something we so often take for granted—is a gift beyond measure. And for those living with COPD, each breath is not just survival; it is a triumph.