Imagine walking into a pharmacy with a prescription in hand. You glance at the shelves filled with medications, and you’re presented with a choice: buy the brand-name drug your doctor prescribed, or opt for a much cheaper version labeled “generic.” The pharmacist assures you they’re the same. But something in you hesitates. If it’s cheaper, is it cutting corners? Is it really just as good?
This is the crossroads where millions of people around the world find themselves each year, and the answer isn’t just about chemistry—it’s about trust, regulation, economics, and, ultimately, your health.
Generic drugs are among the most misunderstood facets of modern medicine. They occupy a unique space in the pharmaceutical world—simultaneously praised for saving billions of dollars globally while also viewed skeptically by patients who worry about quality and effectiveness. To truly grasp the reality of generic drugs, we have to journey through the labyrinth of how drugs are made, approved, regulated, and sold. The truth is more fascinating—and more reassuring—than you might think.
Brand-Name Drugs: The Starting Line of Innovation
To understand generics, we must first step into the world of brand-name, or “innovator,” drugs. These are the medications that revolutionize treatments, offering hope where there was once despair—think of antibiotics, HIV antiretrovirals, or cancer immunotherapies. But before a single pill reaches a pharmacy shelf, it’s the product of years—often more than a decade—of scientific research, clinical trials, and meticulous testing.
Pharmaceutical companies invest heavily in developing a new drug. From the discovery of a promising molecule to the completion of rigorous clinical trials, the process can cost upwards of $1 to $2 billion. The U.S. Food and Drug Administration (FDA), and equivalent regulatory bodies around the world, scrutinize the data to ensure the drug’s safety and effectiveness.
Once approved, these brand-name drugs receive patent protection—essentially a government-granted monopoly—that typically lasts 20 years from the time of discovery. During this period, the manufacturer recoups its investment through market exclusivity. These are the expensive drugs your doctor prescribes—Pfizer’s Lipitor, AstraZeneca’s Nexium, or GSK’s Advair. Their brand names are memorable, marketed with flashy TV commercials, and trusted by physicians.
The Curtain Rises on Generic Drugs
When a brand-name drug’s patent expires, other pharmaceutical companies can apply to produce the same drug. This is where generics enter the scene. But what does it really mean to be “the same”?
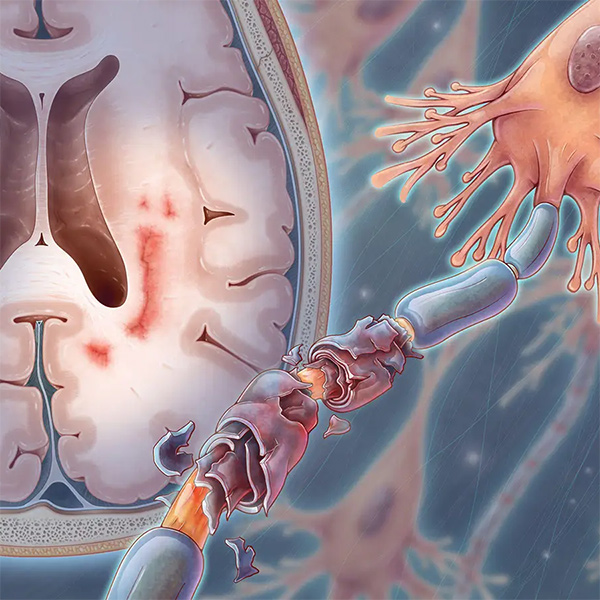
By law and regulatory standards, a generic drug must be “bioequivalent” to its brand-name counterpart. Bioequivalence means that the generic delivers the same amount of active ingredients into a patient’s bloodstream in the same amount of time as the original drug. It must have the same dosage form (pill, capsule, injection), strength, route of administration, and intended use.
In other words, the generic drug is chemically identical where it counts. The only differences allowed are in minor elements like fillers, coloring, and shape—details that don’t affect how the drug works in your body.
How Are Generics Approved? The Science Behind the Sameness
To ensure generics perform just like brand-name drugs, manufacturers must submit an Abbreviated New Drug Application (ANDA) to the FDA or relevant authorities like the EMA (European Medicines Agency). The “abbreviated” part is key—they don’t need to conduct full clinical trials again because those trials were already done for the original drug. Instead, generic manufacturers must demonstrate through rigorous laboratory testing and bioequivalence studies that their drug acts the same way in the body.
This involves studying how the drug is absorbed, how quickly it reaches peak concentration in the blood, and how long it stays in the system. If a generic’s performance falls within 80% to 125% of the original drug’s parameters—a standard scientifically proven to yield no meaningful clinical difference—it is approved.
Regulatory agencies also inspect generic manufacturing facilities with the same scrutiny as brand-name plants, ensuring that Good Manufacturing Practices (GMP) are followed meticulously.
Common Misconceptions About Generic Drugs
Despite this scientific backing, generic drugs face a branding problem—not the kind solved with marketing, but the psychological bias that leads people to believe that higher cost equals higher quality. It’s the same mindset that makes someone choose a $60 bottle of wine over a $15 one, assuming it must be better.
One major myth is that generics are less effective. Patients sometimes report differences in how they feel when switching from brand to generic, or between generics. These perceptions are often rooted in expectation bias. Studies show that when patients believe they’re taking a brand-name drug—even when it’s not—they report better outcomes than when they’re told it’s a generic. That’s the placebo effect at work, shaped by branding and perception, not pharmacology.
Another concern is about inactive ingredients. While these can differ, they rarely impact drug performance unless a patient has a specific allergy. Regulatory agencies monitor these components closely, and substitutions must not interfere with the drug’s delivery or effectiveness.
There are also persistent rumors about overseas manufacturing. While many generics are produced in countries like India or China, so are brand-name drugs. In fact, more than 80% of active pharmaceutical ingredients used in all drugs consumed in the U.S. are manufactured abroad. The key point is that all drugs, regardless of origin, must meet stringent quality standards to be sold in regulated markets.
Cost vs. Quality: Why Generics Are Cheaper
The dramatic price difference between generics and brand-name drugs often raises eyebrows. If they’re the same, why are they so much cheaper?
The answer lies in economics, not quality. Brand-name drug companies spend millions on R&D, clinical trials, and marketing. They charge higher prices to recoup these investments. Generic manufacturers don’t bear these initial costs. They also don’t usually advertise, and they compete in a price-driven market. This means they can sell the same medication at a fraction of the cost—often 80–90% cheaper.
This affordability has massive implications. In the U.S. alone, generics saved the healthcare system over $2.6 trillion between 2009 and 2020. For patients without insurance or those facing high co-pays, generics make life-saving medications accessible and sustainable.
Real-World Effectiveness: Do Generics Perform Equally?
Numerous studies have compared the effectiveness of generic versus brand-name drugs in real-world settings. A landmark review published in the Journal of the American Medical Association (JAMA) analyzed 38 clinical studies and concluded there was no significant difference in outcomes for patients using generic versus brand-name cardiovascular drugs—a category where precision is critical.
Similarly, for conditions like epilepsy, depression, diabetes, and high blood pressure, generics have shown consistent performance across populations. Regulatory bodies continuously monitor adverse events, and if a problem arises, generics can be recalled or production halted just like any drug.
Still, in rare cases, some patients do better on one version than another. This could be due to individual metabolism, allergies to certain inactive ingredients, or even psychological factors. In such situations, doctors can specify a particular manufacturer’s generic or recommend staying with a brand-name version when medically necessary.
The Global Landscape of Generic Drugs
Different countries have different relationships with generics. In the U.S., over 90% of all prescriptions filled are for generics. In Europe, the uptake varies—Germany and the U.K. are enthusiastic adopters, while others like Italy and France have historically lagged due to cultural preferences and branding influences.
In developing countries, generics play a critical role in public health. Programs like the World Health Organization’s Prequalification of Medicines initiative ensure that generics meet global standards for safety and effectiveness, making treatments for HIV, malaria, and tuberculosis accessible to millions at low cost.
India, often dubbed the “pharmacy of the world,” is a major producer of generics. Companies like Cipla and Sun Pharma manufacture high-quality generics for both domestic use and export. These companies have helped shift global attitudes toward generics, particularly in Africa and Southeast Asia.
Controversies and Legal Battles
The path of generic drugs hasn’t been entirely smooth. Brand-name manufacturers sometimes engage in tactics known as “evergreening”—making minor tweaks to their drugs or filing additional patents to extend exclusivity and delay generic competition.
There have also been cases of “pay-for-delay” agreements, where brand-name companies pay generic manufacturers to postpone launching a cheaper version. These practices are under increasing scrutiny by regulators and consumer rights groups, as they undermine the very purpose of generics.
Another concern has been data integrity and manufacturing practices in certain overseas plants. Regulatory agencies have increased global inspections, and high-profile investigations have led to recalls and penalties. While such issues are rare, they underscore the importance of vigilant oversight.
The Role of Pharmacists and Physicians
Your healthcare providers play a crucial role in guiding the use of generics. Physicians are encouraged to prescribe by generic name when possible, and pharmacists can often substitute a generic even if the brand-name is written on the prescription, depending on state laws.
Pharmacists also educate patients who are hesitant or confused. A well-informed pharmacist can explain bioequivalence, address concerns about side effects, and even identify cost-saving options for patients on complex drug regimens.
It’s also important for patients to communicate with their doctors if they notice any changes after switching to a generic. While most transitions are seamless, feedback ensures that any issues are caught early.
The Future of Generic Drugs
The future looks bright for generics, but challenges remain. As biologic drugs—complex medications made from living cells—become more common, the generic equivalent, called biosimilars, is emerging. Biosimilars are not exact copies due to the complexity of biologics but are highly similar in efficacy and safety.
Biosimilars offer enormous savings potential, particularly in oncology and autoimmune treatments. However, public awareness of biosimilars is still low, and regulatory pathways are evolving. Ensuring confidence in these products will be the next frontier in the generics movement.
Meanwhile, digital health tools are helping track medication effectiveness, monitor adverse reactions, and personalize treatment—regardless of whether a drug is generic or branded. This democratization of data could further close the gap in perception between generics and brand-name medications.
Conclusion: Generic Drugs—The Unsung Heroes of Healthcare
Generic drugs are not second-rate substitutes. They are the unsung heroes of modern medicine, quietly keeping healthcare systems afloat, extending lives, and making treatment affordable. They are born from science, approved through rigorous testing, and held to the highest manufacturing standards.
They may not come with glossy advertisements or celebrity endorsements, but they come with something far more valuable—accessibility. They represent the idea that medical innovation should not be a luxury, but a shared human right.
So, the next time you stand at the pharmacy counter with a choice between a brand-name and a generic, know that you’re not settling—you’re participating in one of the most remarkable achievements of modern healthcare: safe, effective medicine for all.