For centuries, tuberculosis (TB) has haunted humanity. Known in the past as “consumption” because of the way it seemed to waste the body away, TB has shaped history, claimed the lives of millions, and continues to challenge science and medicine even in the modern age. Despite medical advances, TB remains one of the world’s leading infectious killers, silently affecting millions each year, especially in vulnerable communities.
What makes tuberculosis such a relentless disease is not only its capacity to spread but also its deceptive nature. Some people carry the bacteria for years without showing symptoms, while others become gravely ill. It can be cured with the right treatment, yet drug resistance has turned it into a renewed global threat. To understand TB is to understand its causes, the way it manifests, how it is diagnosed, and the tools we have to fight it.
What Is Tuberculosis?
Tuberculosis is an infectious disease caused by a bacterium called Mycobacterium tuberculosis. This microorganism primarily affects the lungs but can also spread to almost any part of the body, including the brain, kidneys, and bones. Unlike many bacteria that cause short-term infections, M. tuberculosis has evolved to survive inside the human body for long periods, evading the immune system and creating a condition known as latent tuberculosis.
TB is spread through the air. When a person with active TB in the lungs coughs, sneezes, laughs, or even talks, tiny droplets carrying the bacteria are released into the air. Inhaling just a few of these droplets can expose another person to infection. However, not everyone who breathes in the bacteria becomes sick. Much depends on the strength of the person’s immune system and whether the bacteria remain dormant or become active.
The History of Tuberculosis
Tuberculosis is not a new enemy. Evidence of TB has been found in Egyptian mummies, dating back thousands of years. In Europe, the disease became infamous during the 18th and 19th centuries, reaching epidemic proportions in crowded, industrial cities. It was often romanticized in literature and art as the “disease of poets,” partly because it seemed to disproportionately affect creative figures such as John Keats and Frédéric Chopin.
The discovery of the TB bacterium in 1882 by German physician Robert Koch was a turning point in medical history. Koch’s work not only identified the cause of the disease but also paved the way for the development of microbiology as a field. Later, the introduction of antibiotics in the mid-20th century brought hope, dramatically reducing TB deaths in wealthy countries. Yet, the disease never truly disappeared. In the late 20th century, TB resurged, fueled by the HIV epidemic, poverty, and the rise of drug-resistant strains. Today, it remains a global health crisis.
Causes of Tuberculosis
At its core, tuberculosis is caused by Mycobacterium tuberculosis, but the story is more complex than a single microbe. Whether someone develops TB depends on a delicate interplay between biology, immunity, and social conditions.
The Bacterium: Mycobacterium tuberculosis
This bacterium is uniquely equipped for survival. Unlike many bacteria that are quickly destroyed by the body’s immune defenses, M. tuberculosis has a waxy outer coating made of mycolic acid. This protective shield allows it to resist destruction inside immune cells called macrophages. Instead of being digested, the bacteria can persist, hidden inside the very cells meant to kill them.
Over time, the immune system walls off the bacteria, forming small clusters of immune cells called granulomas. In many cases, this keeps the infection dormant—this is latent TB. But under certain conditions, such as weakened immunity, the bacteria can break free, multiply, and cause active disease.
Risk Factors
Not everyone exposed to TB develops active disease. Several factors increase the risk:
- Weakened immune system: HIV is the most significant risk factor, as the virus destroys immune defenses. Other conditions such as diabetes, malnutrition, or cancer treatments also weaken immunity.
- Living conditions: Crowded housing, poor ventilation, and poverty make transmission more likely.
- Age: Infants, young children, and the elderly are more vulnerable.
- Substance use: Smoking, alcohol abuse, and drug use impair the body’s ability to fight infection.
- Geography: TB is more common in certain parts of the world, including South Asia, Sub-Saharan Africa, and parts of Eastern Europe.
Symptoms of Tuberculosis
TB symptoms vary depending on whether the infection is latent or active, and which organs are affected.
Latent Tuberculosis
In latent TB, the person carries the bacteria but shows no symptoms. They cannot spread the disease, but they remain at risk of developing active TB later. It is estimated that about a quarter of the world’s population has latent TB.
Active Tuberculosis
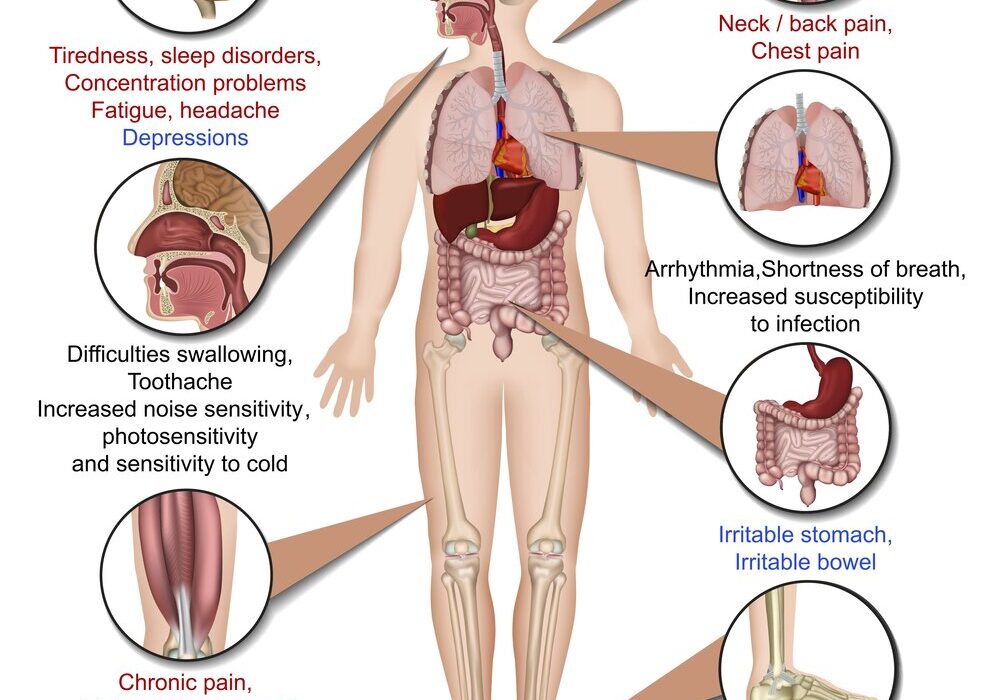
Active TB can be devastating if untreated. When it affects the lungs—pulmonary TB—the most common symptoms include:
- Persistent cough lasting more than three weeks
- Coughing up blood or sputum
- Chest pain or discomfort when breathing or coughing
- Fatigue and weakness
- Night sweats
- Fever and chills
- Unexplained weight loss and loss of appetite
When TB affects organs outside the lungs—extrapulmonary TB—symptoms depend on the site of infection. For example, TB of the spine can cause back pain, TB of the kidneys can cause blood in the urine, and TB of the brain can lead to headaches and neurological issues.
Diagnosis of Tuberculosis
Diagnosing TB is both an art and a science. Because its symptoms can mimic other diseases, accurate testing is essential.
Medical History and Examination
The process usually begins with a detailed medical history and physical examination. Doctors look for risk factors such as exposure to TB, travel history, or underlying health conditions.
Skin and Blood Tests
The tuberculin skin test (TST), also called the Mantoux test, involves injecting a small amount of TB protein under the skin. If the person has been exposed to TB, the site will swell within 48–72 hours. However, this test cannot distinguish between latent and active TB and may be less reliable in people who received the BCG vaccine.
Modern blood tests, such as interferon-gamma release assays (IGRAs), measure the immune system’s response to TB proteins. These tests are more specific and less affected by prior vaccination.
Imaging
Chest X-rays are a crucial tool for detecting pulmonary TB. They can reveal lesions, cavities, or other abnormalities caused by the infection.
Laboratory Tests
The gold standard for TB diagnosis is identifying the bacteria in sputum or tissue samples. Microscopic examination can reveal acid-fast bacilli, while advanced tests such as nucleic acid amplification (PCR) provide rapid and accurate results. Culturing the bacteria, though slower, is essential for confirming diagnosis and testing for drug resistance.
Treatment of Tuberculosis
Treating TB requires patience, precision, and persistence. Unlike many bacterial infections that can be cured in days, TB treatment takes months.
Standard Treatment
The cornerstone of TB treatment is a combination of antibiotics taken for at least six months. The most common first-line drugs are:
- Isoniazid
- Rifampicin (or Rifampin)
- Ethambutol
- Pyrazinamide
The typical regimen involves taking all four drugs for the first two months (intensive phase), followed by isoniazid and rifampicin for another four months (continuation phase). This combination ensures that the bacteria are killed completely and prevents relapse.
Challenges in Treatment
Adherence is the greatest challenge in TB treatment. Because the therapy is long and the side effects can be unpleasant, many patients stop early. This can lead to relapse and, worse, the development of drug-resistant TB.
To address this, many health systems use Directly Observed Therapy (DOT), where healthcare workers supervise patients taking their medication. This approach has improved treatment success rates worldwide.
Drug-Resistant TB
One of the most serious threats today is multidrug-resistant TB (MDR-TB), which does not respond to isoniazid and rifampicin, the two most powerful drugs. Treating MDR-TB requires second-line drugs that are more toxic, less effective, and require up to two years of therapy. Even more alarming is extensively drug-resistant TB (XDR-TB), which resists nearly all available treatments.
Supportive Care
Beyond antibiotics, TB patients often need supportive care, including good nutrition, management of side effects, and treatment for coexisting conditions such as HIV.
Prevention of Tuberculosis
Prevention is as vital as treatment in the global fight against TB.
- Vaccination: The Bacillus Calmette–Guérin (BCG) vaccine is widely used and protects children from severe forms of TB, though its effectiveness in preventing adult pulmonary TB is variable.
- Infection control: Ventilation, masks, and infection-prevention measures in hospitals and crowded settings reduce transmission.
- Preventive therapy: People with latent TB, especially those at high risk such as HIV-positive individuals, may be given antibiotics to prevent progression to active disease.
- Addressing social factors: Reducing poverty, improving living conditions, and ensuring access to healthcare are crucial for long-term TB control.
The Human Experience of Tuberculosis
TB is more than a medical condition—it is a human experience that carries stigma, isolation, and fear. In many societies, those diagnosed with TB are shunned, adding emotional suffering to physical illness. Patients often battle not only the bacteria but also the shame of being labeled contagious.
At the same time, the TB story is one of resilience. Survivors often describe the journey as one of transformation—enduring months of treatment, facing their vulnerabilities, and emerging with newfound strength. Health workers on the frontlines continue to fight tirelessly, bringing hope to patients in the most resource-limited settings.
The Global Burden of Tuberculosis
Despite progress, TB remains one of the top infectious killers worldwide, claiming over a million lives annually. The disease is most prevalent in low- and middle-income countries, where healthcare access is limited. The intersection of TB and HIV has been especially devastating in Africa, while Asia continues to bear the largest number of cases.
Global initiatives led by the WHO, governments, and non-profit organizations aim to reduce TB incidence through research, funding, and improved healthcare systems. The ultimate goal is to end TB as a public health threat, but achieving this requires not only medical advances but also social and political will.
The Future of Tuberculosis Treatment and Research
Research is ongoing to develop shorter, more effective treatments, new vaccines, and better diagnostic tools. Promising approaches include:
- New antibiotics that target resistant strains.
- Shorter drug regimens that improve adherence.
- Next-generation vaccines that provide stronger protection.
- Rapid diagnostic technologies that allow earlier detection.
The fight against TB is not just about science; it is about equity. Ensuring that new tools reach the communities most affected is essential for global progress.
Conclusion: A Disease That Demands Attention
Tuberculosis is a reminder of the fragile balance between humans and microbes. Despite being curable and preventable, TB continues to claim lives, particularly among the most vulnerable. Its persistence reflects not only biological resilience but also deep-rooted inequalities in our world.
To defeat TB, we need more than medicine—we need compassion, education, and commitment. We need to break down stigma, support patients, and ensure healthcare access for all. Above all, we must remember that behind every statistic is a human being longing for health, dignity, and a future free from this ancient disease.