Imagine a quiet revolution in women’s health—one so subtle and routine that many women barely pause to consider its life-saving potential. That revolution is the Pap smear, also known as the Pap test, and it has become one of the most powerful tools in modern preventive medicine. Though it takes just a few minutes and may cause minor discomfort, this simple test has dramatically reduced the number of deaths from cervical cancer, particularly in countries where screening is readily accessible.
The Pap smear is a test designed to detect changes in the cells of the cervix—the lower part of the uterus that opens into the vagina. These cellular changes can indicate the presence of precancerous or cancerous conditions, making it possible to treat issues before they evolve into more serious diseases. Developed in the 1940s by Dr. George Papanicolaou (hence the name), the Pap smear transformed cervical cancer from a leading cause of death into one of the most preventable forms of cancer in women.
Yet despite its critical importance, the Pap smear remains a misunderstood and, at times, underutilized screening tool. For many women, anxiety, myths, cultural taboos, or simple lack of information create barriers to scheduling regular exams. This article dives deep into the history, purpose, procedure, and profound impact of the Pap smear, while also addressing the social and emotional realities that surround it.
Cervical Cancer: A Silent Threat
To understand the significance of a Pap smear, it’s essential to grasp what it helps prevent. Cervical cancer doesn’t usually announce itself loudly in its early stages. It often starts with subtle changes in cervical cells that progress slowly over time. These changes may begin as dysplasia—a medical term for abnormal but non-cancerous cells. If left unchecked, these cells can eventually become cancerous and spread to other parts of the body.
Cervical cancer is almost always caused by persistent infection with the human papillomavirus (HPV), a group of viruses transmitted primarily through sexual contact. While many people contract HPV at some point in their lives and most infections resolve on their own, some high-risk strains can linger and lead to cancer. The beauty of the Pap smear is that it allows doctors to detect cell changes caused by HPV before cancer even develops.
This early detection makes cervical cancer one of the most preventable and treatable cancers. When caught in its precancerous stages, treatment is usually straightforward and highly effective. When detected early in its cancerous form, survival rates are dramatically higher. The key, of course, is catching it early—and that’s where the Pap smear comes in.
How the Pap Smear Works: From Sample to Science
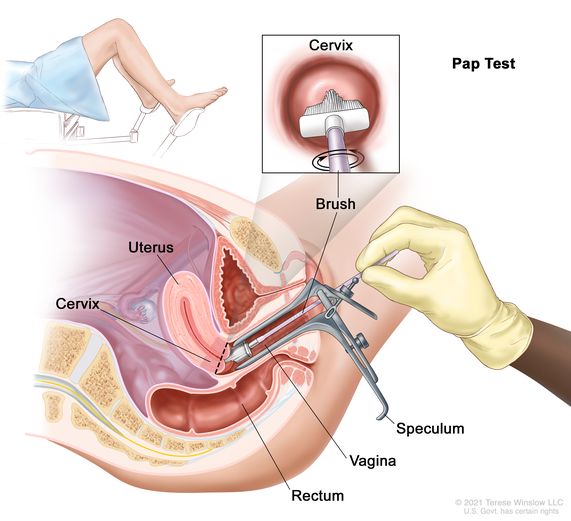
The mechanics of a Pap smear are deceptively simple. During a routine pelvic exam, your healthcare provider uses a speculum to gently widen the vagina and access the cervix. Then, using a small brush or spatula, they collect a sample of cells from the cervical surface. This sample is preserved and sent to a laboratory, where cytologists examine it under a microscope for any signs of abnormality.
From the patient’s perspective, the process may feel invasive, awkward, or slightly uncomfortable—but it is typically brief and painless. The entire collection procedure takes only a few minutes. For many, the emotional discomfort of the exam may outweigh any physical sensation. But within that tiny swab lies an enormous amount of information about your body’s cellular health.
Lab technicians look for several key features: Are the cells shaped normally? Are there any signs of inflammation, infection, or abnormal growth? Are there cells that suggest pre-cancerous or cancerous changes? Depending on the results, your healthcare provider may recommend further testing, such as an HPV test or a colposcopy (a closer examination of the cervix), or simply advise you to return in a few years for another routine screening.
The Evolution of the Pap Smear: A Test That Changed Women’s Health Forever
Before the advent of the Pap smear, cervical cancer was one of the most common causes of cancer-related death among women. Dr. George Papanicolaou’s breakthrough—his ability to identify pre-cancerous cells through a microscope—changed everything. His work in the 1920s and 1930s was initially met with skepticism, but over time, the medical community began to recognize its value. By the mid-20th century, the Pap smear was widely adopted, and the rates of cervical cancer began to plummet in countries where regular screening was implemented.
The success of the Pap smear is a testament to the power of preventive medicine. Unlike treatment-focused care that intervenes after disease appears, screening empowers individuals to detect potential problems before symptoms begin. This shift from reactive to proactive care has saved countless lives.
What’s equally fascinating is how the Pap smear has evolved over time. Originally analyzed by human eyes under a microscope, newer techniques such as liquid-based cytology and automated screening systems have made the process faster and more accurate. When combined with HPV testing—a practice increasingly used alongside the Pap smear—the screening becomes even more powerful, allowing for a more comprehensive assessment of cervical cancer risk.
Why Regular Pap Smears Matter: It’s Not Just One and Done
One of the common misconceptions about Pap smears is that a single test offers lifetime protection. While it’s reassuring to receive normal results, cervical cells can change over time, particularly in response to factors like HPV infection, sexual activity, smoking, immune suppression, or hormonal changes.
Most health organizations recommend that women begin Pap smear screening at age 21, regardless of sexual activity. From ages 21 to 29, a Pap smear every three years is generally sufficient if previous tests are normal. Between 30 and 65, women may be advised to have a Pap smear every three years, or to have both a Pap smear and an HPV test every five years—a strategy known as co-testing. After 65, women who have had consistently normal results may no longer need screening, depending on their health history.
These guidelines are designed to balance the benefits of early detection with the risks of over-testing, which can sometimes lead to unnecessary procedures or anxiety. Regular screening ensures that changes are caught early, before they become dangerous. Skipping years, however, increases the likelihood of missing crucial warning signs. The regularity of screening is not just a bureaucratic box to check; it’s a life-saving rhythm.
Beyond Cancer: What Else Can a Pap Smear Reveal?
While the primary goal of a Pap smear is to screen for cervical cancer, the exam can sometimes uncover other health concerns. Inflammation, infections like yeast or bacterial vaginosis, and even changes caused by hormonal fluctuations can all be detected during a Pap test. Though these conditions are usually benign, identifying them early can help prevent discomfort, complications, or further health issues.
In some cases, your healthcare provider may suggest additional testing based on what’s found. For instance, if your Pap smear shows signs of an HPV infection or if there are mild abnormalities, you may undergo a repeat test in a few months or a colposcopy to take a closer look. The point is not to alarm, but to monitor. Early, cautious observation is one of the greatest gifts of modern gynecological care.
Importantly, it’s also a chance for conversation. The Pap smear appointment opens the door to discussions about reproductive health, menstrual cycles, contraception, and any unusual symptoms you might be experiencing. It’s a powerful opportunity to advocate for your own health.
Emotional Realities: Anxiety, Stigma, and the Need for Compassion
Despite its routine nature, the Pap smear is not emotionally neutral for everyone. Some women experience significant anxiety around the procedure. For survivors of sexual trauma, the thought of a pelvic exam can be deeply distressing. Others may feel embarrassed, fearful of pain, or worried about what the results might reveal.
Cultural stigma also plays a role. In some communities, discussions about sexual health are taboo, and undergoing a Pap smear can be misunderstood as a marker of sexual activity or promiscuity. Such misconceptions create a barrier to care, particularly for young women and those from conservative backgrounds.
Healthcare providers have a responsibility to approach this procedure with empathy, patience, and clear communication. Explaining the process, allowing time for questions, and creating a safe, respectful environment can significantly reduce anxiety. For patients, it’s okay to speak up, express discomfort, and ask for a female provider or someone experienced in trauma-informed care.
Normalizing the Pap smear—not just medically, but socially and emotionally—is essential to ensuring that every woman feels empowered to protect her health.
Barriers to Access: When Routine Isn’t So Routine
While the Pap smear is a cornerstone of preventive health in many developed countries, access is far from universal. In low-income regions, rural communities, and among uninsured populations, screening remains inconsistent. Factors like cost, transportation, availability of trained providers, and lack of awareness all contribute to lower screening rates.
The consequences are devastating. In places where Pap smears are rarely done, cervical cancer remains one of the leading causes of cancer-related death in women. This disparity is particularly heartbreaking because it’s preventable. Public health campaigns, mobile screening units, and self-sampling kits are beginning to make a difference, but much more work is needed to close the gap.
Technology offers hope. Innovations such as AI-powered diagnostic tools, smartphone-enabled screening, and low-cost HPV tests are making it easier to bring effective screening to underserved areas. But technology must be paired with education, infrastructure, and cultural sensitivity to have lasting impact.
The Role of the HPV Vaccine: A Powerful Ally in Prevention
The Pap smear doesn’t exist in isolation. Over the past two decades, the introduction of the HPV vaccine has added a powerful new layer of protection. The vaccine targets the most dangerous strains of HPV—those most likely to cause cervical cancer—as well as those responsible for genital warts.
Vaccination is recommended for boys and girls starting around age 11 or 12, before they become sexually active, although it can be given as late as age 26—and in some cases up to 45. The vaccine doesn’t eliminate the need for Pap smears, since it doesn’t cover every cancer-causing strain, but it dramatically reduces the risk.
Together, the Pap smear and the HPV vaccine form a dynamic duo. One prevents infection; the other detects any resulting cellular changes. When used together, they create a robust defense against cervical cancer, making it increasingly rare in younger generations.
When Results Come Back Abnormal: What Happens Next?
Hearing that your Pap smear is abnormal can be frightening, but it’s important to understand that “abnormal” doesn’t mean cancer. It means that some cells don’t look quite right and need further evaluation. Most of the time, these abnormalities resolve on their own or can be treated easily.
Depending on the type and severity of the abnormality, your provider may recommend another Pap smear in six to twelve months, an HPV test, or a colposcopy. If a biopsy confirms the presence of precancerous cells, treatments such as cryotherapy, laser therapy, or a procedure known as LEEP (loop electrosurgical excision procedure) can remove the problematic tissue before it becomes cancerous.
Early detection keeps treatment options simple and success rates high. That’s the magic of screening—it shifts outcomes dramatically in your favor.
A Lifelong Partnership with Your Health
At its heart, the Pap smear represents more than just a test. It symbolizes a woman’s partnership with her own body. It’s a regular check-in, a preventive ritual, and a courageous act of self-care. While it may not be the most glamorous part of a health routine, it is unquestionably one of the most impactful.
Creating a healthy relationship with the Pap smear means viewing it not as a dreaded obligation, but as a proactive, empowering moment. It’s a reminder that your health matters, that you deserve answers, and that you have the tools to protect yourself.
Conclusion: The Small Test That Saves Lives
In a world filled with complex health challenges, the Pap smear stands out for its simplicity, affordability, and effectiveness. It doesn’t require fancy equipment or futuristic medicine—just awareness, access, and a few minutes of courage.
Every time a woman walks into a clinic for her Pap smear, she’s doing something profoundly powerful. She’s saying yes to prevention. Yes to peace of mind. Yes to the knowledge that her life is worth protecting.
If you’re due for a Pap smear—or if you’ve never had one—consider this your sign. Make the appointment. Ask the questions. Take the step. Because when it comes to cervical health, a little swab can go a very long way.