The liver is one of the most remarkable organs in the human body. Tucked under the rib cage on the right side of the abdomen, it quietly works day and night, filtering blood, metabolizing nutrients, and detoxifying harmful substances. Without it, life would not be possible. Every morsel of food we eat, every sip of liquid we drink, and every medication we take passes through the liver in some form. It is the body’s natural chemical factory, tirelessly balancing, breaking down, and storing substances that sustain us.
Yet, despite its resilience, the liver is also vulnerable. Liver diseases can progress silently, often without noticeable symptoms until they are advanced. This quiet deterioration is why the liver is sometimes called the “silent organ.” Understanding liver disease—its causes, symptoms, methods of diagnosis, and treatment options—is crucial not only for those at risk but for anyone who values the foundation of health itself.
Understanding Liver Disease
The term “liver disease” does not refer to a single condition but rather an umbrella term that covers many disorders affecting the structure and function of the liver. Some are acute, appearing suddenly and severely, while others are chronic, developing over many years. What unites them all is the gradual breakdown of the liver’s ability to perform its vital tasks.
The liver has over 500 known functions, including:
- Producing bile to digest fats.
- Processing carbohydrates, proteins, and fats from food.
- Detoxifying drugs and toxins.
- Storing vitamins and minerals.
- Regulating blood clotting.
When disease disrupts these processes, the effects ripple across the entire body. This is why liver disease is not only a local problem in the liver but a systemic issue affecting overall health and well-being.
Causes of Liver Disease
The causes of liver disease are varied, but they generally fall into a few broad categories: infections, lifestyle factors, genetic disorders, autoimmune conditions, and toxic damage.
Viral Infections
Viruses are among the most common culprits behind liver disease. Hepatitis viruses—A, B, C, D, and E—are the most notorious. Each type spreads differently and has different impacts on the liver:
- Hepatitis A is often contracted through contaminated food or water. It usually causes an acute infection and rarely leads to long-term damage.
- Hepatitis B spreads through blood and bodily fluids. It can cause both acute and chronic disease, potentially leading to cirrhosis or liver cancer.
- Hepatitis C is primarily spread through blood contact, such as shared needles. It is a leading cause of chronic liver disease worldwide.
- Hepatitis D occurs only in individuals already infected with Hepatitis B, making the disease more severe.
- Hepatitis E, similar to Hepatitis A, spreads via contaminated water and is more common in developing regions.
These infections can inflame and scar the liver, reducing its capacity to function.
Alcohol-Related Liver Disease
Alcohol is metabolized in the liver, but excessive and prolonged drinking overwhelms the organ’s detoxification ability. This can cause a spectrum of damage:
- Fatty liver, where fat accumulates in the cells.
- Alcoholic hepatitis, an inflammation that can be severe and life-threatening.
- Cirrhosis, a stage where healthy tissue is replaced by scar tissue, permanently impairing liver function.
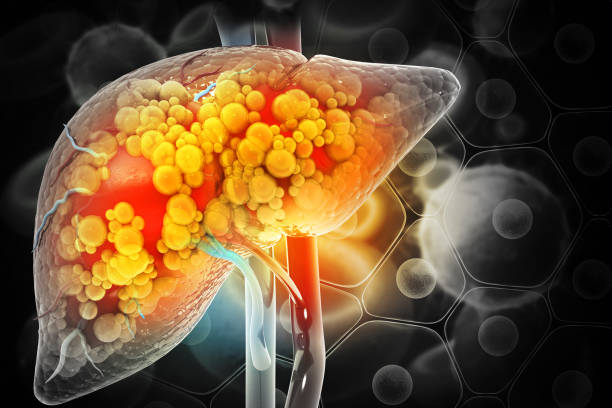
Non-Alcoholic Fatty Liver Disease (NAFLD)
As modern lifestyles become increasingly sedentary and diets more calorie-dense, NAFLD has emerged as a global epidemic. This condition occurs when fat builds up in the liver despite little or no alcohol consumption. In some people, this progresses to non-alcoholic steatohepatitis (NASH), where inflammation and scarring occur. Left unchecked, NASH can advance to cirrhosis and liver cancer.
Genetic Disorders
Some individuals inherit conditions that affect the liver:
- Hemochromatosis causes excessive iron buildup.
- Wilson’s disease leads to copper accumulation.
- Alpha-1 antitrypsin deficiency results in abnormal protein deposits in the liver.
Though rare, these disorders demonstrate how small genetic mutations can have devastating impacts.
Autoimmune Liver Diseases
In some cases, the body’s immune system mistakenly attacks the liver, leading to autoimmune hepatitis. Other autoimmune conditions such as primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC) target the bile ducts, causing inflammation and scarring that eventually damage the liver.
Toxins and Medications
The liver processes most drugs and toxins, which makes it vulnerable to damage from overdose, prolonged use, or chemical exposure. For example, excessive acetaminophen (paracetamol) can cause acute liver failure, while long-term exposure to industrial chemicals can scar the liver.
Symptoms of Liver Disease
One of the most challenging aspects of liver disease is that it often progresses silently. In early stages, there may be no noticeable signs at all. However, as the disease advances, symptoms begin to emerge:
- Fatigue and general weakness.
- Jaundice, a yellowing of the skin and eyes caused by bilirubin buildup.
- Dark urine and pale stools due to bile processing issues.
- Abdominal pain or swelling, often from fluid buildup known as ascites.
- Swelling in the legs and ankles (edema).
- Itchy skin, caused by bile salt deposits.
- Loss of appetite, nausea, or unexplained weight loss.
- Easy bruising and bleeding, as the liver produces fewer clotting proteins.
In severe cases, liver disease can lead to confusion, memory loss, or disorientation—a condition called hepatic encephalopathy caused by toxins affecting the brain.
Diagnosis of Liver Disease
Diagnosing liver disease requires a combination of medical history, physical examination, laboratory tests, and imaging.
- Blood tests can measure liver enzymes, bilirubin, clotting ability, and protein levels. Elevated liver enzymes often signal inflammation or damage.
- Imaging techniques such as ultrasound, CT scans, or MRI provide detailed pictures of the liver’s structure.
- FibroScan, a specialized ultrasound, measures liver stiffness to assess scarring.
- Liver biopsy, though invasive, remains the gold standard for diagnosing many liver conditions. A small tissue sample is examined under a microscope to assess damage.
The diagnostic process is not only about identifying the disease but also understanding its stage and severity, which is crucial for guiding treatment.
Treatment of Liver Disease
Treatment depends on the underlying cause, the severity of the condition, and the overall health of the patient.
Lifestyle Modifications
For many liver diseases, lifestyle changes form the foundation of treatment. These may include:
- Eliminating alcohol completely.
- Losing weight and adopting a balanced diet rich in whole foods.
- Exercising regularly to reduce fat accumulation in the liver.
- Avoiding unnecessary medications or toxic exposures.
Medications
Medications can target specific causes:
- Antiviral drugs for hepatitis B and C.
- Steroids or immunosuppressants for autoimmune hepatitis.
- Chelation therapy to remove excess iron or copper in genetic disorders.
- Medications to control symptoms such as itching, fluid buildup, or confusion.
Procedures and Surgery
In some cases, advanced treatment is needed:
- Endoscopic procedures to manage complications such as varices (swollen veins in the esophagus).
- Liver resection to remove diseased portions.
- Liver transplantation, often the last option when the liver fails entirely. Transplants can save lives, but they come with challenges such as donor availability, cost, and the need for lifelong immunosuppression.
The Emotional and Human Impact of Liver Disease
Beyond biology, liver disease carries profound emotional and social consequences. Patients often grapple with fatigue, stigma, and uncertainty about the future. Families may struggle with the demands of care, the financial burden of treatments, or the fear of losing a loved one.
These human dimensions remind us that health is never just physical—it is emotional, social, and spiritual. Counseling, support groups, and compassionate medical care play vital roles in healing alongside medicine.
Preventing Liver Disease
The good news is that many liver diseases are preventable or manageable with early intervention. Vaccination against hepatitis A and B, practicing safe sex, avoiding sharing needles, moderating alcohol intake, maintaining a healthy weight, and exercising regularly all reduce risk. Regular health check-ups, especially for those with risk factors, can detect liver disease early before irreversible damage occurs.
The Future of Liver Health
Advances in science are bringing new hope. Antiviral therapies have turned hepatitis C from a chronic, life-threatening disease into a curable condition for many. Stem cell research and bioengineering raise the possibility of regenerating liver tissue in the future. Artificial liver support devices are under development, potentially bridging patients to transplant or recovery.
As medicine evolves, so does our understanding of how lifestyle, environment, and genetics interact in liver disease. Public health initiatives and global cooperation will remain essential in reducing the burden of these conditions worldwide.
Conclusion: Protecting the Guardian
The liver is more than an organ—it is a guardian, silently protecting us from within. Liver disease threatens this balance, often quietly and progressively. By understanding its causes, recognizing its symptoms, advancing diagnostic tools, and applying effective treatments, we can protect this vital organ and preserve the rhythm of life it sustains.
Ultimately, the story of liver disease is not just one of biology, but of resilience and hope. With awareness, compassion, and scientific progress, we can turn the tide against liver disease and honor the silent guardian that keeps us alive.