For decades, Alzheimer’s disease has remained one of medicine’s most stubborn mysteries—a devastating condition with no known cure, and only modestly effective treatments. Most efforts have focused on hallmark features like amyloid plaques and tau tangles, hoping that removing these toxic buildups might halt or even reverse cognitive decline. But results have been disappointing. Now, scientists at the Mayo Clinic have unveiled a compelling new theory: perhaps the disease begins even earlier, not in the misfolding of proteins, but in a subtle breakdown of the brain’s energy supply.
Published in the journal Alzheimer’s & Dementia, the new study highlights a surprising and powerful driver of disease progression—mitochondrial complex I, a key protein complex that fuels the brain’s energy needs. When its function falters, the consequences ripple outward, altering gene expression, triggering inflammation, and mirroring the very changes observed in Alzheimer’s patients. The findings offer both a radical shift in how we understand Alzheimer’s disease and a promising new target for future treatments.
Mitochondria: More Than Just the Cell’s Power Plant
Most of us learned in high school biology that mitochondria are the “powerhouses” of the cell—organelles that generate energy in the form of adenosine triphosphate (ATP), which powers nearly all cellular processes. But in neurons, which are some of the most energy-hungry cells in the human body, mitochondria play a much more intricate and vital role.
“Our brains represent only 2% of our body weight, but they consume about 20% of our total energy,” explains Dr. Eugenia Trushina, senior author of the study and a leading neurodegenerative disease researcher at Mayo Clinic. “Any disruption in the way neurons generate and manage energy can have serious consequences for brain health.”
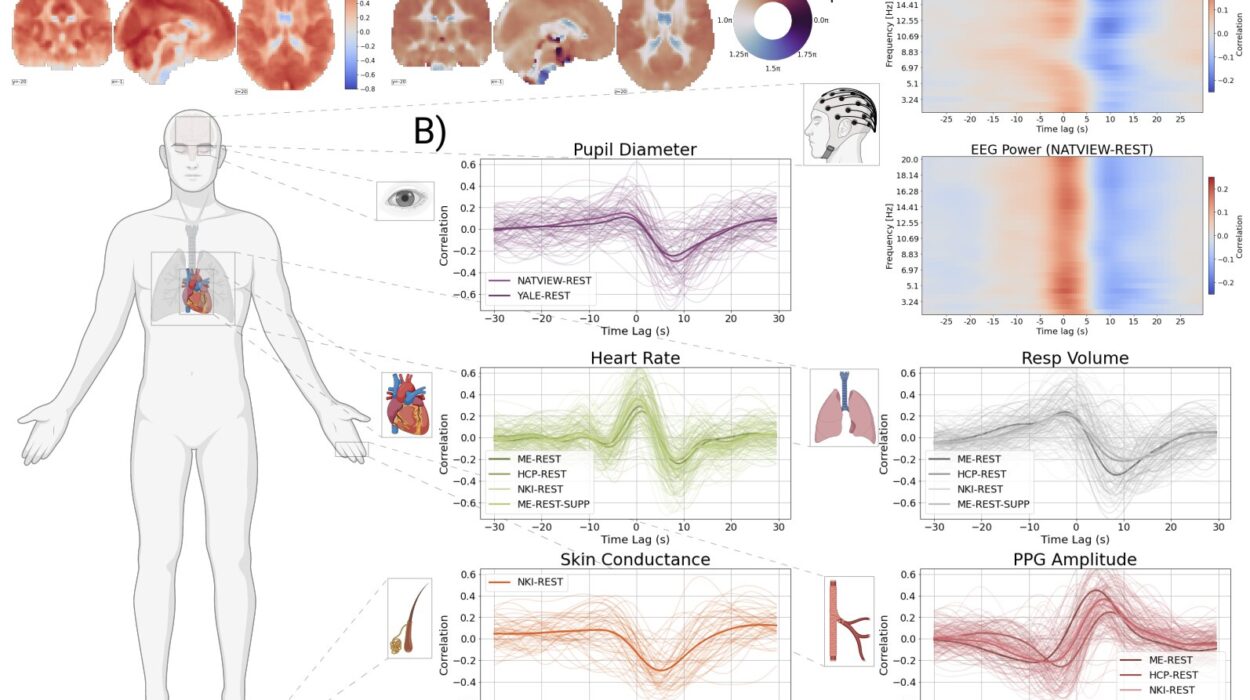
The study zeroes in on complex I—the first and largest component of the mitochondrial electron transport chain. It acts as a gatekeeper in the process of oxidative phosphorylation, which ultimately converts food into usable cellular energy. Malfunction here doesn’t just cause energy shortages; it can lead to the buildup of damaging byproducts, like reactive oxygen species, and trigger gene expression patterns eerily similar to those seen in Alzheimer’s brains.
A New Role for Complex I in Alzheimer’s Disease
Dr. Trushina’s team employed advanced molecular techniques and computational modeling to analyze what happens when complex I doesn’t function properly. Using laboratory models that mimic aspects of Alzheimer’s disease, they found that even mild disruptions to complex I activity could lead to widespread cellular dysfunction.
But there was a twist.
When researchers used specially designed small molecules to gently tweak complex I—rather than completely shutting it down—they noticed something extraordinary. The brain cells didn’t collapse; instead, they adapted. They initiated stress responses that reduced inflammation, corrected energy imbalances, and activated protective genes. In other words, a slight push in the right direction seemed to awaken the cell’s own self-defense systems.
“This wasn’t about fixing the entire disease process at once,” says Dr. Trushina. “It was about nudging cells to do what they naturally know how to do—protect themselves, restore balance, and maintain function.”
Male and Female Brains May Respond Differently
One of the most intriguing and potentially important discoveries was how sex influenced the response to treatment. Male and female models reacted differently to complex I modulation, both in terms of gene activity and cellular outcomes.
“This sex-dependent effect is not just interesting—it could be crucial,” says Dr. Trushina. “We’ve known for a while that Alzheimer’s disease affects men and women differently, both in terms of risk and symptom progression. But treatments have not yet accounted for these differences.”
The implication is that future Alzheimer’s therapies may need to be sex-specific, designed to work with the biological differences in male and female brains. It’s a reminder that personalized medicine isn’t just about genetics or environment—it’s also about biology we’ve historically overlooked.
Looking Beyond Plaques and Tangles
Alzheimer’s disease has long been associated with two types of pathological structures: amyloid plaques, formed by sticky protein deposits outside neurons, and tau tangles, twisted fibers inside neurons. These have dominated research and drug development efforts for decades.
But critics argue that these may be symptoms, not causes. After all, many people accumulate amyloid in their brains without ever developing cognitive symptoms. And recent anti-amyloid drugs, while groundbreaking, have shown only modest benefit—and come with serious side effects.
“This is why the mitochondrial perspective is so exciting,” Dr. Trushina explains. “We’re not waiting for plaques to form. We’re going upstream to a place where the disease might begin—before symptoms, before brain shrinkage, before memory loss.”
In this view, mitochondrial dysfunction is a spark, not just a consequence. And by modulating energy production early, researchers hope to extinguish that spark before it ignites a full-blown neurodegenerative fire.
Harnessing the Cell’s Survival Instincts
One of the most powerful aspects of the study is its demonstration that cells can fight back—if given the right signal. The small molecules used by the researchers don’t act like traditional drugs that aim to stop or reverse a specific defect. Instead, they modulate function gently, restoring balance rather than enforcing control.
This is a strategy rooted in systems biology—the idea that complex networks like energy metabolism don’t respond well to all-or-nothing interventions. Instead, they benefit from subtle shifts that activate adaptive responses already built into the system.
In the case of neurons, these include reducing oxidative stress, improving ATP production, stabilizing mitochondrial structure, and dampening inflammatory signals. Each of these is known to play a role in Alzheimer’s progression. Together, they may offer a powerful, multifaceted defense.
A Path Toward New, Preventive Therapies
Perhaps the most exciting part of this research is its potential to lead to early, preventive treatments. Unlike many existing drugs that are given after diagnosis, these complex I modulators might one day be used to protect at-risk individuals—those with a family history of Alzheimer’s, or early signs of cognitive decline.
“This is the vision behind Mayo Clinic’s Precure initiative,” Dr. Trushina says. “We want to develop tools that don’t just treat disease—we want to predict and intercept it before it becomes irreversible.”
The team’s next steps involve further testing the safety and efficacy of these molecules in animal models, with hopes of eventually moving to clinical trials. They will also explore biomarkers that could signal when mitochondrial dysfunction begins—clues that could guide personalized treatment plans years before full-blown symptoms appear.
Why This Matters to You
Alzheimer’s disease affects nearly 7 million Americans, with numbers expected to double in the coming decades. It not only robs individuals of memory and identity but devastates families, caregivers, and healthcare systems. It is not a disease of the distant future—it’s a growing crisis.
What makes this new study so important is its hopeful message: there may be another way forward. By shifting the focus from broken proteins to broken energy systems, we may find earlier, more effective, and more humane ways to fight this disease. We may even be able to stop it before it starts.
More than a scientific breakthrough, this research represents a philosophical one. It suggests that rather than fighting pathology head-on, we might do better to support the body’s own resilience, to amplify the protective instincts already wired into our cells.
The Dawn of a New Era in Alzheimer’s Research
It’s still early. Much work remains before these insights can be translated into a drug that helps real people. But the direction is clear, and the promise is real.
For too long, Alzheimer’s has been a mystery we watched unfold too late. This study from Mayo Clinic offers a new beginning—a lens that focuses not on what’s broken, but on what might still be saved. And in that lens, there is light.
More information: Huanyao Gao et al, Mitochondrial complex I deficiency induces Alzheimer’s disease–like signatures that are reversible by targeted therapy, Alzheimer’s & Dementia (2025). DOI: 10.1002/alz.70519