Every night, millions of people drift into what should be a peaceful sleep—but for some, that rest becomes a silent battle. Obstructive sleep apnea, a disorder marked by repeated pauses in breathing during sleep, can quietly strain the heart, disrupt oxygen flow to the brain, and leave the body exhausted. But new research from Korea University Ansan Hospital has revealed something even more concerning: moderate to severe obstructive sleep apnea may increase the risk of developing cerebral microbleeds—tiny, often invisible signs of brain damage that can foreshadow stroke or dementia.
Understanding the Invisible Scars of the Brain
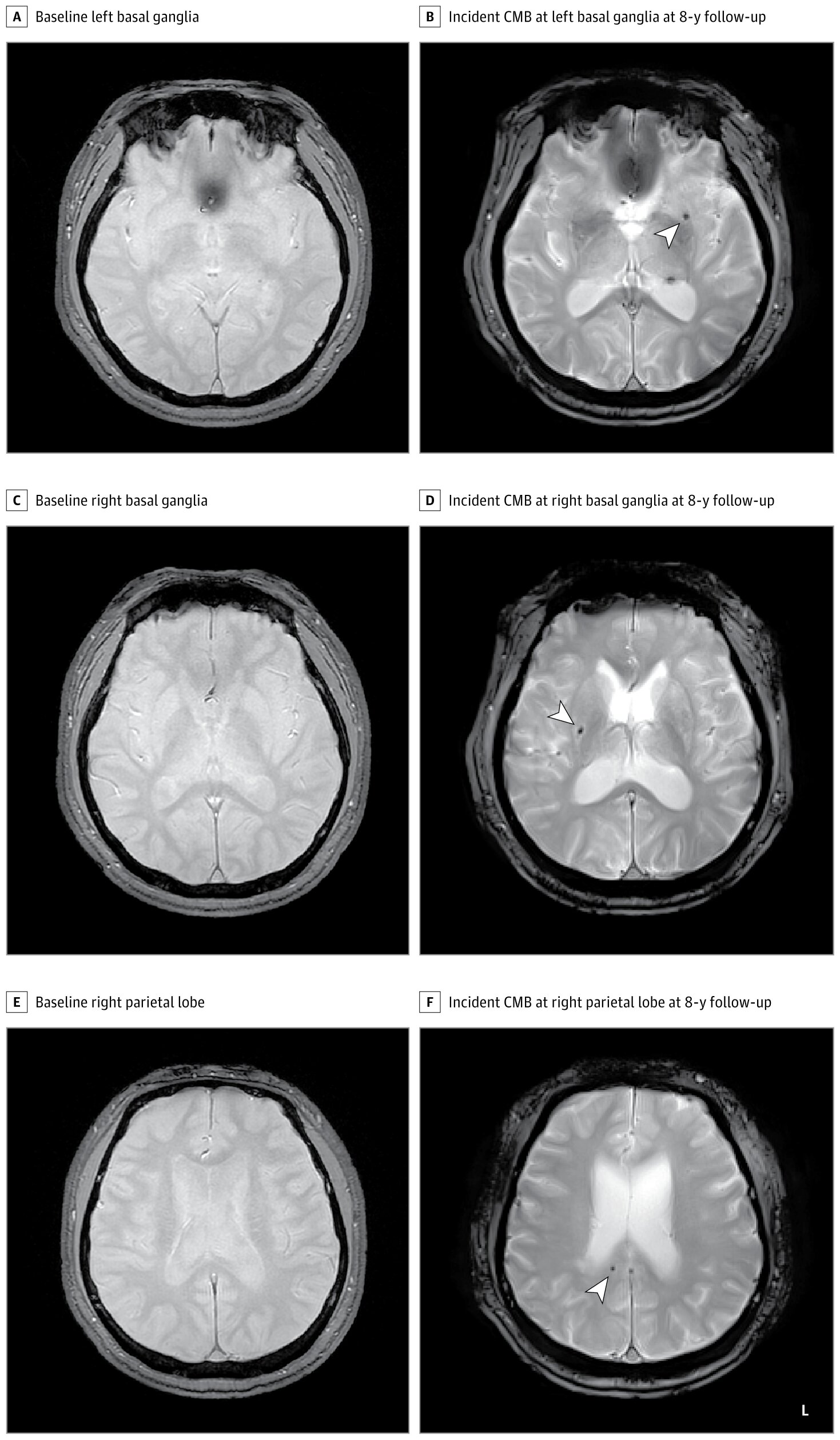
Cerebral microbleeds are minute spots of bleeding, often too small to cause immediate symptoms but large enough to be detected on high-resolution MRI scans. They appear as dark pinpoints—silent witnesses of vascular injury deep within the brain. For years, neurologists have recognized them as early markers of cerebrovascular fragility, linked to cognitive decline, stroke, and even Alzheimer’s disease.
In middle-aged adults, only about 3% show these microbleeds, but in older populations, that number can reach nearly a quarter. Each one represents a rupture in the brain’s delicate network of vessels—a warning sign that the body’s vital organ is under strain.
Why Sleep Apnea Matters
Sleep apnea may seem harmless at first—just snoring, interrupted breathing, or daytime fatigue. But the condition’s physiological effects run deep. When breathing stops repeatedly during sleep, oxygen levels in the blood plummet. The brain, deprived of oxygen, sends stress signals through the body, causing surges in blood pressure and inflammation. Over time, this nightly assault damages blood vessels, including those in the brain.
Previous research hinted at a possible connection between sleep apnea and microbleeds, but the evidence was inconsistent. Some studies showed a link, while others did not. The new study, published in JAMA Network Open, set out to resolve this uncertainty through a large-scale, long-term investigation.
A Study That Watches Sleep and the Brain
The researchers followed 1,441 adults from a Korean community, all free of microbleeds or cardiovascular disease at the start. Each participant underwent in-home polysomnography—a comprehensive sleep test that tracks breathing, oxygen levels, and brain activity—alongside brain MRI scans. Over the following eight years, they were monitored for the development of new cerebral microbleeds.
Participants were grouped based on their apnea-hypopnea index, a measure of breathing interruptions per hour:
- No sleep apnea (0–4.9 events/hour)
- Mild sleep apnea (5.0–14.9 events/hour)
- Moderate to severe sleep apnea (15 or more events/hour)
The distinction mattered. What the researchers found next was striking.
When Breathing Pauses, the Brain Suffers
At the four-year follow-up, microbleeds had developed in 1.85% of those without sleep apnea, 1.61% with mild apnea, and 4.66% with moderate to severe apnea. By eight years, those numbers grew to 3.33%, 3.21%, and a concerning 7.25%, respectively.
In simple terms, people with moderate to severe sleep apnea were more than twice as likely to develop cerebral microbleeds compared with those without the condition. Even after adjusting for known risk factors—such as smoking, high blood pressure, diabetes, and cholesterol—the association persisted.
The results paint a clear picture: the more severe the sleep apnea, the greater the likelihood of developing these early markers of brain injury.
The Genetic Puzzle: Is It in Our DNA?
The research team also wanted to know whether genetics could explain the link. They looked at a genetic variation called APOE-ε4, a known risk factor for Alzheimer’s disease and cerebrovascular problems.
Among the 1,233 participants with genetic data, roughly 19% carried the APOE-ε4 gene. When the researchers adjusted for this factor, the association between sleep apnea and microbleeds grew even stronger—rising from a relative risk of 2.14 to 2.91.
This finding suggests that while genetics may amplify vulnerability, the connection between sleep apnea and brain microbleeds cannot be explained by genes alone. Instead, it points to the direct impact of disrupted breathing and oxygen deprivation on the brain’s blood vessels.
A Window Into Brain Health
Cerebral microbleeds are not just abstract data points—they are early signs that the brain is being quietly injured. They often precede more serious events like stroke, cognitive decline, or dementia. Identifying and addressing their causes early could have enormous implications for public health.
The fact that sleep apnea—a common and treatable condition—appears to increase the risk of these microbleeds offers a powerful opportunity for prevention. Continuous positive airway pressure (CPAP) therapy, weight management, and lifestyle changes have all been shown to reduce the effects of sleep apnea. With early detection and intervention, it may be possible to protect the brain before irreversible damage occurs.
Why This Matters for an Aging World
As populations age, dementia and stroke have become some of the most feared and costly diseases worldwide. The brain’s blood vessels are central to both. If sleep apnea is indeed a modifiable risk factor for microbleeds, treating it could help delay or even prevent the cascade of cognitive and vascular decline that follows.
In many cases, sleep apnea goes undiagnosed—especially in older adults who attribute poor sleep or fatigue to aging. Yet simple sleep studies can reveal the condition, and treatment can transform not only sleep quality but long-term brain health.
The Night as a Mirror of the Mind
There is something profoundly poetic about this discovery. Sleep, which should restore the body, can become a time of harm if the rhythm of breath falters. The pauses we never notice—the silent moments when the body struggles for air—can leave marks that only an MRI can see. These microbleeds are whispers from the brain, telling us that something as basic as breathing is deeply intertwined with the health of our thoughts, our memories, and our future selves.
Looking Forward
The findings from Korea University Ansan Hospital are not just an academic insight; they are a call to awareness. Sleep apnea is more than snoring—it is a systemic disorder with consequences that ripple through the body and the brain. As researchers continue to explore the mechanisms linking apnea, blood flow, and neural integrity, one truth becomes increasingly clear: the quality of our sleep shapes the architecture of our minds.
By recognizing and treating sleep apnea early, we might not only prevent fatigue or heart strain—but also preserve the fragile networks that make us who we are. In protecting our sleep, we may very well protect our ability to think, remember, and dream.
More information: Ali Tanweer Siddiquee et al, Obstructive Sleep Apnea and Cerebral Microbleeds in Middle-Aged and Older Adults, JAMA Network Open (2025). DOI: 10.1001/jamanetworkopen.2025.39874