Every human body tells a story. Under the skin, beneath the muscles, in every drop of blood or slice of tissue lies a narrative waiting to be read. It is a story of balance, function, adaptation, and—sometimes—disruption. And when that story takes a dark turn, when a cough becomes cancer, or fatigue masks a fatal disease, it is the science of pathology that deciphers the message.
Pathology is the beating heart of modern medicine—the often unseen but absolutely critical field that explains why we get sick and how we can be treated. If doctors are the detectives of disease, pathologists are the forensic scientists working tirelessly in the background, uncovering the microscopic clues that solve the mystery.
Yet, despite its importance, pathology remains one of the least understood branches of medicine to the general public. In this article, we’ll embark on a journey into the fascinating world of pathology—what it is, how it works, its history, its heroes, and why no diagnosis can truly exist without it.
What Is Pathology?
At its core, pathology is the scientific study of disease. The word itself comes from the Greek pathos (meaning suffering or disease) and logos (meaning study). But don’t let the ancient etymology fool you—modern pathology is a cutting-edge discipline that blends biology, chemistry, and advanced technology to understand how diseases originate, develop, and affect the body.
Pathology does not treat patients directly in the way a cardiologist or surgeon might. Instead, it operates behind the scenes, providing crucial insights that guide diagnosis, prognosis, and treatment decisions. Pathologists examine everything from a simple skin biopsy to complex molecular patterns in cancer cells. Their analyses determine whether a patient has pneumonia or lung cancer, appendicitis or Crohn’s disease, a benign tumor or a deadly one.
In short, pathology answers the fundamental question: What’s wrong?
The Subfields of Pathology: A Universe Within a Discipline
Like medicine itself, pathology is vast and divided into specialized branches. Each one explores disease through a different lens, focusing on particular body systems, techniques, or types of analysis.
Anatomical Pathology
Anatomical pathology deals with the structural changes in cells, tissues, and organs caused by disease. It’s the branch most people imagine when they think of pathology—microscopes, slides, and stained tissues.
When a patient has a lump removed, a mole biopsied, or an organ taken out during surgery, that sample goes to an anatomical pathologist. Using various techniques, including gross examination (visible to the naked eye), microscopic analysis, and chemical staining, the pathologist determines whether the tissue is normal or diseased—and if diseased, how severely.
Clinical Pathology
Clinical pathology is all about laboratory analysis. Clinical pathologists oversee hospital labs that process blood, urine, and other bodily fluids to detect infections, monitor chronic diseases, or spot abnormal chemistry.
They might identify a dangerous electrolyte imbalance, confirm a viral infection like HIV, or evaluate the severity of diabetes. Clinical pathologists also run hematology labs, analyzing blood cells to diagnose leukemia or anemia.
Molecular Pathology
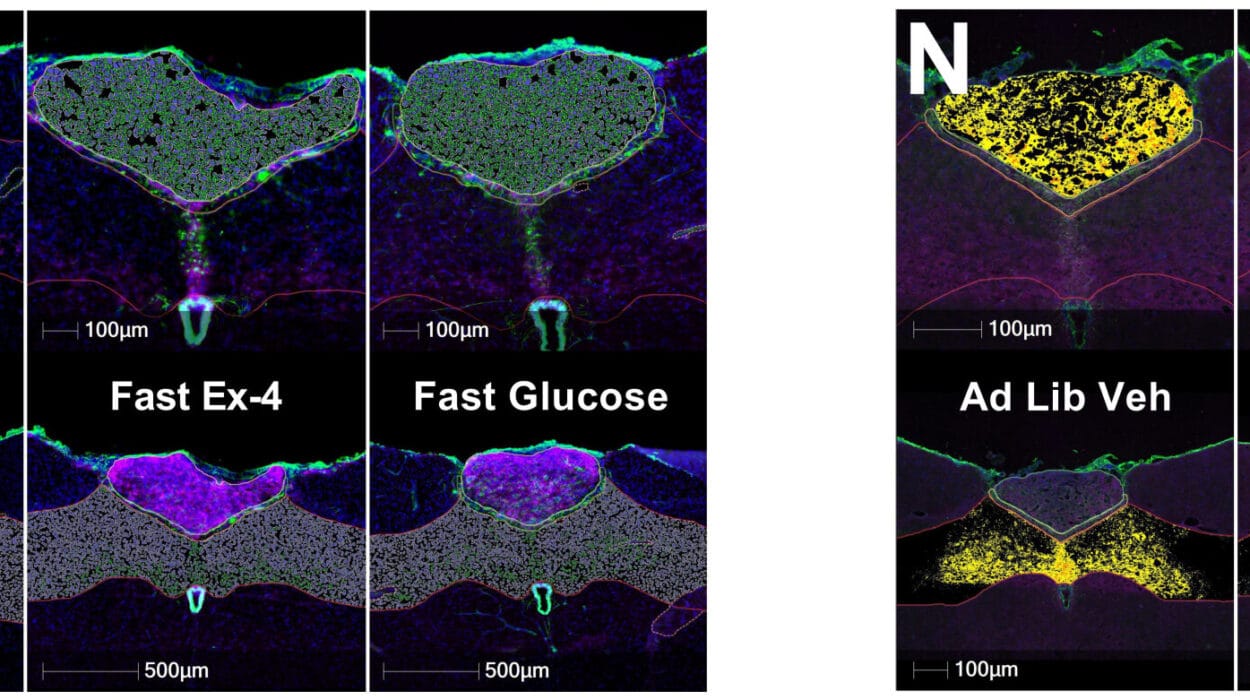
A newer and rapidly growing field, molecular pathology zooms in even further—down to genes and molecules. It employs DNA sequencing, PCR testing, and other genetic tools to uncover the mutations and molecular signatures behind diseases.
This subfield is especially vital in cancer care, where treatment decisions increasingly depend on the genetic profile of a tumor. If a lung cancer contains a specific mutation (like EGFR or ALK), a molecular pathologist helps identify it so targeted therapies can be used.
Forensic Pathology
While most pathologists diagnose diseases in the living, forensic pathologists investigate the dead. These are the medical examiners who perform autopsies, determine cause of death, and assist in criminal investigations.
From suspicious deaths to mass disasters, forensic pathologists bring medical clarity to some of society’s darkest moments.
Veterinary Pathology
Not all pathology deals with humans. Veterinary pathologists study diseases in animals, from domestic pets to livestock and wildlife. Their work is vital for animal health and helps prevent the spread of zoonotic diseases (those that can jump from animals to humans), such as rabies, avian flu, or COVID-19.
A Day in the Life of a Pathologist
While many imagine pathologists as lab-bound introverts peering endlessly through microscopes, the truth is far more dynamic. Their day might begin with case sign-outs, reviewing slides and dictating diagnostic reports. They often consult with surgeons, oncologists, and radiologists in tumor boards—multidisciplinary meetings where patient treatment strategies are debated.
Pathologists may also supervise technologists, ensure lab accuracy, troubleshoot machines, conduct research, or teach medical students. Their work is both cerebral and collaborative. Every diagnosis they make can alter a patient’s fate.
It’s also not uncommon for a pathologist to make a life-saving call—catching a rare cancer that others missed, identifying a deadly infection in a blood smear, or recognizing a genetic disorder that affects an entire family.
Diagnosing Disease: From Biopsy to Report
Let’s walk through a real-world scenario to see how pathology transforms a patient’s symptoms into a diagnosis.
Imagine a middle-aged woman who discovers a lump in her breast. Her doctor orders a core needle biopsy, which retrieves a small cylinder of tissue from the lump. That tissue is sent to the pathology lab.
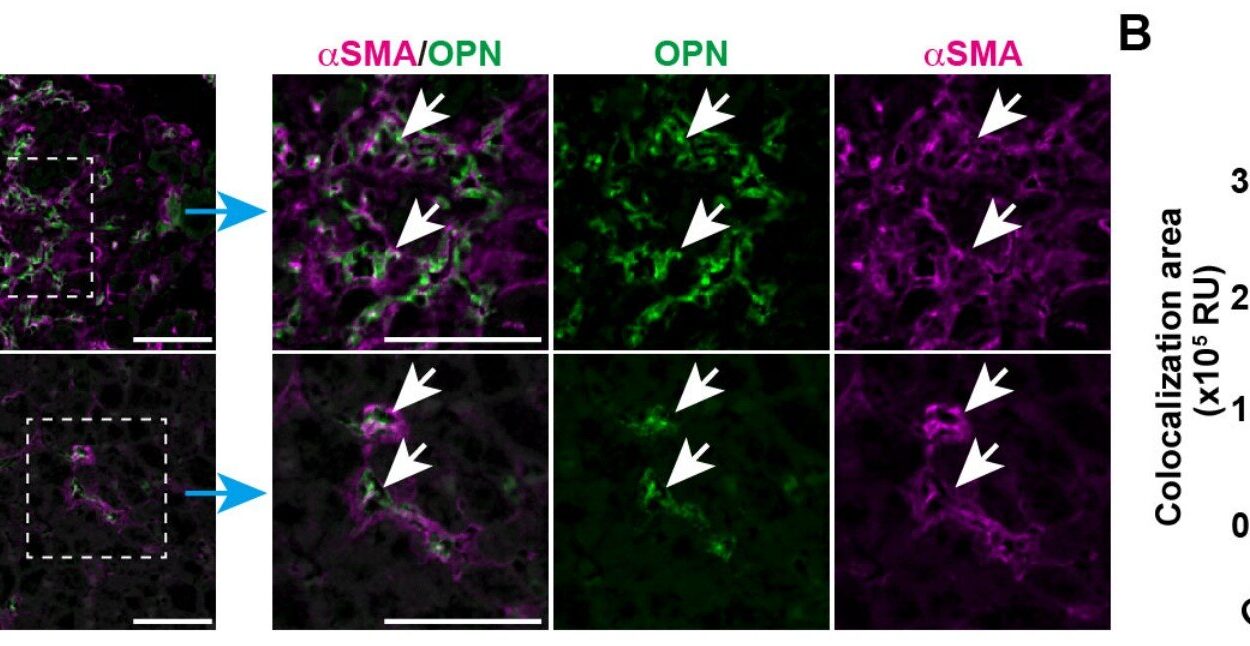
First, the specimen is handled by a histotechnologist, who embeds it in paraffin wax, slices it thinly, and stains it with dyes like hematoxylin and eosin (H&E). These stains help highlight cellular structures under the microscope.
The prepared slide is then examined by a pathologist, who looks for signs of cancer: irregular nuclei, loss of cellular organization, rapid cell division. If cancer is present, the pathologist will specify the type (e.g., ductal carcinoma), the grade (how aggressive it appears), and whether the margins (edges) are clean.
Often, additional immunohistochemistry is done—staining the tissue for specific proteins that indicate hormone sensitivity (e.g., estrogen or HER2 receptors). These markers guide treatment decisions.
In some cases, molecular testing may follow to look for mutations like BRCA1/2 or PIK3CA. Finally, a comprehensive pathology report is written and shared with the treating physician, who uses it to tailor the patient’s therapy.
This process—from biopsy to final diagnosis—is the foundation upon which all cancer care is built.
The Language of Disease
Pathology has its own rich and precise vocabulary. A good pathologist must be fluent in this language, using it to paint an accurate and concise picture of what’s happening inside a patient’s body.
Consider these commonly used terms:
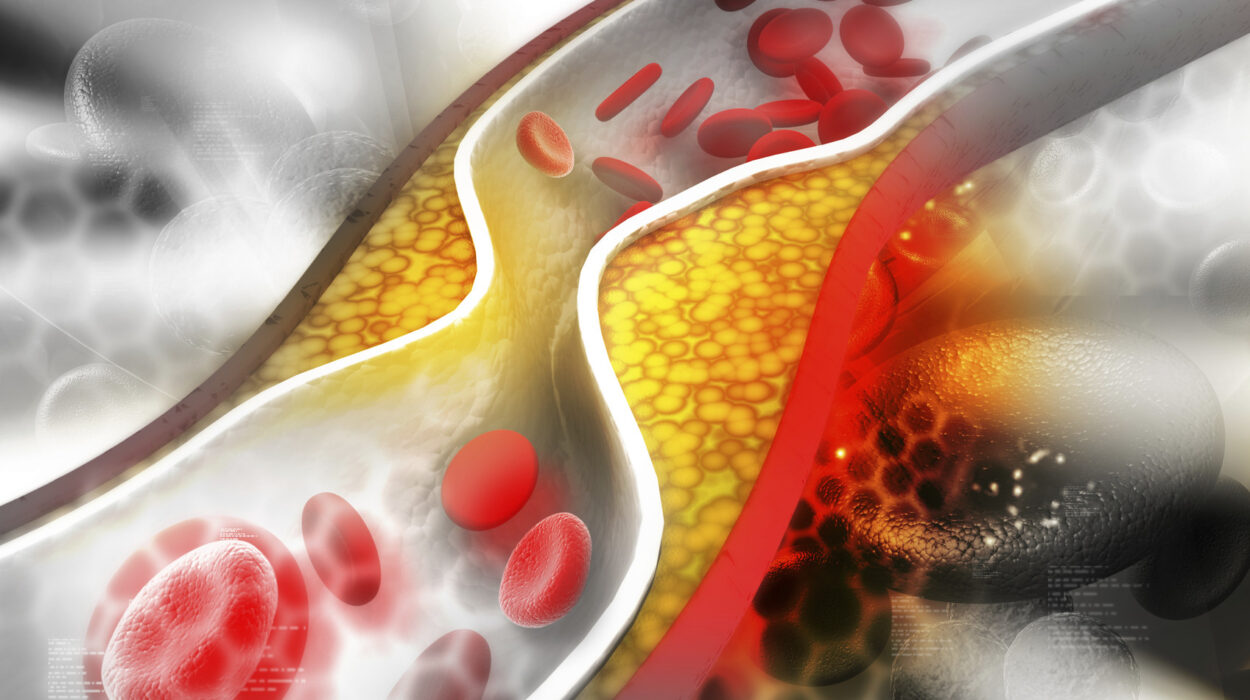
- Inflammation: The body’s immune response to injury or infection.
- Neoplasia: Uncontrolled growth of cells, potentially leading to tumors.
- Necrosis: Premature or pathological cell death.
- Dysplasia: Abnormal cellular growth, often precancerous.
- Metaplasia: One type of cell transforming into another, typically as an adaptation to chronic irritation.
Each term conveys subtle nuances that can influence treatment. Saying “low-grade dysplasia” vs. “invasive carcinoma” is like the difference between a cracked window and a demolished house. It changes everything.
Pathology in the Age of Technology
Like all sciences, pathology is evolving rapidly. The digital revolution is transforming how pathologists work, diagnose, and even collaborate.
Digital pathology now allows slides to be scanned and viewed on a screen. This means pathologists can share images worldwide, enabling remote consultations and second opinions in real time. It also facilitates machine learning, where AI algorithms help detect cancer, count cells, and analyze patterns.
Whole-genome sequencing is giving pathologists the ability to understand disease at the deepest level. Rather than merely seeing what’s wrong under the microscope, they can now know why it went wrong, down to the mutations that triggered it.
Liquid biopsies, where blood is tested for circulating tumor DNA, are emerging as non-invasive tools for early cancer detection—something that could revolutionize diagnosis and monitoring.
Still, technology doesn’t replace the pathologist. It enhances them. Human insight, experience, and clinical context remain irreplaceable in making sense of complex diseases.
The History of Pathology: From Autopsies to Algorithms
Pathology has a long and storied past, intertwined with the evolution of medicine itself.
In ancient times, the concept of disease was shrouded in mysticism. Hippocrates and Galen laid early foundations, but it wasn’t until the Renaissance that human dissection became accepted and pathology as a science began to blossom.
In the 17th century, Giovanni Morgagni performed hundreds of autopsies, correlating symptoms with post-mortem findings. His 1761 book, De Sedibus et Causis Morborum, is considered the birth of pathological anatomy.
In the 19th century, Rudolf Virchow revolutionized medicine by introducing the idea that disease occurs at the cellular level. His work laid the foundation for modern histopathology.
The 20th century saw the rise of molecular biology, staining techniques, electron microscopy, and immunohistochemistry. By the 21st century, pathology had become a hybrid of art, science, and technology.
Pathology and Public Health
Beyond individual diagnosis, pathology also plays a vital role in epidemiology and public health. During outbreaks—from Ebola to COVID-19—it’s pathologists who first identify the virus, understand its transmission, and monitor its mutations.
Autopsies help track emerging diseases. Biopsies reveal patterns of environmental illness. Blood tests identify nutritional deficiencies or toxic exposures.
Pathology is the backbone of screening programs: Pap smears for cervical cancer, blood tests for hepatitis, colonoscopies for polyps. These efforts have saved millions of lives.
Ethical Dilemmas and Challenges
As with any medical field, pathology is not without its challenges.
The rise of genetic testing raises questions about privacy, consent, and the psychological burden of knowing one’s future risks. Should you be told you carry a gene for Alzheimer’s, even if there’s no cure? Should relatives be informed?
In forensic pathology, decisions about cause and manner of death can have legal implications—potentially exonerating or condemning a suspect. Accuracy and impartiality are paramount.
And there’s the human factor: the burden of being the final arbiter. A misdiagnosis in pathology can mean a missed cancer—or unnecessary surgery. Pathologists must be cautious, collaborative, and continually educated.
Conclusion: Seeing the Invisible
Pathology is the soul of medicine’s scientific method. It transforms illness into information. It makes the invisible visible. It reveals the truth of the human body—both its triumphs and its tragedies.
Though it may work in the shadows, away from the patient’s bedside, pathology touches every corner of healthcare. Every diagnosis, every prognosis, every treatment owes its precision to the quiet expertise of pathologists.
In the age of personalized medicine, where treatments are tailored to each individual’s biology, pathology will only grow more essential. It is the gateway to understanding disease—not as a mysterious curse, but as a solvable puzzle.
And as our tools improve, as our data deepens, as our knowledge expands, one thing remains constant:
The quest to understand what ails us—and to heal.