Imagine waking up one day to find your body turning against you—not by accident, injury, or external force, but through its own defenses. The immune system, once your protector, now sees you as the enemy. Cells meant to destroy viruses and bacteria begin targeting your tissues, your organs, your life.
This is not the plot of a sci-fi thriller—it’s the reality faced by millions of people around the world who live with autoimmune diseases.
Autoimmune conditions are some of the most complex, misunderstood, and intriguing disorders in all of medicine. They are not caused by outside invaders like infections, nor are they genetic disorders in the traditional sense. Instead, they arise from a miscommunication within the very system designed to keep us healthy.
In this article, we’ll explore the science behind autoimmune diseases, their bewildering diversity, how they affect the body, what it’s like to live with one, and the path researchers are taking to better understand, treat, and perhaps even cure these chronic conditions.
The Immune System: Defender of the Realm
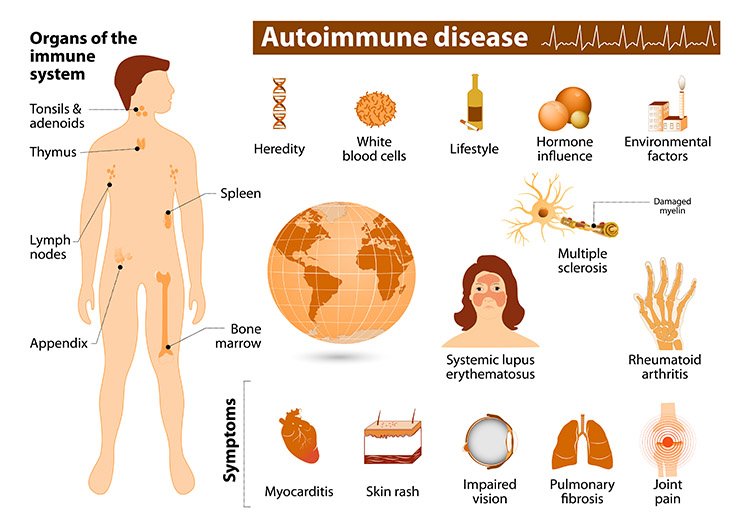
To understand autoimmune disease, we must first grasp how the immune system works. It is one of the most sophisticated defense mechanisms nature has ever evolved—a vast network of cells, tissues, and molecules spread throughout the body, designed to detect and eliminate harmful invaders.
At its core, the immune system has one primary mission: distinguish self from non-self.
When a foreign pathogen—like a virus, bacteria, or fungus—enters the body, immune cells recognize its unique molecular signature and mount a response. White blood cells, antibodies, and specialized T-cells all leap into action, neutralizing the threat with astonishing precision.
In a healthy system, this process includes a system of checks and balances. Immune cells are trained during development not to react against the body’s own tissues. If a cell does show signs of self-reactivity, it’s usually destroyed before it can cause harm.
But sometimes, something goes wrong. A few rogue cells escape the checkpoints. They multiply, recruit others, and begin attacking the very tissues they’re supposed to protect. When this happens, we have an autoimmune response.
The Rogue’s Gallery: A Diversity of Disorders
There are over 80 known autoimmune diseases, and they can affect virtually every organ system in the body. Some target specific organs; others cause widespread, systemic havoc.
Type 1 diabetes, for instance, occurs when the immune system attacks insulin-producing beta cells in the pancreas. Rheumatoid arthritis targets the joints. Multiple sclerosis damages the protective sheaths around nerve fibers in the central nervous system. Lupus can affect the skin, joints, kidneys, heart, and even the brain.
Despite their differences, all autoimmune diseases share one common feature: a breakdown in immune tolerance, where the body fails to recognize part of itself as “self.”
Let’s take a closer look at a few of the more well-known autoimmune disorders to understand their symptoms, mechanisms, and impact.
Type 1 Diabetes: A Silent Siege on the Pancreas
Type 1 diabetes (T1D) is often diagnosed in children or young adults, but it can occur at any age. It arises when the immune system mistakenly identifies insulin-producing beta cells in the pancreas as foreign and systematically destroys them.
Without insulin—a hormone critical for regulating blood sugar—glucose builds up in the bloodstream, leading to a range of acute and chronic health problems. T1D must be managed with daily insulin injections or pumps, and even with careful monitoring, it can lead to complications like neuropathy, kidney damage, and heart disease.
The exact trigger for T1D is still unknown. It may involve a combination of genetic susceptibility and environmental factors—such as viral infections—that tip the immune system into overdrive.
Rheumatoid Arthritis: The Fire in the Joints
Unlike osteoarthritis, which is caused by wear and tear on the joints, rheumatoid arthritis (RA) is an autoimmune disease where the immune system attacks the synovium—the lining of the membranes that surround the joints.
This leads to painful swelling, stiffness, and eventual joint deformity. Over time, the inflammation can spread to other parts of the body, including the heart, lungs, and blood vessels.
RA disproportionately affects women, and while it often begins between ages 30 and 60, it can strike earlier or later. Treatments include immunosuppressive drugs, anti-inflammatory medications, and physical therapy to manage pain and preserve mobility.
Systemic Lupus Erythematosus: The Great Mimic
Often called “the great imitator,” lupus can manifest in so many ways that it’s notoriously difficult to diagnose. Its symptoms—ranging from fatigue and fever to joint pain, rashes, and organ damage—can mimic dozens of other conditions.
Lupus is caused by the production of autoantibodies that attack cells and tissues throughout the body. These antibodies can form immune complexes that deposit in the skin, kidneys, brain, and blood vessels, leading to chronic inflammation and damage.
It’s most common in women of childbearing age and is more prevalent among people of African, Hispanic, and Asian descent. Lupus flare-ups can be triggered by stress, sunlight, infections, and even certain medications.
Multiple Sclerosis: When Nerves Go Numb
Multiple sclerosis (MS) is a neurodegenerative autoimmune disease where the immune system attacks the myelin sheath—the protective coating around nerve fibers in the central nervous system.
As the myelin degrades, nerve signals slow down or stop altogether, leading to symptoms like vision problems, muscle weakness, balance issues, and cognitive decline.
MS often progresses in unpredictable cycles of relapse and remission. Some patients experience a slow, steady worsening of symptoms, while others have long periods of stability punctuated by sudden flares.
There is no cure, but treatments aim to reduce inflammation, manage symptoms, and slow the progression of disability.
What Causes Autoimmune Disease?
This is one of the great mysteries of modern medicine. Why does the immune system go haywire in some people but not others?
Scientists believe that genetics play a role. Certain genes related to the human leukocyte antigen (HLA) complex appear to increase the risk of autoimmune disorders. However, genes alone aren’t the full story. Identical twins often show different autoimmune outcomes, which points to environmental triggers.
Infections are strong suspects. In some cases, a virus or bacteria may mimic a protein in the body, causing the immune system to attack both. This phenomenon is known as molecular mimicry.
Hormones also seem to be involved—many autoimmune diseases are more common in women, particularly during reproductive years, suggesting a link to estrogen and other hormonal cycles.
Other contributing factors include:
- Stress: Chronic emotional or physical stress may alter immune regulation.
- Diet: Western diets high in processed foods and low in fiber may impact gut health and immune function.
- Environmental toxins: Exposure to chemicals like silica, heavy metals, or solvents has been linked to increased autoimmune risk.
- Microbiome imbalances: Disruptions in gut flora may play a role in autoimmune dysregulation.
The interplay of these factors is complex and still under intense investigation.
Living with an Autoimmune Disease: The Daily Reality
For those living with autoimmune disorders, the experience is often a rollercoaster—unpredictable flares, invisible symptoms, side effects from medications, and the social challenge of explaining an illness that often doesn’t “look” like anything from the outside.
Fatigue is one of the most common and debilitating symptoms across nearly all autoimmune diseases. It’s not the kind of tiredness that sleep can fix—it’s a bone-deep exhaustion that can disrupt every part of daily life.
Pain is another common theme, whether in the joints, muscles, or affected organs. Mental health challenges like depression and anxiety are also more prevalent among autoimmune patients, partly due to chronic illness and partly due to physiological effects of inflammation on the brain.
Patients often become experts in their own bodies, learning to anticipate flares, track triggers, and manage complex medication regimens.
And yet, despite all this, many people with autoimmune diseases lead full, vibrant lives—working, raising families, creating art, and advocating for others.
Diagnosis: A Long and Winding Road
Diagnosing autoimmune disease is rarely straightforward. Symptoms can be vague, intermittent, and easily confused with other conditions. It often takes years for patients to receive a correct diagnosis, during which time the disease may continue to cause damage.
Doctors rely on a combination of:
- Medical history and physical exam
- Blood tests to detect autoantibodies
- Imaging to visualize inflammation or damage
- Biopsy in some cases (especially with skin or kidney involvement)
Still, no single test can confirm all autoimmune diseases. The process often involves ruling out other causes and gradually building a clinical picture that points toward an autoimmune origin.
Treatment: Taming the Immune Beast
There is no cure for most autoimmune diseases, but many can be managed effectively with the right treatment plan. The goal is to reduce inflammation, control symptoms, prevent organ damage, and improve quality of life.
Common treatment approaches include:
- Corticosteroids to rapidly reduce inflammation during flares
- Immunosuppressants like methotrexate or azathioprine
- Biologic agents such as TNF inhibitors (e.g., Humira, Enbrel) or B-cell depleting therapies (e.g., Rituxan)
- Targeted therapies designed to block specific immune pathways
- Supportive care, including pain management, physical therapy, and mental health support
Patients must balance the benefits of immune suppression with the risks—such as increased susceptibility to infections, side effects, and long-term complications.
Lifestyle also plays a vital role. Regular exercise, a balanced anti-inflammatory diet, stress reduction, and good sleep hygiene can all help reduce symptom severity and improve resilience.
Research Frontiers: Toward a Cure?
Autoimmune disease research is one of the fastest-moving areas in medicine today. Scientists are exploring novel therapies that go beyond broad immune suppression toward immune modulation—training the body to recognize “self” again.
Exciting areas of research include:
- Tolerance induction therapy, which seeks to retrain the immune system to ignore specific tissues
- Gene editing, such as CRISPR, to correct faulty immune programming
- Microbiome manipulation to restore gut-immune balance
- Peptide therapies that block autoantigen presentation
- Personalized medicine using genetic and biomarker profiling
There is also growing interest in preventing autoimmune diseases before they start. By identifying high-risk individuals and intervening early—perhaps with vaccines or dietary changes—scientists hope to stop autoimmunity before it takes hold.
Conclusion: A Battle Fought from Within
Autoimmune diseases are paradoxes. They reveal the immense power of the immune system—but also its capacity for error. They are invisible battles fought within, where the lines between friend and foe blur, and where the body becomes its own worst enemy.
And yet, amid the pain and complexity, there is resilience. Millions of people navigate these challenges every day with courage, creativity, and strength. Their stories are a testament to the human spirit—and to the urgency of medical science to understand what goes wrong, and how to make it right.
The future holds promise. With each discovery, we move closer to unraveling the mystery of autoimmunity and bringing healing not just to the body, but to the mind and the life that it carries.
Because when the body attacks itself, it’s not just biology—it’s a profound, personal struggle. And one worth understanding.