Cancer is often described as a disease of mutations, a chaotic rewriting of the genetic script. But a new study unveiled at the 2025 American Society of Hematology meeting invites us to look at the disease through a different lens. Imagine a bustling city where roads vanish overnight. Neighborhoods become isolated. Essential services can’t reach the people who depend on them. Life slowly breaks down, not because the buildings are wrong, but because the connections between them have collapsed.
This, researchers say, is what happens inside our cells when the 3D structure of DNA begins to unravel. And even small disruptions to this architecture may be enough to tip a healthy cell toward malignancy.
A Blueprint Lost in the Middle of Construction
The work comes from Martin Rivas, Ph.D., a cancer researcher at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine. His team presented a study with an idea that feels both technical and deeply intuitive at once. The title is a mouthful, but its message is clear. “SMC3 and CTCF Haploinsufficiency Drive Lymphoid Malignancy via 3D Genome Dysregulation and Disruption of Tumor Suppressor Enhancer-Promoter Loops.”
The study proposes something called architectural tumor suppression. It is a concept built around the idea that some proteins don’t just manage DNA structure—they actively prevent cancer by preserving the loops that connect gene switches, called enhancers, to the genes they control, known as promoters.
Lose even half of these proteins, like SMC3 or CTCF, and the consequences are dramatic. The loops that keep tumor suppressor genes switched on start to vanish. “We’ve long known that mutations drive cancer,” said Rivas. “But this work shows that architecture—the way DNA folds—can be just as important. It’s like losing the blueprint for a building while construction is under way.”
When the blueprint disappears, so does the order it once enforced.
How Small Cracks Become Deep Fault Lines
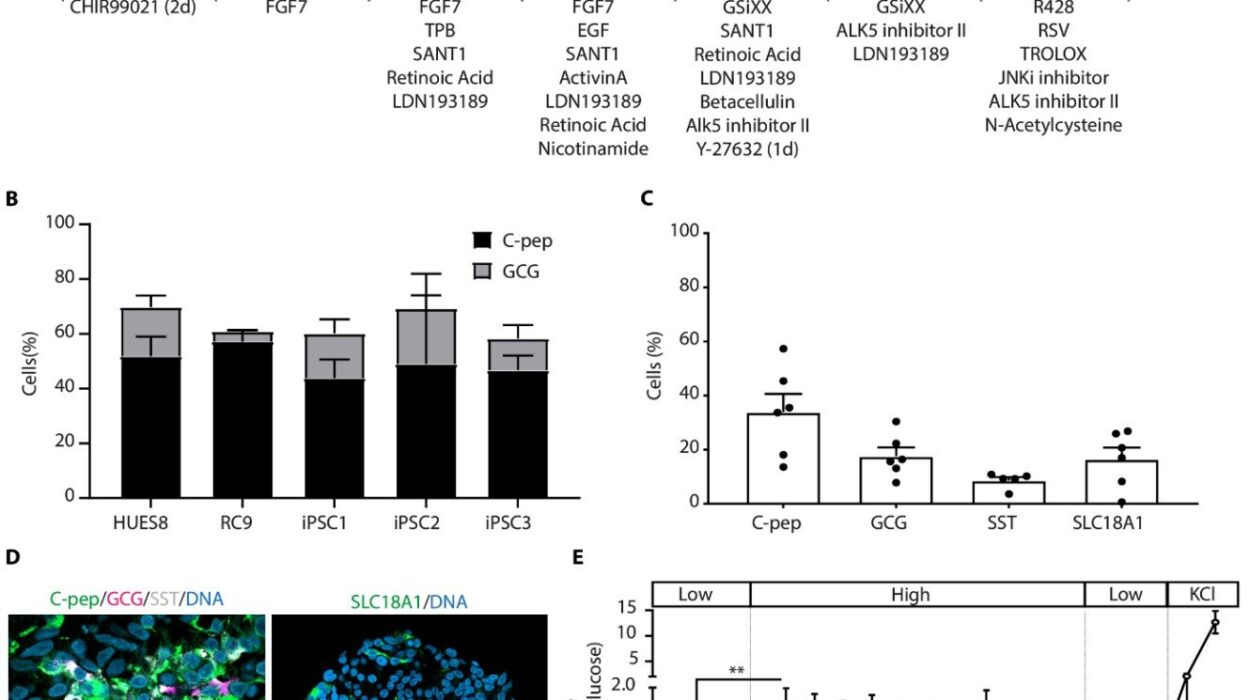
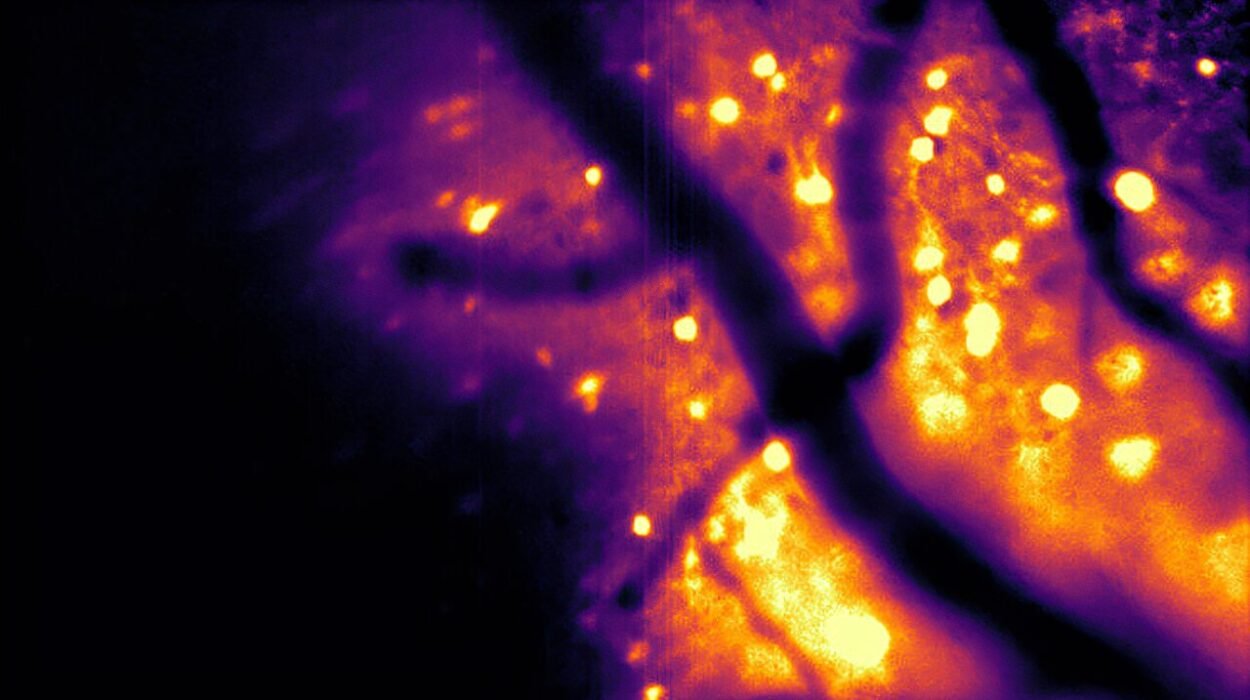
The team used AI-driven analytics to dive into enormous datasets. These included Hi-C maps that visualize DNA folding, single-cell RNA sequencing that captures individual cellular voices, and epigenetic profiles that reveal chemical marks shaping gene activity. When all these layers were woven together, a striking pattern emerged.
Partial loss of SMC3 or CTCF does not completely destroy genome structure. The cell doesn’t collapse into genetic chaos. Instead, something subtler—and perhaps more dangerous—happens. Short-range enhancer-promoter loops begin to erode. These are the tiny but essential wiring connections that keep tumor suppressor genes like Tet2, Kmt2d, and Dusp4 running.
Without these loops, B-cells enter what the researchers call a decision bottleneck. They struggle to mature into plasma cells, the very cells responsible for producing antibodies. This stalled development creates fertile ground for disease to take hold.
AI tools provided the clarity needed to see this hidden ripple effect. “This is where computational biology shines,” Rivas added. “AI allowed us to see patterns invisible to the human eye—how losing just one copy of a gene reshapes the entire 3D landscape.”
The emerging picture is one where cancer does not begin with catastrophic failure, but with quiet, structural weakening.
The Human Consequences Hidden in the Loops
The research isn’t limited to lab models. It has echoes in real patient outcomes. Individuals with diffuse large B-cell lymphoma who show lower expression of SMC3 tend to fare worse. The architectural damage appears to carry clinical weight.
This finding hints at a future where measurements of genome structure could become a biomarker—a signal that warns physicians how aggressive a patient’s disease might be. If doctors could understand how healthy or damaged the 3D genome is, they might adjust treatments with greater precision.
Even more compelling is the therapeutic potential. Instead of targeting genetic mutations directly, future treatments might aim to restore lost DNA loops or mimic their stabilizing effects. In this view, cancer becomes not only a problem of code but a problem of scaffolding. Fix the scaffolding, and the cell may regain its stability.
The implications ripple outward. Treatments might one day reinforce the architecture of the genome the same way engineers stabilize a trembling bridge or rebuild the infrastructure of a failing city.
Why This Discovery Matters
At the heart of this study is a shift in how we think about cancer. For decades, the field has focused on broken genes. Now, researchers are realizing that the folding, looping, and physical structure of DNA are just as critical to the cell’s survival.
“We’re entering an era where cancer treatment could mean repairing architecture, not just fixing broken genes,” said Rivas. “That’s a paradigm shift.”
This paradigm shift doesn’t erase what we know about cancer genetics. Instead, it adds a new layer of understanding, one that explains how cells with few mutations can still fall apart—or how cells with many mutations sometimes resist transformation. It depends not only on what genes are present, but on whether those genes can communicate through their loops, signals, and structural highways.
The city analogy circles back here. Inside our cells, tumor suppressor genes are like essential service centers. They need roads—DNA loops—to reach the rest of the genome and perform their work. When those roads disappear, even without obvious mutations, the system begins to falter. Neighborhoods become isolated. Signals fail. Cancer finds openings.
In this new view of cancer biology, restoring those lost roads becomes a tantalizing possibility. It means giving the cell back its internal map. It means reconnecting the lifelines that keep it healthy.
And most importantly, it opens the door to therapies that work not by rewriting genetic code, but by rebuilding the structure that holds life together.