For decades, scientists have tried to answer two elusive questions about Alzheimer’s disease: what sets it in motion, and why do some people with Alzheimer’s-like changes in their brains never develop dementia? A groundbreaking new study published in Nature offers a powerful, paradigm-shifting answer—one that may eventually help prevent, diagnose, and even reverse the disease.
The culprit, according to a team of researchers at Harvard Medical School, may be a hidden deficiency of lithium, a naturally occurring element already known for its role in mood regulation. This discovery, built on a decade of painstaking experiments, offers more than just another clue. It suggests that lithium is essential for brain health, and its loss could be the earliest and most overlooked spark that lights the fire of neurodegeneration.
The findings not only offer new insight into how Alzheimer’s begins, but also why it progresses—and, perhaps most remarkably, why in some people it doesn’t.
A Mysterious Defender in the Brain
When most people hear “lithium,” they think of batteries or bipolar disorder. But the human brain, it turns out, naturally contains trace amounts of lithium, and until now, no one really understood why.
In a study led by Professor Bruce Yankner at Harvard’s Blavatnik Institute, researchers show for the first time that this trace lithium plays a protective role in every major brain cell type—including neurons, microglia, and oligodendrocytes—and helps preserve cognitive function. The absence of lithium, they found, is not a silent change but a starting gun for the cascade of pathology we associate with Alzheimer’s disease.
Through a series of advanced techniques—ranging from mass spectrometry analysis of human brain tissue to mouse models genetically engineered for Alzheimer’s—the team discovered that lithium depletion happens early, before the classic symptoms of Alzheimer’s appear. In fact, it may be one of the first detectable biochemical changes as the disease begins its stealthy march through the brain.
What Happens When Lithium Disappears
Lithium in the brain appears to vanish just as the protein amyloid beta begins to accumulate. The researchers found that amyloid binds lithium, sequestering it and making it unavailable to brain cells. This critical change interferes with the normal functioning of neurons and other support cells, weakening the brain’s natural defenses.
In people who have early signs of Alzheimer’s but remain cognitively healthy, lithium levels are high. In contrast, those in the mild cognitive impairment (MCI) stage—often a precursor to Alzheimer’s—show a sharp drop. By the time full-blown dementia has developed, lithium is almost completely gone from the brain tissue.
This lithium loss, the researchers argue, is not just a result of the disease—it may be a driver.
The Mouse Model That Unlocked the Mystery
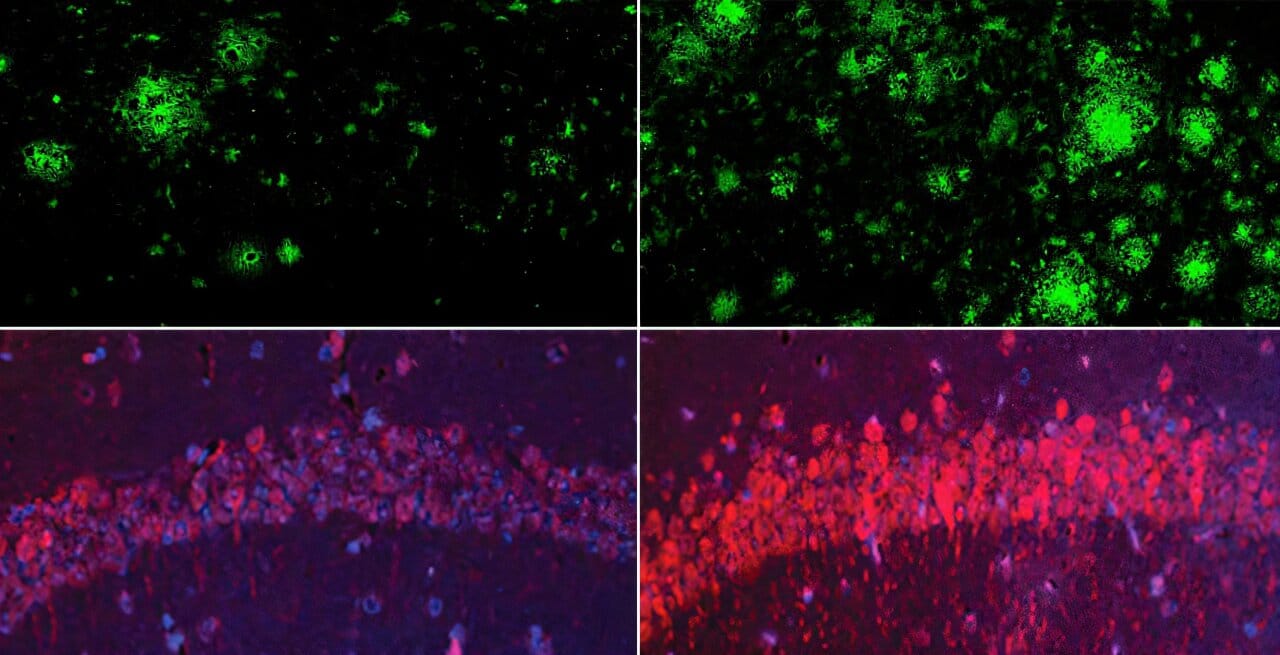
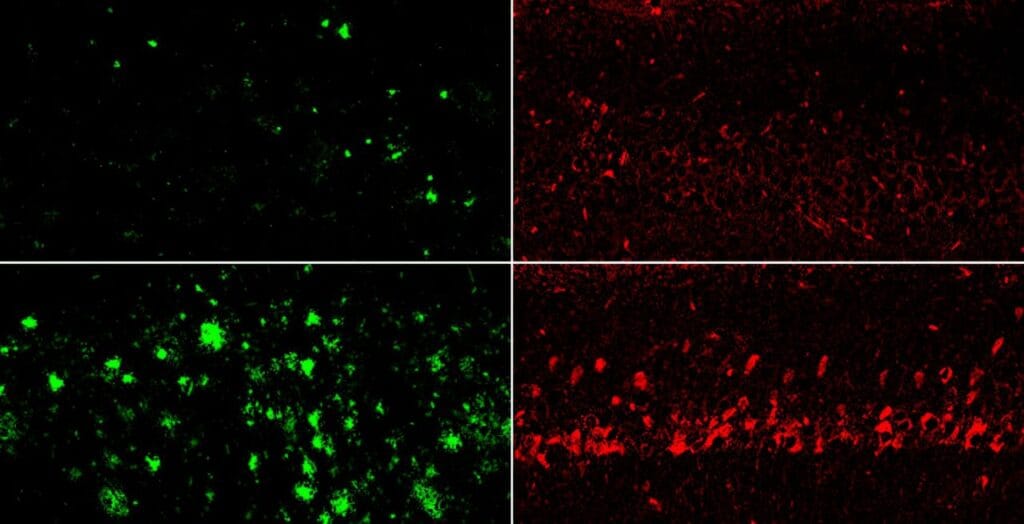
To test whether lithium deficiency could cause Alzheimer’s-like changes, the researchers placed healthy mice on a lithium-restricted diet. Over time, these animals developed the telltale signs of Alzheimer’s disease: memory loss, inflammation, loss of synapses, and even accumulation of amyloid plaques and tau-like tangles.
When lithium levels dropped, so did the brain’s ability to protect itself. Cells that normally clean up amyloid beta—microglia, the brain’s immune cells—stopped working effectively. Neurons lost their connections. Myelin, the protective coating on brain circuits, began to break down. Even gene activity shifted, mimicking the harmful patterns seen in human Alzheimer’s cases.
In essence, the study showed that lithium depletion wasn’t just associated with Alzheimer’s—it actually mimicked and accelerated it.
A New Kind of Lithium, a New Kind of Hope
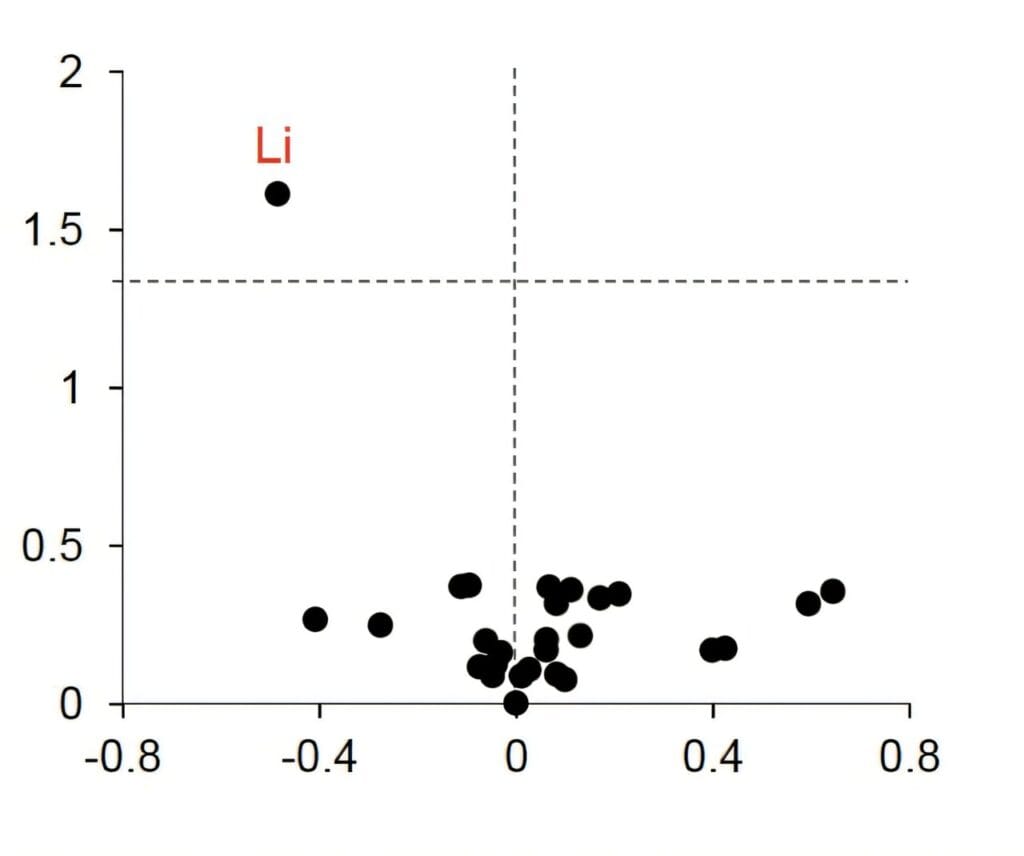
Recognizing the potential for therapeutic intervention, the researchers screened for lithium compounds that could escape the grip of amyloid beta. They identified one—lithium orotate—that could bypass amyloid binding and reach the brain in effective, nontoxic doses.
When they gave lithium orotate to mice showing signs of Alzheimer’s, something astonishing happened: the disease began to reverse. Memory improved. Brain structure and function recovered. Even in older mice with advanced pathology, the compound restored cognitive ability.
Even more promising, lithium orotate achieved this at one-thousandth the dose used in traditional lithium medications like lithium carbonate—levels too small to cause side effects.
These findings open the door to a new kind of Alzheimer’s therapy—one that targets the disease at its earliest stages, possibly even before symptoms arise.
Why Alzheimer’s Isn’t the Same for Everyone
One of the most confounding aspects of Alzheimer’s has always been its variability. Some people with significant amyloid plaque buildup show no symptoms. Others decline rapidly. Genes like APOE4 increase risk but don’t guarantee disease. Lifestyle factors such as diet and exercise play roles, but the puzzle remains incomplete.
This new lithium theory offers a unifying explanation: those who maintain healthy brain lithium levels may be protected, even if other risk factors are present. Conversely, individuals with depleted lithium stores may be vulnerable, regardless of genetics.
This idea is supported by previous population studies that found lower Alzheimer’s rates in regions with naturally higher lithium levels in drinking water. The new research provides a biological basis for these correlations and a potential framework for early detection and intervention.
Toward a Simple Blood Test—and a New Standard of Care
One of the most practical implications of this discovery is the potential to develop a simple blood test to measure lithium levels, enabling doctors to assess Alzheimer’s risk long before memory loss begins.
If further research confirms the findings, routine lithium screening could become part of annual checkups for aging adults—an early-warning system similar to cholesterol tests for heart disease. Those found to be deficient could be treated with very low-dose lithium supplements, possibly preventing or delaying the onset of dementia.
The researchers stress, however, that more work is needed. While the animal results are compelling, human biology is more complex. Only controlled clinical trials can determine whether lithium orotate is safe and effective in people with or at risk for Alzheimer’s.
Still, the signs are hopeful. The compound already has a known safety profile, and the ultra-low doses required for brain benefit may reduce the risk of toxicity seen in older lithium drugs.
From Battlefield to Blueprint
One of the biggest challenges in Alzheimer’s research has been studying the disease early enough to understand its root causes. Most brain studies rely on tissue from patients in the final stages of dementia—akin to surveying a battlefield after the war is lost.
But thanks to the collaboration with the Rush Memory and Aging Project in Chicago, the Harvard team had access to an unprecedented resource: postmortem brain tissue from thousands of individuals across the entire spectrum of cognitive health. This allowed the scientists to see Alzheimer’s not just as an end-stage disease, but as a continuum that begins long before symptoms appear.
Their discovery redefines how we think about the disease and offers a new blueprint—one that starts with maintaining optimal lithium levels and leads to a new kind of intervention that targets not a single molecule, but the broader biology of the aging brain.
A New Era in Alzheimer’s Science
For decades, Alzheimer’s research has focused on removing amyloid plaques and tau tangles from the brain. But treatments based on those approaches have met with limited success. This new research suggests that the more fundamental problem might be a loss of lithium—an elemental protector of brain function.
By restoring lithium, scientists may not just delay the damage, but prevent it entirely. It’s a bold new direction—one that doesn’t seek to treat the smoke, but to extinguish the spark.
Of course, caution is warranted. The human brain is one of the most complex systems in the known universe, and translating mouse results into human therapies is never simple. But for millions of people watching loved ones fade into memory loss, and for millions more who fear the disease may one day claim them too, this discovery offers something precious:
Hope.
Not just for a slightly slower decline, but for a genuine, biological shield—rooted in nature, accessible through science, and ready, perhaps, to be deployed in the fight against one of humanity’s most devastating diseases.
More information: Lithium deficiency and the onset of Alzheimer’s disease, Nature (2025). DOI: 10.1038/s41586-025-09335-x
Ashley I. Bush, Does lithium deficiency contribute to Alzheimer’s disease?, Nature (2025). DOI: 10.1038/d41586-025-02255-w , doi.org/10.1038/d41586-025-02255-w