In a groundbreaking study published in Nature Neuroscience, researchers from the University of Geneva and École Polytechnique Fédérale de Lausanne have uncovered a startling new connection between the brain and the immune system: your body can mount an immune response to a threat it hasn’t physically encountered—simply by anticipating infection.
Using immersive virtual reality (VR), the team demonstrated that encountering a digitally simulated, infectious presence is enough to kick the immune system into action. It’s the first time science has shown that neural anticipation alone—without real pathogens—can trigger an immune cascade. And the implications could rewrite what we know about the boundaries between the mind and body.
Immune Cells That Don’t Wait for Proof
At the center of this discovery are innate lymphoid cells (ILCs)—a lesser-known class of immune cells that serve as first responders in the body’s defense system. Unlike T cells or B cells, which need to recognize specific antigens before springing into action, ILCs are instinctive and fast, reacting to general signs of tissue stress, infection, or inflammation.
In this new study, scientists showed that ILCs don’t just respond to actual infections—they also react to the brain’s anticipation of infection, revealing a stunning layer of neuro-immune interaction. When people feel like they might get sick—even in a virtual environment—the body doesn’t wait for proof. It gets ready.
Testing Immunity in the Metaverse
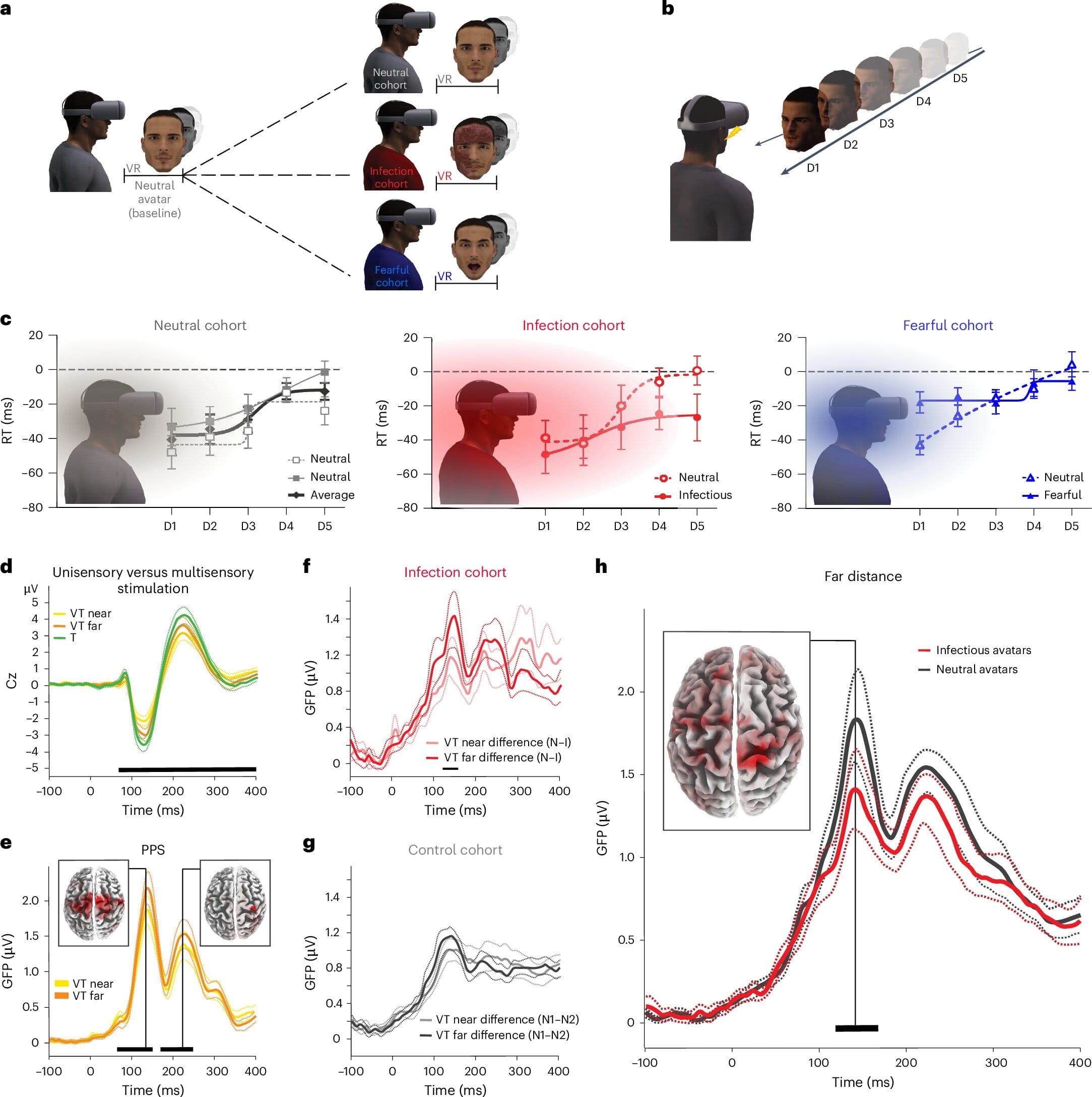
To test this theory, researchers designed a rigorous and richly multisensory experiment. Sixty healthy adults were immersed in a VR environment, where they encountered avatars that either appeared infectious (e.g., coughing, sneezing, showing signs of illness), neutral, or fear-inducing but not infectious. A fourth group was given an actual influenza vaccine to compare how the body reacts to real-world infection stimuli.
The team used a battery of state-of-the-art tools—electroencephalography (EEG), functional magnetic resonance imaging (fMRI), mass spectrometry, flow cytometry, and psychophysical testing—to monitor how the participants’ brains and immune systems responded.
Their most surprising finding? The immune system responded to virtual infection almost as if it were real.
Peripersonal Space: Where the Mind Draws the Line
Key to understanding this reaction is a concept called peripersonal space (PPS)—the invisible zone surrounding your body where the brain maps potential threats as they approach. This space isn’t just a passive boundary; it’s an active, flexible buffer where multisensory processing and survival mechanisms overlap.
Participants who encountered infectious avatars in VR displayed an expansion of this PPS, which could be measured through faster reaction times to touch, even when the avatars were further away. It’s as if their brains were subconsciously pushing out their sensory boundaries to give more reaction time in case of infection—just as they would in the face of a real biological threat.
This expansion of PPS correlated strongly with increased neural activity in areas of the brain that process salience, body awareness, and threat anticipation, such as the anterior insula and medial prefrontal cortex.
EEG and fMRI Show the Brain Lighting Up Before the Body Is Even Touched
Using EEG and fMRI, the researchers discovered that participants’ brains began showing anticipatory neural activity the moment the infectious avatars came into view. Even though no physical contact occurred, there was clear engagement in the multisensory-motor cortex, anterior cingulate cortex, intraparietal sulcus, and other areas involved in mapping body space and predicting threat.
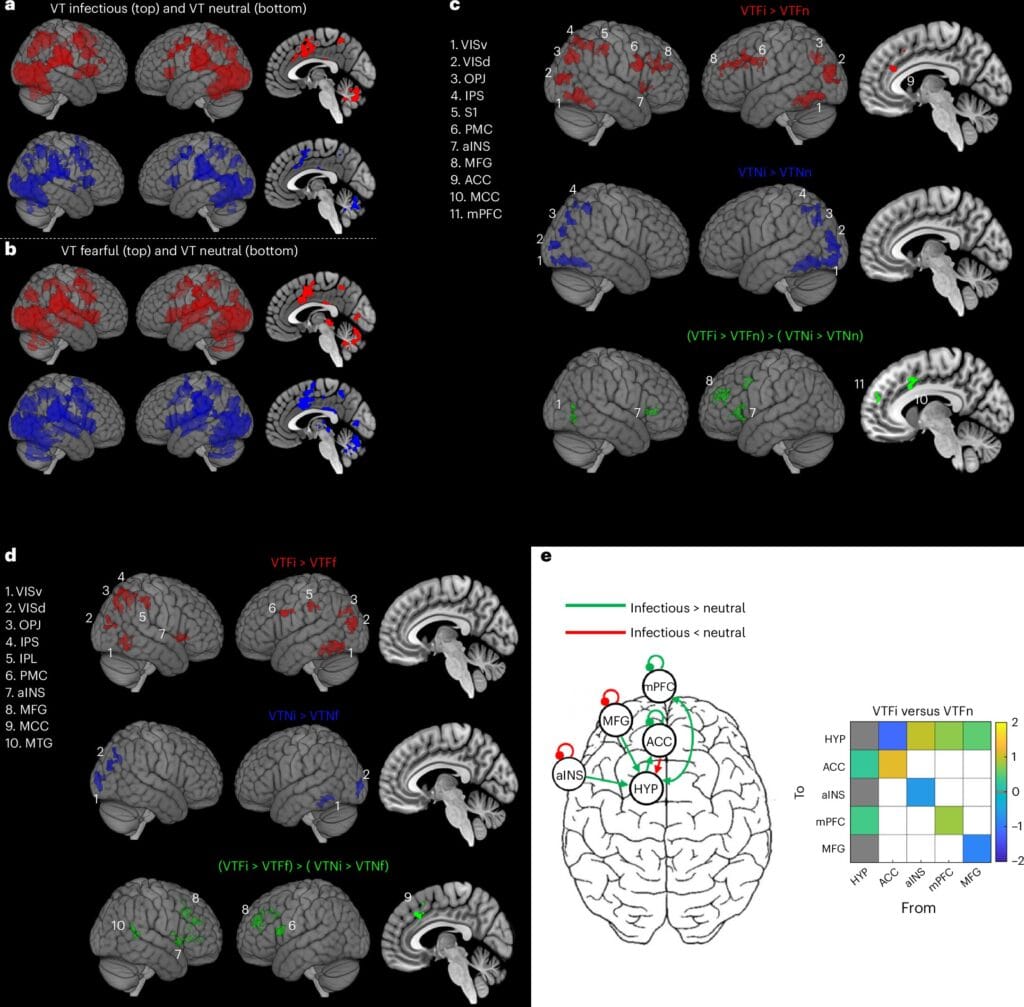
Dynamic causal modeling, a technique used to examine how brain regions influence each other, revealed altered connectivity between these brain areas and the hypothalamus, a key hub in the neuroendocrine system. This pathway, known as the hypothalamic-pituitary-adrenal (HPA) axis, plays a central role in coordinating the body’s stress and immune responses.
Simply put, the brain was not just imagining a threat—it was mobilizing the biological systems needed to defend against it.
Real Immune Shifts Without Real Infection
When researchers looked at the participants’ blood samples, the immune changes were unmistakable. People exposed to the infectious avatars experienced a marked modulation in their ILC populations. Specifically, there was a decrease in ILC1s, which are typically involved in fighting viral infections, and an increase in ILC2s and ILC precursors, which help orchestrate tissue repair and response to allergens.
These changes closely mirrored those seen in participants who received the actual influenza vaccine, albeit to a slightly lesser degree. The virtual threat triggered real, measurable changes in immune readiness—like a fire crew arriving before the alarm had even been sounded.
This immune modulation wasn’t just a stress response. When compared to participants who faced fearful but non-infectious avatars (like threatening or angry individuals), only the infectious avatars triggered this particular immune signature, highlighting the specificity of the anticipatory immune response.
A Brain That Learns to Defend Before It’s Attacked
This finding reframes how we think about the immune system’s relationship with the brain. While past research has shown how real infections can influence neural activity, this is one of the first demonstrations that neural anticipation alone can signal the immune system into a preparatory state.
In evolutionary terms, this makes perfect sense. Organisms that could anticipate danger—especially from pathogens that spread invisibly—would have had a survival advantage. If the immune system can be warned by the brain that an infection is likely based on environmental cues, it could prepare in advance, potentially stopping an illness before it even takes root.
Virtual Reality, Real Medicine?
While this research is deeply rooted in neuroscience and immunology, its potential applications go far beyond the laboratory. The possibility that virtual environments can modulate immune function raises fascinating questions for medicine, mental health, and technology.
Could VR be used to train the immune system, much like vaccines do, but without actual pathogens? Could people with immune deficiencies or chronic illnesses benefit from digital exposures that prime their defenses? And what of people who live in fear of illness—could their immune systems be chronically activated, with consequences for both their physical and mental health?
These are not science fiction questions anymore. They are scientifically grounded hypotheses born of a world where the brain and body are not separate realms but intimately intertwined players in our survival.
The Neuro-Immune Future Is Here
The study doesn’t just offer a peek into how our immune system works—it offers a glimpse of the future. A future where medicine and neuroscience converge, where VR and immunology dance, and where the boundary between thought and biology becomes ever thinner.
By demonstrating that the brain can preemptively activate the immune system through anticipation alone, this research opens a profound new chapter in human biology. It reminds us that health is not merely a physical state—it is also an experience, shaped by how we perceive the world and what we believe is coming next.
Your mind, it turns out, may be the best first line of defense your body has.
More information: Sara Trabanelli et al, Neural anticipation of virtual infection triggers an immune response, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-02008-y