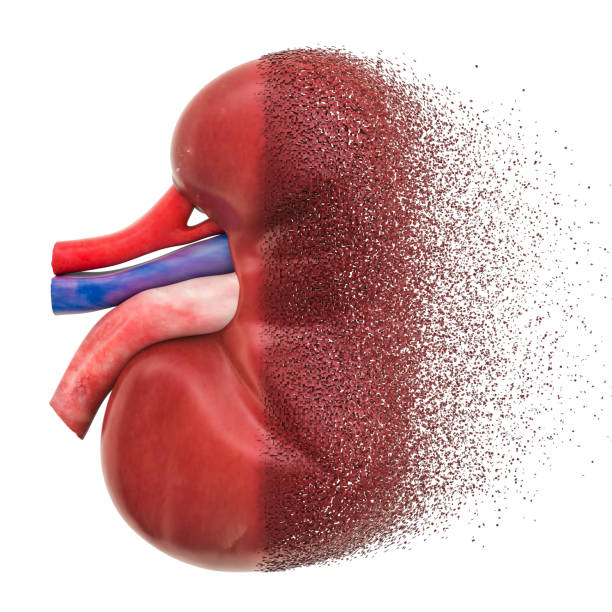
The kidneys, two small bean-shaped organs tucked neatly beneath the ribcage, rarely call attention to themselves. They work quietly, filtering waste, balancing electrolytes, and keeping blood pressure steady, day in and day out. Yet when the kidneys begin to falter, the consequences ripple throughout the entire body. Chronic kidney disease (CKD) is one of the most widespread, yet often silent, health crises of our time.
Unlike acute illnesses that announce themselves loudly, CKD often advances silently, sometimes for years, before revealing its presence. Millions of people walk through life unaware that their kidneys are slowly failing, only to discover the disease when it has already reached an advanced stage. Understanding CKD—its causes, its symptoms, its diagnosis, and its treatments—is not just about medicine. It is about survival, quality of life, and the power of awareness.
What Is Chronic Kidney Disease?
Chronic kidney disease is a long-term condition characterized by a gradual loss of kidney function over time. Healthy kidneys act like natural filters, removing waste products, toxins, and excess fluids from the blood. They also help regulate blood pressure, produce hormones that support red blood cell production, and maintain bone health by balancing calcium and phosphate.
In CKD, this filtration system breaks down. As kidney tissue is damaged, waste begins to accumulate in the blood, fluids may build up in the body, and the delicate balance of electrolytes is disturbed. Unlike acute kidney injury, which develops quickly and may be reversible, CKD progresses slowly and is often irreversible. Without treatment, it can lead to kidney failure, requiring dialysis or transplantation to sustain life.
Globally, CKD affects more than 850 million people, making it one of the most significant non-communicable diseases. Its prevalence is rising due to aging populations, increasing rates of diabetes and hypertension, and lifestyle changes that contribute to obesity and cardiovascular disease.
The Causes of Chronic Kidney Disease
CKD is not caused by a single factor but is the result of multiple health conditions and lifestyle influences. The most common causes include:
Diabetes: The Leading Culprit
Diabetes is the number one cause of CKD. High blood sugar damages the small blood vessels in the kidneys, reducing their ability to filter waste. Over time, this condition, known as diabetic nephropathy, can progress from microalbuminuria (tiny amounts of protein leaking into the urine) to full-blown kidney failure.
Hypertension: The Silent Destroyer
High blood pressure is another major cause. Constantly elevated pressure damages the delicate structures of the kidneys, forcing them to work harder and leading to scarring. In turn, CKD can worsen hypertension, creating a vicious cycle.
Glomerulonephritis
This group of diseases involves inflammation of the glomeruli, the microscopic filters in the kidneys. Causes can be autoimmune disorders, infections, or unknown factors. Over time, chronic inflammation scars kidney tissue and reduces function.
Polycystic Kidney Disease
A genetic condition, polycystic kidney disease (PKD) causes clusters of fluid-filled cysts to grow in the kidneys, enlarging them and impairing their ability to function. PKD is one of the most common inherited causes of CKD.
Prolonged Obstruction of the Urinary Tract
Conditions such as kidney stones, enlarged prostate in men, or cancers in the urinary tract can obstruct the normal flow of urine. Persistent obstruction can damage the kidneys permanently.
Recurrent Infections
Repeated kidney infections (pyelonephritis) can cause long-term scarring and damage.
Other Contributing Factors
Smoking, obesity, certain medications (such as non-steroidal anti-inflammatory drugs when used long-term), and exposure to toxins can increase the risk of CKD. Genetics, ethnicity, and family history also play a role, with some populations—such as African Americans, Hispanics, and South Asians—at higher risk.
The Progression of CKD
CKD does not appear overnight. It advances in stages, measured by glomerular filtration rate (GFR)—a test of how much blood the kidneys filter per minute.
- Stage 1: Kidney damage with normal or increased GFR (≥90).
- Stage 2: Mild reduction in GFR (60–89).
- Stage 3: Moderate reduction (30–59).
- Stage 4: Severe reduction (15–29).
- Stage 5: Kidney failure (GFR <15), also known as end-stage renal disease (ESRD).
In the early stages, many people experience no symptoms. As the disease progresses, symptoms emerge gradually, often subtle at first, and then increasingly disruptive.
Symptoms of Chronic Kidney Disease
The challenge with CKD is that symptoms often appear late. By the time many patients notice something is wrong, significant kidney damage has already occurred. The symptoms include:
- Fatigue and weakness: As toxins build up, energy levels plummet.
- Swelling (edema): Extra fluid may accumulate in the ankles, feet, hands, or around the eyes.
- Changes in urination: Frequency, volume, or appearance of urine may shift—sometimes foamy due to protein leakage, or dark due to blood.
- Nausea and vomiting: Waste buildup can upset the digestive system.
- Loss of appetite and weight loss: Food may taste metallic, and appetite can diminish.
- Itching and dry skin: Waste accumulation in the blood can cause skin irritation.
- Shortness of breath: Fluid buildup may affect the lungs, or anemia may reduce oxygen delivery.
- Muscle cramps and restless legs: Electrolyte imbalances disrupt normal muscle function.
- Confusion or difficulty concentrating: Accumulated toxins can impair brain function.
These symptoms are not exclusive to CKD, which makes early detection challenging.
Diagnosis of Chronic Kidney Disease
Diagnosing CKD requires a combination of tests, medical history, and physical examination.
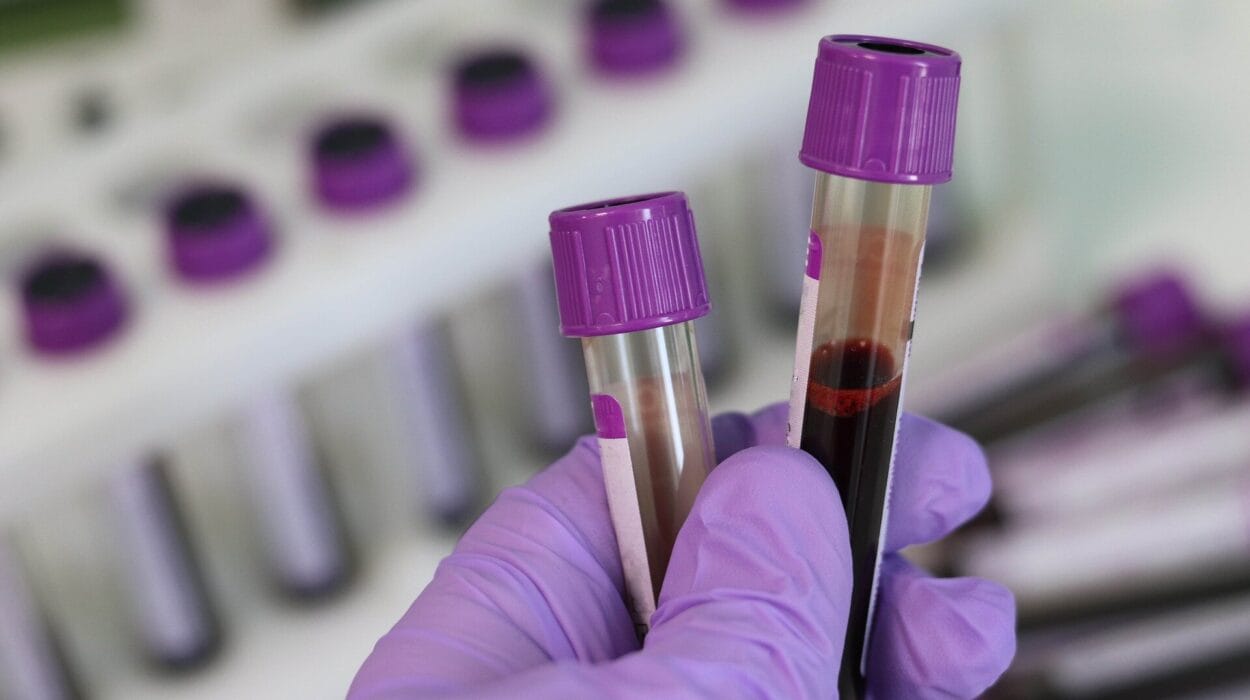
Blood Tests
- Serum creatinine and GFR estimation: Creatinine is a waste product filtered by the kidneys. High levels suggest poor kidney function. GFR, calculated from creatinine, age, sex, and body size, measures how efficiently the kidneys filter blood.
- Blood urea nitrogen (BUN): Elevated BUN indicates waste accumulation.
Urine Tests
- Urinalysis: Detects protein, blood, or abnormalities.
- Albumin-to-creatinine ratio (ACR): Measures protein leakage, often the first sign of kidney damage.
Imaging Tests
- Ultrasound or CT scans: Reveal structural abnormalities, kidney size, cysts, stones, or obstructions.
Kidney Biopsy
In uncertain cases, a small tissue sample may be taken to identify the type and extent of damage.
Diagnosis is not only about confirming CKD but also about identifying its cause and stage, which guide treatment decisions.
Treatment of Chronic Kidney Disease
CKD cannot always be cured, but its progression can often be slowed, symptoms managed, and quality of life preserved. Treatment strategies depend on the stage of the disease.
Addressing the Underlying Cause
- Diabetes management: Tight blood sugar control through diet, medication, or insulin slows damage.
- Hypertension management: Controlling blood pressure with lifestyle changes and medications—particularly ACE inhibitors or ARBs—protects the kidneys.
- Treating glomerulonephritis or infections: Specific therapies, such as immunosuppressants or antibiotics, may help.
Lifestyle Modifications
- Dietary adjustments: Limiting sodium, protein, potassium, and phosphorus intake reduces the burden on the kidneys. A renal diet is often supervised by a dietitian.
- Fluid management: Depending on kidney function and swelling, fluid intake may need regulation.
- Avoiding harmful substances: Smoking cessation, limiting alcohol, and avoiding nephrotoxic medications preserve kidney function.
- Exercise: Regular physical activity supports heart and kidney health.
Managing Complications
CKD affects many systems, and treatment often involves addressing complications:
- Anemia: Erythropoiesis-stimulating agents (ESAs) and iron supplements may restore red blood cell levels.
- Bone and mineral disorders: Medications and dietary adjustments balance calcium and phosphate.
- Cardiovascular risk: Cholesterol-lowering drugs and blood pressure control reduce heart disease risks.
Advanced Stages: Dialysis and Transplantation
When CKD progresses to end-stage renal disease, kidneys can no longer sustain life without external support.
- Dialysis:
- Hemodialysis: Blood is filtered through a machine outside the body.
- Peritoneal dialysis: The abdominal lining acts as a natural filter with the help of a dialysis solution.
- Kidney transplantation: Replacing the failing kidneys with a healthy donor kidney offers the best long-term outcome for many patients. However, organ availability, rejection risks, and lifelong immunosuppressive therapy complicate this option.
Living with CKD: The Human Dimension
A diagnosis of CKD changes life profoundly. Beyond the medical treatments, patients often face emotional challenges—fear of progression, anxiety about dialysis, financial strain, and the psychological weight of living with a chronic condition.
Support systems—family, friends, healthcare teams, and patient communities—play a vital role in helping individuals adapt. Counseling, stress management techniques, and patient education empower individuals to take charge of their health, make informed choices, and maintain hope.
Prevention and Early Detection
Since CKD often develops silently, prevention and early detection are key. Regular check-ups, especially for people with risk factors such as diabetes, hypertension, or family history, can detect kidney damage early. Simple urine and blood tests can uncover CKD long before symptoms appear, allowing timely intervention.
Prevention strategies—healthy diet, regular exercise, blood pressure and sugar control, avoiding smoking—are the same habits that protect overall health. Public health campaigns and community awareness are essential tools in reducing CKD’s global burden.
The Future of CKD Management
Medical research is advancing rapidly. New drugs, such as SGLT2 inhibitors originally developed for diabetes, have shown remarkable promise in slowing CKD progression. Advances in regenerative medicine may one day enable scientists to grow or repair kidney tissue. Artificial intelligence is being used to detect early signs of kidney disease from routine health records.
The vision for the future is not only better treatments but also more equitable access to care, ensuring that everyone—regardless of geography or income—can benefit from medical advances.
A Message of Hope
Chronic kidney disease is daunting, but it is not a hopeless condition. With early detection, proper management, and lifestyle changes, many people live full, active lives with CKD. Even in advanced stages, treatments like dialysis and transplantation provide a lifeline, and ongoing research promises even better solutions in the future.
To understand CKD is to understand the resilience of the human body and spirit. The kidneys may be silent workers, but their health echoes loudly in every part of our lives. By listening carefully—through awareness, prevention, and care—we can honor their role and protect the life-sustaining harmony they provide.