Tucked deep inside the female reproductive system lies the cervix, a small, doughnut-shaped structure that plays a big role in your health. Despite its modest size—only about two to three centimeters in length—the cervix is a vital gatekeeper between the uterus and the vagina. It’s involved in menstruation, fertility, childbirth, and even serves as the first line of defense against infections and diseases. Yet for many women, the cervix remains somewhat of a mystery. You can’t see it. You can’t feel it. And unless something goes wrong, you probably don’t give it much thought.
But understanding your cervical health isn’t just about being aware of an organ buried in your pelvis—it’s about unlocking the knowledge to safeguard your reproductive system, prevent serious diseases like cervical cancer, and advocate for your own well-being during doctor’s visits. In a world where many conversations about women’s health are still clouded in taboo or misinformation, knowledge about the cervix can be liberating and even life-saving.
Getting to Know the Anatomy of the Cervix
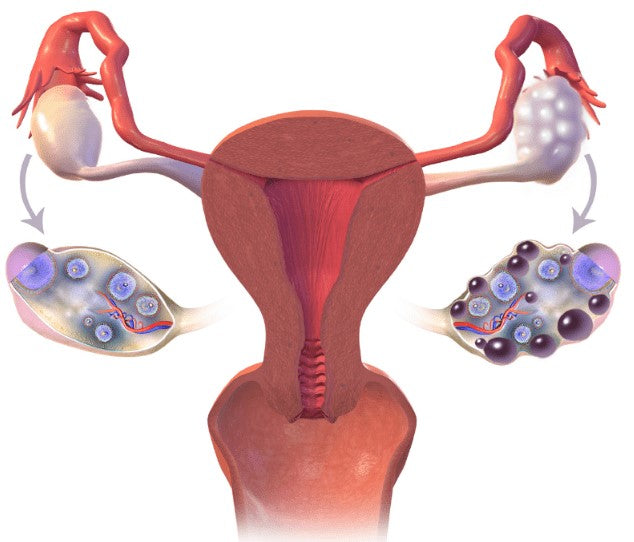
The cervix is part of the uterus and connects it to the vaginal canal. Anatomically, it’s divided into two parts: the endocervix, which is the inner part closest to the uterus, and the ectocervix, which is the outer part that protrudes into the vagina. These two regions are made up of different types of cells—columnar cells in the endocervix and squamous cells in the ectocervix. The place where these two cell types meet is called the transformation zone, and it’s a crucial area when it comes to cervical health because it’s particularly vulnerable to abnormal changes, including precancerous lesions.
What the cervix does depends heavily on your hormonal status. During your menstrual cycle, it produces different types of cervical mucus that either help sperm swim into the uterus or act as a barrier to block them. During pregnancy, the cervix becomes a tightly closed gateway to keep the fetus safe. And when it’s time to give birth, it performs a miraculous feat—it softens, dilates, and opens wide enough for a baby to pass through.
How Hormones Shape Cervical Health
Hormones are the silent orchestrators of your cervical health. Estrogen and progesterone, the two main female sex hormones, influence the cervix’s appearance, texture, and secretions throughout your menstrual cycle. In the follicular phase (the first half of your cycle), rising estrogen levels stimulate the cervix to produce thin, stretchy, and fertile-quality cervical mucus—sometimes described as resembling raw egg whites. This mucus makes it easier for sperm to reach the egg and fertilize it.
As ovulation passes and progesterone rises in the luteal phase, cervical mucus becomes thicker and more hostile to sperm, acting almost like a security guard to block the cervix from anything that doesn’t belong. If pregnancy occurs, the cervix creates a mucus plug that seals the uterus, protecting the developing baby. If pregnancy doesn’t occur, progesterone levels fall, the cervix softens again, and menstruation begins.
Hormonal shifts can also change the position and feel of the cervix—something that women practicing fertility awareness may track as part of understanding their cycles. These subtle but significant changes are a testament to the cervix’s responsiveness and the pivotal role hormones play in its function.
Cervical Mucus: Your Body’s Natural Communicator
Cervical mucus might not be glamorous, but it’s one of the best indicators of reproductive health you have. This often overlooked bodily fluid is like a window into what your hormones are doing. Paying attention to its texture, color, and consistency can tell you whether you’re ovulating, pregnant, or experiencing a hormonal imbalance.
For instance, dry or sticky mucus may indicate the beginning or end of a cycle, while creamy mucus suggests the fertile window is approaching. The slippery, clear, stretchy kind is a sign you’re most fertile. After ovulation, mucus typically becomes cloudy and thick again. But it’s not just fertility this mucus reflects. It can also be a warning sign when something is off. Changes in color, odor, or texture—like a sudden yellow, green, or foul-smelling discharge—can signal infections like bacterial vaginosis or sexually transmitted infections.
Learning to read your cervical mucus can empower you to track your cycle naturally, spot signs of fertility, and recognize when something is wrong before it becomes a bigger problem.
Pap Smears and Cervical Screenings: What They Really Tell You
If there’s one thing every woman hears about the cervix, it’s the Pap smear. This routine screening, named after Dr. George Papanicolaou, who developed the test, has been one of the most effective tools in the fight against cervical cancer. But many women dread or misunderstand it.
A Pap smear is a simple procedure where a healthcare provider gently scrapes cells from the cervix to examine them under a microscope. What they’re looking for are changes in those cervical cells—specifically abnormal cells that could become cancerous over time. These changes are often caused by persistent infections with certain strains of human papillomavirus (HPV).
The goal of the Pap smear isn’t just to detect cancer—it’s to catch the earliest signs of trouble, when the changes are still in a reversible, pre-cancerous stage. With regular screenings, most of these abnormalities can be managed long before they ever become dangerous. Cervical cancer often takes years to develop, so early detection is everything.
Cervical screenings may also include HPV testing, especially for women over 30. HPV tests identify whether high-risk strains of the virus are present in the cervical tissue. When combined with Pap smears, HPV testing gives a more complete picture of cervical health and cancer risk.
The Role of HPV in Cervical Health
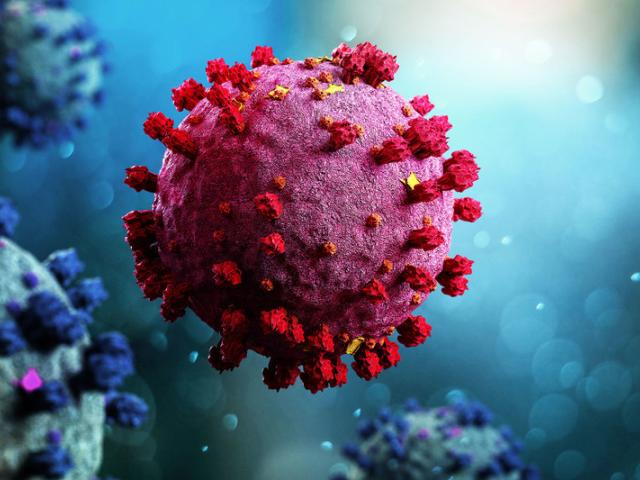
Human papillomavirus (HPV) is a common virus, so common that most sexually active people will contract it at some point. For many, it causes no symptoms and clears on its own. But certain high-risk strains can linger and cause cervical cell changes that may progress to cancer if not detected and managed.
HPV is primarily spread through skin-to-skin contact during sex, and it doesn’t always require penetration to be transmitted. That’s why condoms, while helpful, don’t offer full protection. The types of HPV most associated with cervical cancer are strains 16 and 18, which together account for roughly 70% of all cervical cancer cases.
Fortunately, there’s a powerful tool to fight back: the HPV vaccine. Vaccination can prevent infection with the most dangerous HPV strains and significantly reduce the risk of developing cervical and other anogenital cancers. It’s most effective when given before sexual activity begins, but even women who are already sexually active can benefit from it. The CDC now recommends HPV vaccination up to age 45 in some cases, especially if the individual hasn’t been previously vaccinated.
Cervical Cancer: Prevention, Symptoms, and Risk Factors
Cervical cancer doesn’t usually cause noticeable symptoms in its early stages, which is why screening is so important. When symptoms do appear, they may include abnormal vaginal bleeding (especially after sex), pelvic pain, or unusual discharge. These symptoms can also be caused by less serious conditions, but they should always be checked out.
Several risk factors can increase the likelihood of developing cervical cancer, including persistent high-risk HPV infection, smoking, a weakened immune system, long-term use of oral contraceptives, and having multiple sexual partners. However, having one or more of these factors doesn’t mean a woman will definitely get cancer—just that extra vigilance is needed.
Preventing cervical cancer is largely about routine care and informed choices. Regular screenings, HPV vaccination, practicing safe sex, and not smoking are some of the most effective strategies. Advances in science and medicine mean that cervical cancer is one of the most preventable and treatable forms of cancer, particularly when caught early.
The Cervix Through Life’s Stages
Your cervix changes as you age, and each stage of life brings its own set of concerns and considerations. In adolescence and early adulthood, the cervix is more exposed and sensitive, making younger women more susceptible to HPV infections and related changes. That’s why early vaccination and education are so critical.
In your reproductive years, your cervix undergoes monthly transformations influenced by hormones. It also plays a starring role in pregnancy and childbirth, softening and dilating to allow life to pass through. After giving birth, the cervix undergoes healing and reshaping, though it may never return to its exact pre-pregnancy state.
As menopause approaches, estrogen levels decline, leading to changes in the cervix and vaginal tissues. The cervix becomes less elastic, the canal may narrow, and mucus production drops. These changes can make sex more uncomfortable and Pap smears more difficult. However, staying sexually active, using vaginal moisturizers or hormone therapy (when appropriate), and continuing with regular screenings can help maintain cervical health post-menopause.
When the Cervix Speaks: Listening to Symptoms
While cervical health issues often begin silently, your body usually tries to send warning signs. Paying attention to subtle changes can help you detect problems early. Pain during intercourse, persistent pelvic discomfort, irregular bleeding, or foul-smelling discharge should never be ignored. They may point to infections, polyps, fibroids, or even early signs of malignancy.
Abnormal Pap smear results don’t automatically mean you have cancer. They’re a signal that something needs closer inspection. You may be asked to undergo further testing, like a colposcopy (where the cervix is examined under magnification) or a biopsy (where a small tissue sample is taken). These follow-up procedures allow your healthcare provider to understand the nature and severity of any abnormal cells and determine what treatment, if any, is needed.
Treating Cervical Conditions: From Infections to Dysplasia
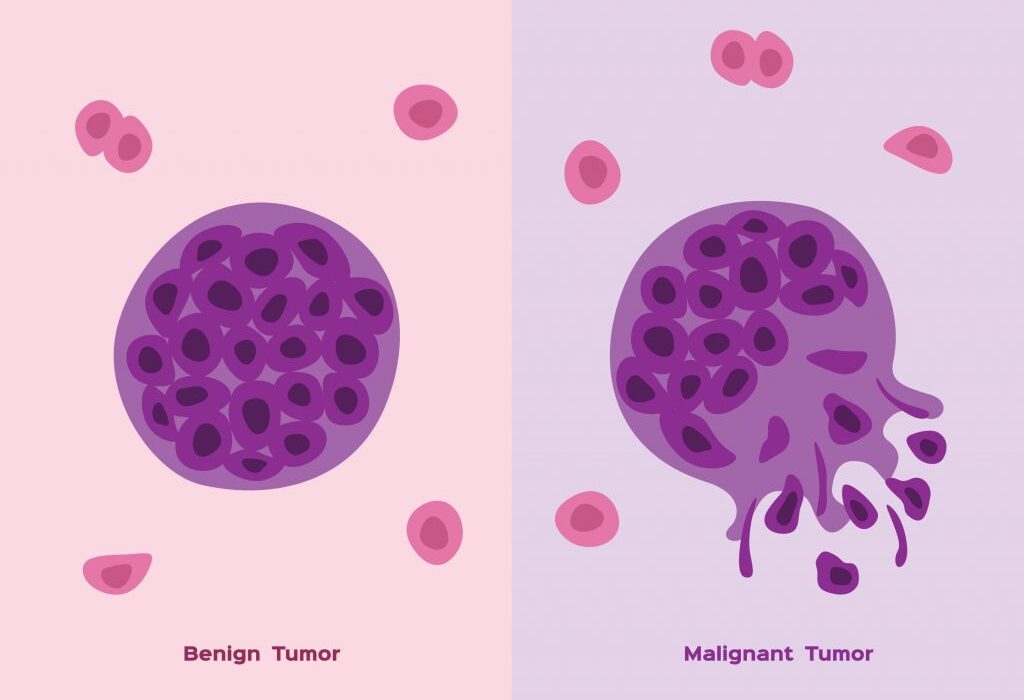
Cervical health challenges range from benign infections to precancerous changes called cervical dysplasia. The good news is that many of these issues are treatable—especially when caught early. Yeast infections, bacterial vaginosis, and sexually transmitted infections like chlamydia or gonorrhea can usually be cleared with medication.
When it comes to dysplasia—abnormal cell changes that can be mild, moderate, or severe—treatment depends on how far the changes have progressed. Mild dysplasia may resolve on its own, particularly in younger women. Moderate to severe cases may require procedures like cryotherapy (freezing), LEEP (loop electrosurgical excision procedure), or even conization (removing a cone-shaped piece of tissue) to eliminate the abnormal cells.
These procedures are typically done on an outpatient basis and are highly effective. Still, they can affect future fertility or cervical strength, so decisions about treatment should be made with both short-term and long-term health in mind.
Empowerment Through Education and Advocacy
Understanding your cervical health is about more than anatomy or medical procedures—it’s about empowerment. It’s about knowing what’s normal for your body, what changes to watch for, and what questions to ask your doctor. It’s about shaking off the stigma that still surrounds female reproductive health and speaking up when something doesn’t feel right.
Far too many women avoid cervical screenings due to fear, discomfort, or embarrassment. But armed with knowledge, the experience becomes less daunting. You are not just a passive patient in the exam room—you are an active participant in your own health. When you understand the language of your body, you can advocate for better care, better access, and better outcomes.
The Future of Cervical Health: Innovations and Hope
Medical science is evolving, and so is cervical healthcare. Self-sampling HPV tests, home screening kits, and more personalized treatment options are on the horizon. These innovations could make it easier for more women, especially those in underserved communities, to access life-saving care.
There’s also growing recognition that cervical health is tied to broader issues—access to education, healthcare equity, and reproductive rights. The World Health Organization has even launched a global strategy to eliminate cervical cancer as a public health issue within the next century. This vision is ambitious but achievable with continued research, outreach, and public health investment.
Conclusion: Your Cervix, Your Health, Your Power
The cervix may be a small part of your body, but it holds enormous importance. From facilitating conception to protecting pregnancies, from responding to hormones to alerting you when something’s wrong, it is a remarkably dynamic organ.
By understanding your cervical health—how it works, how to care for it, and when to seek help—you step into a powerful role in your own healthcare journey. You don’t need to be a doctor or a scientist to understand your body. You just need to be curious, attentive, and proactive. Because your health, your comfort, and your future are worth it.