Imagine a world where a minor cut could kill you. Where childbirth was a gamble with death. Where pneumonia, strep throat, or a urinary tract infection could become life-threatening. It’s not the plot of a dystopian novel. It was reality—just over a century ago. Then came antibiotics. They were the miracle drugs of the 20th century, the invisible warriors that reshaped medicine, prolonged human life, and transformed fatal infections into treatable inconveniences. But this miracle comes with a catch.
Today, we’re facing a mounting global health crisis: antibiotic resistance. Bacteria are adapting, evolving, and outsmarting the very drugs designed to kill them. The era of antibiotics, some scientists warn, may be slipping through our fingers. But before we get into why resistance is one of the gravest threats to global health, let’s first understand how antibiotics work—and why they were such a revolutionary force.
The Birth of Antibiotics: A Serendipitous Discovery
The story of antibiotics begins, famously, with a petri dish and a stroke of luck. In 1928, Alexander Fleming, a Scottish bacteriologist, returned from vacation to his messy lab in London. Among the cultures of Staphylococcus bacteria he’d left behind, he noticed something strange: a mold had contaminated one dish, and around it, the bacteria had been killed. The mold was Penicillium notatum. Fleming had stumbled upon the world’s first true antibiotic—penicillin.
Fleming’s discovery didn’t immediately change the world. The mold was difficult to grow and its antibacterial agent hard to extract. It wasn’t until the 1940s, thanks to scientists like Howard Florey and Ernst Boris Chain, that penicillin was mass-produced. During World War II, it saved countless lives from battlefield infections. It became known as the “wonder drug.”
Penicillin’s success ushered in a golden age of antibiotic discovery. Streptomycin, chloramphenicol, tetracycline—all emerged in the decades that followed. Pharmaceutical companies and research labs scoured soil and mold for new bacteria-fighting compounds. By the 1970s, antibiotics were everywhere, curing diseases, enabling surgeries, and saving lives on a scale previously unthinkable.
What Exactly Are Antibiotics?
Antibiotics are substances—natural or synthetic—that inhibit the growth of, or outright kill, bacteria. They’re not effective against viruses, fungi, or parasites; antibiotics target bacterial infections specifically. This is why antibiotics don’t work for colds, the flu, or COVID-19.
There are two main types of antibiotics: bactericidal and bacteriostatic. Bactericidal antibiotics kill bacteria directly. Think of them as microbial assassins. Bacteriostatic antibiotics, on the other hand, don’t kill bacteria but stop them from multiplying, giving the body’s immune system time to eliminate the infection.
These drugs operate in several ways, depending on their chemical structure and bacterial target. Some break down bacterial cell walls. Others inhibit protein synthesis or DNA replication. Regardless of the method, the result is the same: the bacteria can’t function, reproduce, or survive.
How Antibiotics Work: Microscopic Warfare
To appreciate the power of antibiotics, it’s worth looking closer at how they wage war on bacteria.
One of the most common antibiotic targets is the bacterial cell wall. Human cells don’t have cell walls, but many bacteria do, and this structural difference is a key vulnerability. Drugs like penicillin and cephalosporins interfere with peptidoglycan, a molecule crucial for building bacterial walls. Without it, the bacteria burst under their own pressure—like a balloon with a pinhole.
Other antibiotics focus on the machinery bacteria use to produce proteins. Tetracyclines, macrolides (like erythromycin), and aminoglycosides disrupt the ribosomes—the molecular factories that synthesize proteins. Since bacterial ribosomes differ from human ones, antibiotics can selectively disrupt bacterial protein production without harming the host.
Still others target bacterial DNA. Fluoroquinolones, such as ciprofloxacin, interfere with enzymes bacteria need to unwind and replicate their DNA. No DNA replication, no reproduction.
Antibiotics exploit the biological differences between human and bacterial cells, giving them a remarkable ability to kill or suppress pathogens without (usually) harming the patient. But this precision is not foolproof.
The Rise of Antibiotic Resistance: An Evolutionary Tale
To understand antibiotic resistance, we need to understand evolution. Bacteria, like all living things, mutate. Each time they divide, their DNA is copied—and occasionally, errors sneak in. These mutations can be neutral, harmful, or beneficial. When a bacterium mutates in a way that helps it survive antibiotics, that mutation is a jackpot.
Imagine a patient with a bacterial infection. They take antibiotics. Most bacteria die. But a few have mutations that help them resist the drug—they might pump it out of their cells, change the drug’s target, or produce enzymes that destroy the antibiotic. These survivors multiply, creating a new population that the drug can no longer touch.
This is natural selection at warp speed. And it’s happening everywhere—inside hospitals, on farms, in soil, in water systems. Bacteria share genes, too. They can pass resistance traits to other bacteria, even across species, through a process called horizontal gene transfer. One superbug can teach another how to survive.
The more antibiotics we use, the more we pressure bacteria to evolve. And we’ve used a lot—often unnecessarily.
Overuse and Misuse: The Recipe for Resistance
The explosion of antibiotic resistance isn’t just bad luck. It’s largely our own doing. Antibiotics are powerful tools, but they’ve been overprescribed, overused, and mishandled for decades.
Doctors sometimes prescribe antibiotics “just in case,” even when they’re not needed—especially for viral infections. Patients often demand antibiotics, expecting a quick fix, or fail to finish their prescribed course, allowing surviving bacteria to rebound stronger than ever. In some countries, antibiotics are available over the counter, making self-medication common and regulation difficult.
But one of the biggest culprits is agriculture. Globally, more antibiotics are used in animals than in humans. Livestock are often fed antibiotics not just to treat disease, but to promote growth and prevent infections in crowded, unsanitary conditions. This creates vast reservoirs of resistant bacteria, which can spread to humans through food, water, and the environment.
Waste from hospitals, farms, and pharmaceutical factories also leaks antibiotics and resistant bacteria into rivers and soil, turning nature into a breeding ground for resistance. The result: bacteria that were once easily defeated by a pill now survive treatments, spread rapidly, and cause infections that are harder, longer, and more expensive to treat.
Superbugs: When Bacteria Become Invincible
Some bacteria have become resistant to multiple antibiotics. These are known as multidrug-resistant (MDR) or extensively drug-resistant (XDR) bacteria—more commonly called superbugs. The most notorious include:
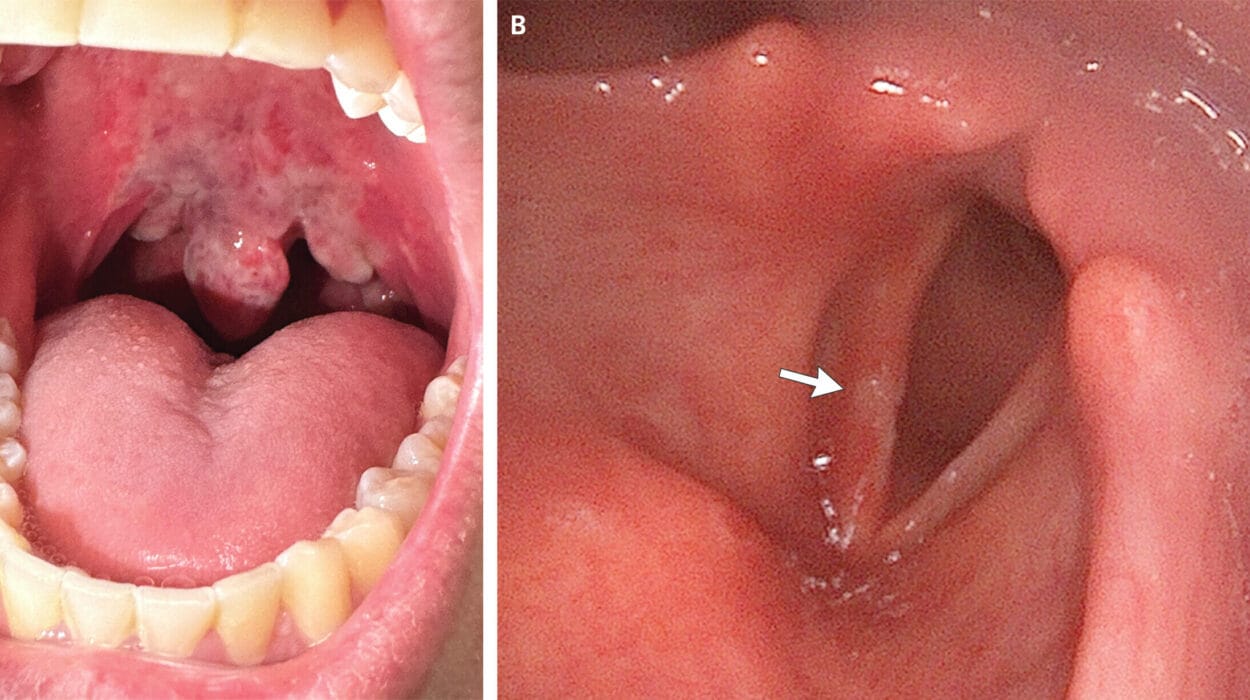
MRSA (methicillin-resistant Staphylococcus aureus)—a common hospital-acquired infection that resists many frontline antibiotics.
CRE (carbapenem-resistant Enterobacteriaceae)—a family of bacteria resistant to carbapenems, some of the most powerful antibiotics we have.
XDR-TB (extensively drug-resistant tuberculosis)—a form of TB that’s nearly impossible to treat with existing drugs.
These pathogens can cause deadly infections in hospitals, nursing homes, and intensive care units. But increasingly, they’re showing up in community settings, too. And they’re not just a problem in developing countries. The U.S. Centers for Disease Control and Prevention (CDC) estimates that more than 2.8 million antibiotic-resistant infections occur in the U.S. each year, killing at least 35,000 people.
Worldwide, the numbers are staggering. A 2019 study in The Lancet estimated that in 2019, nearly 5 million deaths were associated with antibiotic resistance, and 1.27 million were directly caused by it. If current trends continue, some experts predict that drug-resistant infections could kill 10 million people a year by 2050—more than cancer.
The Pipeline Problem: Why New Antibiotics Are Scarce
You might think the solution is simple: invent new antibiotics. But the reality is far more complex.
Antibiotic development is scientifically difficult and financially unrewarding. Most low-hanging scientific fruit has been picked; finding new antibiotic classes is challenging and time-consuming. Clinical trials are expensive, and antibiotics are typically used for short durations, unlike chronic medications that generate steady income.
Moreover, the moment a new antibiotic is approved, medical experts urge its limited use to preserve its effectiveness. That’s great for public health, but a disaster for profits. As a result, many pharmaceutical companies have abandoned antibiotic research altogether. Of the 18 largest pharmaceutical companies in the world, none has a robust antibiotic pipeline.
A few nonprofit and public-private partnerships are trying to fill the gap, but progress is slow. Without strong incentives, new antibiotics will remain scarce, and we’ll be stuck fighting superbugs with outdated weapons.
Fighting Back: Strategies to Combat Resistance
Despite the daunting challenge, hope is not lost. A multifaceted approach can turn the tide.
First, we must use existing antibiotics responsibly. This means prescribing them only when needed, using the right drug at the right dose for the right duration. It also means educating patients not to demand antibiotics for colds or flu, and to always complete their prescriptions.
Second, better diagnostics are crucial. Rapid tests that distinguish bacterial from viral infections can reduce unnecessary antibiotic use. Improved surveillance can help track resistance patterns and guide treatment.
Third, infection prevention is key. Vaccination, hand hygiene, sanitation, and infection control in hospitals can reduce the spread of resistant bacteria. Fewer infections mean less need for antibiotics.
Fourth, the agricultural sector must change. Many countries are banning the use of antibiotics for growth promotion, and some are tightening regulations on veterinary drug use. More sustainable farming practices can reduce dependence on antibiotics.
Finally, global cooperation is essential. Resistance knows no borders. Coordinated efforts—like the World Health Organization’s Global Action Plan on Antimicrobial Resistance—are vital to share data, fund research, and develop policies that protect the effectiveness of antibiotics for future generations.
The Role of the Public: Everyone Has a Part to Play
Antibiotic resistance isn’t just a problem for doctors, scientists, or governments. It’s a societal issue that demands awareness and action at every level. As individuals, we can:
- Avoid pressuring healthcare providers for antibiotics.
- Always follow prescriptions exactly.
- Never use leftover antibiotics or share them.
- Support vaccination efforts.
- Practice good hygiene and food safety.
Consumers can also influence corporate practices by choosing meat products raised without unnecessary antibiotics. Public pressure can drive policy changes, encourage responsible farming, and promote innovation.
The battle against resistance requires a cultural shift—a rethinking of how we view illness, medicine, and our place in the microbial world.
Looking Ahead: A Delicate Balance
Antibiotics are both a triumph of modern science and a cautionary tale. They gave us power over life-threatening diseases, but that power came with responsibility—a responsibility we haven’t always honored.
The future of antibiotics depends on our willingness to change. With careful stewardship, investment in innovation, and global solidarity, we can preserve these life-saving drugs for generations to come. But if we fail, we risk returning to a world where infections that once seemed trivial once again become deadly.
In the end, antibiotic resistance isn’t just about microbes. It’s a mirror reflecting our medical habits, our food systems, and our relationship with nature. The story is still being written—and we all have a role in how it ends.