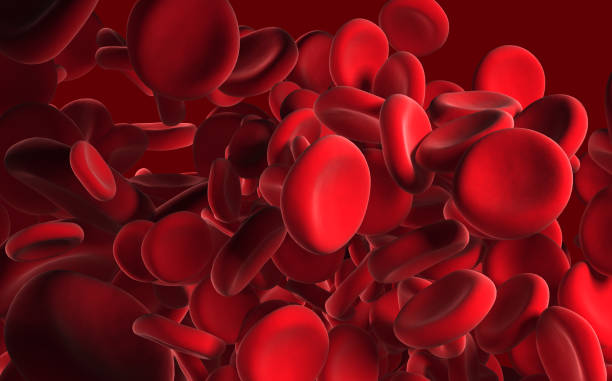
For decades, Alzheimer’s disease has been one of the most haunting mysteries in medicine. Families watch their loved ones slowly lose memory, language, and independence, while scientists struggle to understand why the disease begins and how to stop it. Traditionally, research has focused on the brain itself—on the sticky amyloid plaques and twisted tau tangles that are seen in autopsies of patients. But a new study led by the Emory Goizueta Brain Health Institute and partner institutions has opened an unexpected door: the blood.
In findings published in Nature Aging, researchers studied more than 2,100 people across four major research cohorts and discovered that changes in blood proteins could reveal hidden clues about Alzheimer’s development and progression. The work does more than expand our knowledge—it shifts the landscape of how we think about the disease, and it could change how we diagnose and treat it in the years to come.
The Search Beyond the Brain
For a long time, the scientific community saw Alzheimer’s primarily as a disease of the brain. The presence of amyloid plaques—clumps of sticky proteins—and tau tangles has been the central narrative of Alzheimer’s research. But this view has always been incomplete. Some people with heavy plaque buildup never develop dementia, while others show severe memory decline without dramatic plaque accumulation.
This mismatch has left scientists asking: What else is happening?
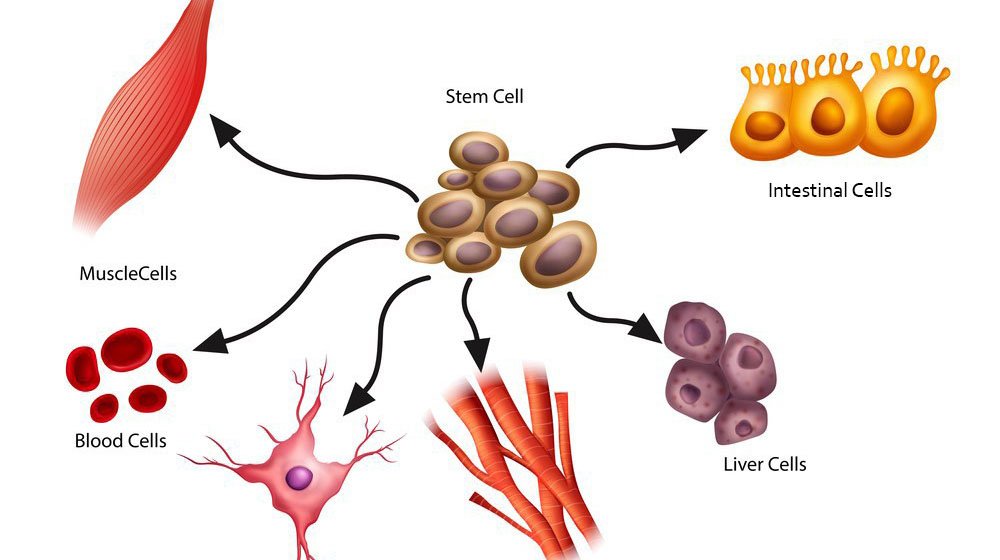
The new study begins to answer that question. By analyzing blood samples with advanced tools capable of measuring thousands of proteins, the team uncovered patterns that suggest Alzheimer’s is not just a brain disease—it is a whole-body disease.
What the Blood Reveals
The researchers found that several groups of proteins in the blood were tied to memory and thinking problems. These proteins weren’t only linked to plaques or tangles but reflected broader processes:
- Immune system activity – suggesting the body’s defense system may fuel inflammation that harms the brain.
- Protein disposal mechanisms – pointing to difficulties in clearing away damaged or misfolded proteins.
- Energy metabolism – indicating that how the body generates and uses energy might affect brain health.
- The extracellular matrix – the structural support system of the body, which may influence how brain cells communicate.
What is striking is that many of these protein changes could not be explained by known Alzheimer’s brain changes. As senior author Dr. Erik Johnson of Emory’s Goizueta Alzheimer’s Disease Research Center put it, “This means that what’s happening in the rest of the body could play a role in Alzheimer’s risk and how fast the disease progresses.”
A Shift in Perspective
This discovery challenges the idea that Alzheimer’s is purely a neurological condition. Instead, it highlights the possibility that the immune system, metabolism, and even processes in other organs may influence the disease. If Alzheimer’s is shaped by signals and systems throughout the body, then new treatments could be developed to target these pathways—opening therapeutic doors that were once unimaginable.
Instead of struggling to get drugs into the brain, where the protective blood-brain barrier makes access difficult, doctors may one day be able to intervene by targeting processes in the blood and peripheral organs.
Toward a Blood Test for Alzheimer’s
Another exciting implication of the study is diagnostic. Today, diagnosing Alzheimer’s can involve invasive spinal taps, expensive brain scans, or years of clinical observation. But this research strengthens the case for a simple blood test as a powerful tool for detection.
“All of this work is foundational to the development of blood tests,” explains Dr. Allan Levey, executive director of the Goizueta Institute at Emory. Such tests could track multiple pathologies alongside amyloid plaques, helping doctors catch the disease earlier and monitor its progression more easily.
A routine blood draw could someday replace more invasive procedures, allowing doctors not only to diagnose Alzheimer’s sooner but also to tailor treatments to each individual based on their unique protein patterns.
The Power of Collaboration
This breakthrough was made possible by a wide network of research participants and institutions. The team drew from diverse sources, including:
- Emory University Alzheimer’s research studies
- The Bio-Hermes study
- The Religious Orders Study
- The Rush Memory and Aging Project (ROSMAP)
Together, these cohorts provided the depth and variety of data necessary to uncover meaningful patterns across thousands of proteins. Without these collaborations—and the generosity of participants who shared their time, health information, and samples—this leap forward would not have been possible.
A Future of Hope
Alzheimer’s is one of the most feared diseases of our time, not only because of its devastating toll on memory and identity but also because of how little we have been able to do to stop it. For decades, the field has chased the mystery of amyloid plaques, often with disappointing results. But this new research offers something profoundly hopeful: a shift in the narrative.
By revealing that Alzheimer’s is connected to systems beyond the brain, scientists can now begin to explore new frontiers of treatment and prevention. The study reminds us that the body and brain are inseparably linked, and that understanding one requires paying attention to the other.
Conclusion: A New Chapter in the Fight Against Alzheimer’s
The blood, it turns out, carries more than oxygen and nutrients. It carries clues—signs of how our bodies and brains are intertwined in health and disease. The discovery by Emory Goizueta Brain Health Institute and its partners marks a turning point in Alzheimer’s research.
It shows us that the disease is more complex than plaques and tangles, more dynamic than what we see in autopsies. It shows us that hope for earlier detection, easier testing, and broader treatment options may lie not only in the brain but also in the bloodstream.
In the end, this research is not just about proteins or pathways. It is about people—the millions living with Alzheimer’s today, the families who care for them, and the generations who may one day be spared the heartbreak of memory loss. Each new discovery brings us closer to that future, and this study is a powerful step along the way.
More information: Shiva Afshar et al, Plasma proteomic associations with Alzheimer’s disease endophenotypes, Nature Aging (2025). DOI: 10.1038/s43587-025-00965-4