If you’ve ever enjoyed a peanut butter sandwich or a bowl of strawberries without incident, you can thank an unsung hero in your body: a highly selective, highly intelligent immune system. While allergic reactions to food are often front-page news—sometimes tragically so—what’s far less appreciated is how often your immune system does not overreact. In fact, for most people, most of the time, the immune system allows the continual introduction of foreign proteins into the gut—proteins that it could just as easily misidentify as a threat—with quiet grace.
This remarkable restraint is no accident. It’s the result of an essential immunological phenomenon called oral tolerance—the immune system’s active decision to not attack the foods we eat. Long considered a kind of immunological black box, this tolerance has eluded full mechanistic understanding for decades. But now, a groundbreaking study published in Nature by Dr. Ranit Kedmi and colleagues at Israel’s Weizmann Institute of Science has cracked open that box. Their findings reveal a surprisingly intricate cellular network that determines whether the immune system treats food as friend or foe.
The Prenatal Beginnings of Tolerance
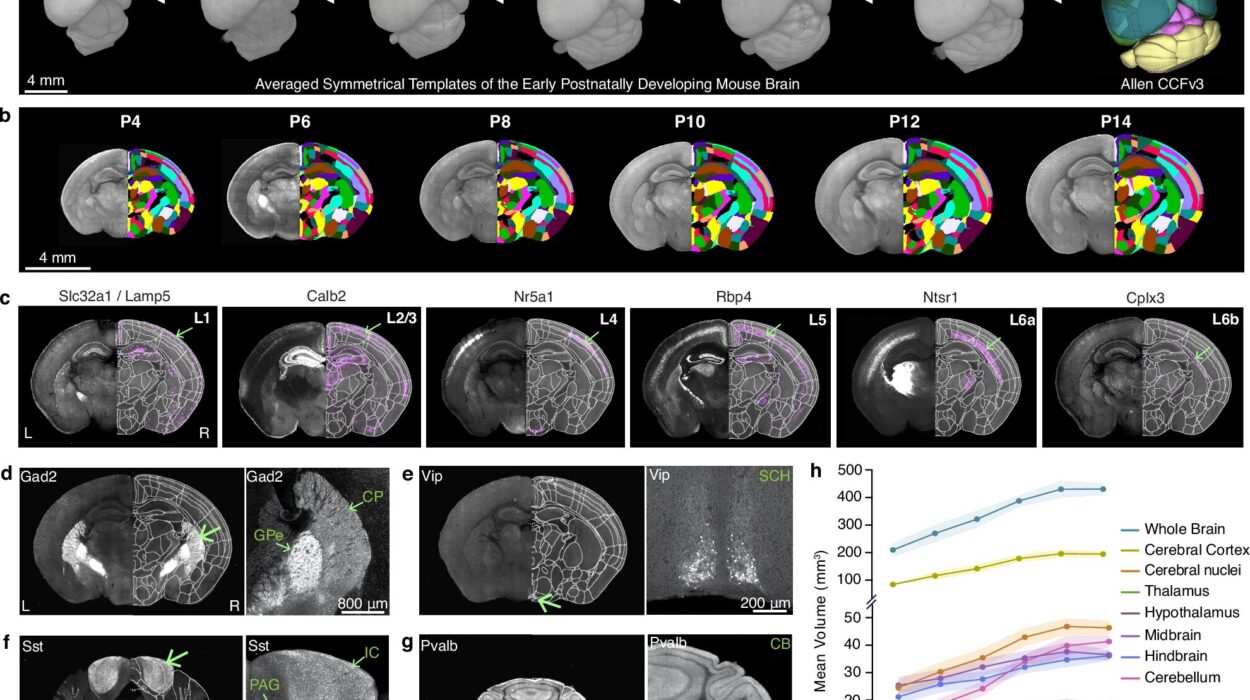
Oral tolerance isn’t something that suddenly switches on the day a baby eats mashed peas for the first time. It begins far earlier—in utero. During pregnancy, a fetus is already exposed to molecular traces of the food the mother consumes. This early exposure subtly introduces the fetal immune system to foreign dietary antigens, laying the groundwork for future tolerance. It’s a sort of immunological preview, a quiet whisper that says: “This is safe.”
That process accelerates during breastfeeding, when even more dietary molecules are passed from mother to child. And as a child grows and begins consuming a variety of foods, the immune system continues this education. But the lessons don’t come from food alone—they’re heavily influenced by another classroom: the gut microbiome. These vast bacterial communities produce a range of metabolites and proteins that themselves could be mistaken for harmful invaders. Instead, a well-tuned immune system learns to recognize both food and friendly bacteria as harmless, weaving a peaceful coexistence that is foundational to gut health.
The Mystery of the Missing Dendritic Cell
For many years, immunologists believed that this learning process was orchestrated by a class of immune cells called dendritic cells—the same cells that marshal forces during infections. When pathogens invade, dendritic cells digest them and display their protein fragments to other immune cells, waving a red flag that screams, “Attack!”
So, it was logical to assume they played the same gatekeeping role with food—choosing, in this case, to wave a white flag and instruct tolerance instead. But an odd problem persisted: when researchers genetically eliminated the key subset of dendritic cells believed to be responsible, oral tolerance still emerged in lab mice. Somehow, the immune system was preserving the peace without its usual diplomats.
This paradox puzzled researchers. If dendritic cells weren’t essential for oral tolerance, then who was?
ROR-γt: The Unexpected Peacekeeper
Dr. Ranit Kedmi, during her postdoctoral work, had taken interest in an unusual, elusive population of immune cells called ROR-γt+ cells—named after the gene that regulates their development. These cells, which don’t fit neatly into any one immune category, seemed to be lurking in the gut’s complex cellular architecture. She wondered: Could these mysterious cells be quietly shaping the body’s decision to tolerate food?
Her team set out to test this hypothesis using genetically modified mice. In these animals, the ROR-γt cells were still present—but stripped of their ability to present food-derived antigens to the rest of the immune system. The results were dramatic: the mice rapidly developed food allergies. The absence of ROR-γt cell signaling triggered a cascade of immune responses, leading to inflammation and food rejection.
It was a stunning reversal of the prevailing model. Rather than dendritic cells being the core peacekeepers, Kedmi’s study found that specialized ROR-γt cells were the ones initiating tolerance. This reshuffled the immunological narrative—and opened new investigative frontiers.
A Four-Cell Symphony of Suppression
Kedmi’s team didn’t stop there. Determined to unravel the full circuit of oral tolerance, lead researcher Anna Rudnitsky and colleagues deployed a suite of advanced genetic and imaging tools to watch the immune system in action.
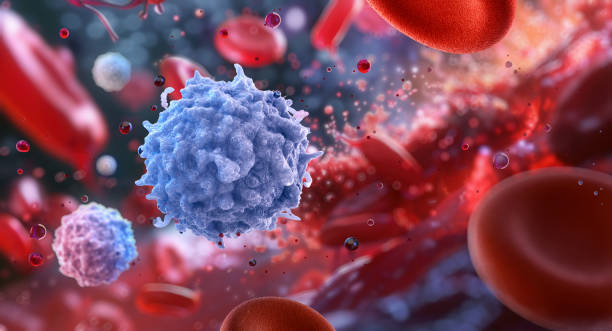
What they discovered was a complex, coordinated network involving four distinct cell types. This cellular relay began with the ROR-γt cells, which processed and presented food particles. From there, the signal passed to a second and third group of intermediary immune cells—each modulating the message and forwarding it along the line. Finally, the chain reached a familiar group of immune warriors: CD8+ T cells, the body’s enforcers.
Under normal circumstances, CD8 cells are responsible for hunting down virus-infected or cancerous cells and executing them with deadly precision. But in the context of oral tolerance, the message delivered by the ROR-γt-initiated cascade was clear: stand down. The CD8s were suppressed, their inflammation-inducing instincts put on pause.
This suppression of CD8 cells at the final step was the immune system’s version of a peace treaty. It ensured that ingested proteins, no matter how foreign, were greeted with tolerance rather than aggression.
What Happens When Peace Is Broken?
Yet this elegant immune détente poses a dilemma. If CD8 cells are silenced by food-related signals, what happens if a dangerous microbe enters the body disguised with similar proteins? Could pathogens exploit oral tolerance to sneak past immune defenses?
To test this, Kedmi’s group engineered a clever experiment. They introduced a harmless food protein into the mouse gut, conditioning the immune system to tolerate it. Then, they infected the same mice with a microbe engineered to express that same protein. What happened next was astonishing.
The immune system recognized the microbial threat and temporarily lifted the suppression. The CD8 cells launched a full assault, eliminating the invader. Once the infection cleared, the tolerance network was restored, and the CD8s once again became passive in the face of the dietary protein.
This indicated that oral tolerance isn’t a static peace—it’s dynamic. It can be dialed up or down depending on circumstances, constantly weighing whether foreign proteins are benign or dangerous.
Kedmi likens this to diplomatic relations between neighboring countries. “Two nations may have a peace accord,” she explains, “but if one fires across the border, the other will respond with force—peace treaty or not. The immune system is just as nuanced. It prioritizes defense when needed, but is always ready to return to peace.”
Allergy and Autoimmunity: When Tolerance Goes Awry
The implications of these findings are enormous. Food allergies, celiac disease, and inflammatory bowel conditions all appear to involve breakdowns in oral tolerance. For instance, in celiac disease, the immune system treats gluten—a harmless protein—as a mortal enemy, leading to CD8-mediated destruction of the gut lining.
By identifying the specific cellular actors and checkpoints in the tolerance network, researchers can now start pinpointing exactly where things go wrong. Is it a failure of the ROR-γt cells to initiate the tolerance cascade? A disruption in the intermediary signaling? Or is it the final suppression of CD8 cells that fails?
Answering these questions may lead to a new era in treating immune-mediated food disorders—not just by blocking symptoms but by restoring tolerance itself.
A New Chapter in Immunology
The story of oral tolerance is still unfolding, but the work of Kedmi and her team has added a bold new chapter. They have transformed an elusive concept into a tangible, testable cellular model. In doing so, they’ve redefined how we understand immune balance in the gut—and perhaps in other mucosal tissues as well.
Their study is a testament to how far immunology has come since the early days of blanket “attack-or-ignore” models. The immune system is not a simple switchboard—it is a symphony, with players who harmonize, pause, and crescendo with precision.
Thanks to this research, we are closer than ever to understanding why our immune systems let us feast in peace—and what happens when that peace is shattered. It’s a powerful reminder that health is not the absence of conflict, but the presence of intelligent restraint.
Reference: Anna Rudnitsky et al, A coordinated cellular network regulates tolerance to food, Nature (2025). DOI: 10.1038/s41586-025-09173-x