There is a universe within each of us—a vast, invisible ecosystem so complex, dynamic, and essential that our lives would be impossible without it. This universe is the microbiome: the collection of trillions of bacteria, viruses, fungi, and other microbes that live in and on the human body. Most of these microscopic residents live in our gut, nestled within the folds of the intestines, forming intricate colonies that interact intimately with our health.
What was once seen as a nuisance or a threat—bacteria in the body—is now understood to be a vital organ in its own right. The microbiome is not just a passive passenger. It plays an active, commanding role in digestion, metabolism, brain function, and especially immune regulation. It trains, calibrates, and balances the immune system, acting both as a sentinel and a diplomat—alerting the body to danger, but also reminding it when not to overreact.
In recent decades, the study of the microbiome has reshaped our understanding of health and disease. Scientists now know that disruptions in the microbial balance—what is called dysbiosis—can contribute to autoimmune conditions, allergies, inflammatory bowel diseases, obesity, even cancer and depression. But the most captivating story, and perhaps the most consequential, is how this hidden world orchestrates the symphony of our immune defenses.
The Early Dialogue: Birth and the Microbial Gift
The relationship between the microbiome and the immune system begins before we take our first breath. For decades, it was believed that babies were sterile in the womb and colonized only during birth. New research suggests that small numbers of microbes may be present even in the placenta and amniotic fluid, priming the immune system before birth. But it is the moment of delivery that truly marks the microbial debut.
Babies born vaginally are coated in their mother’s microbiota—primarily Lactobacillus species from the birth canal. This early inoculation seeds the infant’s gut and shapes the initial microbial landscape. In contrast, babies born via cesarean section are colonized by skin bacteria, which may lead to altered immune responses. Studies show that C-section births are associated with higher rates of asthma, allergies, and autoimmune diseases—an echo of this microbial difference.
Breast milk is the next microbial treasure. It is not sterile, but teeming with beneficial bacteria and specialized sugars called human milk oligosaccharides (HMOs). These HMOs are indigestible to infants but serve as food for beneficial gut bacteria like Bifidobacterium infantis. This elegant design nurtures a healthy gut flora and educates the developing immune system, steering it away from overreacting to harmless stimuli.
During the first year of life, the infant microbiome undergoes dramatic changes. By age three, it stabilizes into an adult-like community. But this early window is critical. Disruptions due to antibiotics, formula feeding, or hygiene can have long-lasting effects, potentially tilting the immune system toward chronic inflammation or allergic hypersensitivity.
A Delicate Balance: Immune Tolerance and Microbial Training
Our immune system is a paradox. It must be aggressive enough to eliminate threats, yet restrained enough not to attack our own tissues or harmless substances like pollen or food proteins. This balance is known as immune tolerance—and the microbiome is its teacher.
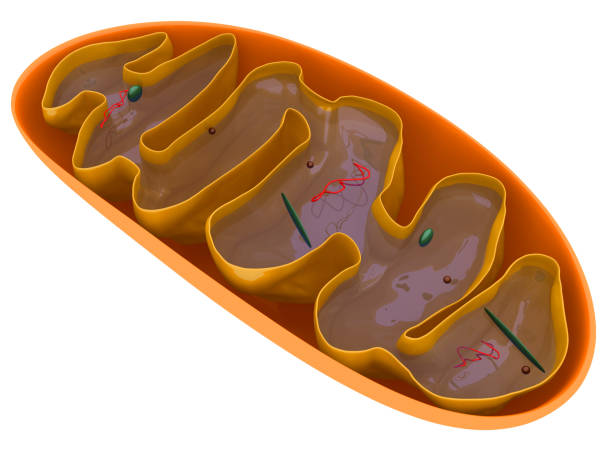
In the gut, immune cells are constantly sampling the microbial environment. Specialized cells extend dendrites through the intestinal lining to “taste” what’s inside the lumen. Microbial metabolites, especially short-chain fatty acids (SCFAs) like butyrate and acetate, signal to the immune system to calm down and tolerate the presence of friendly microbes.
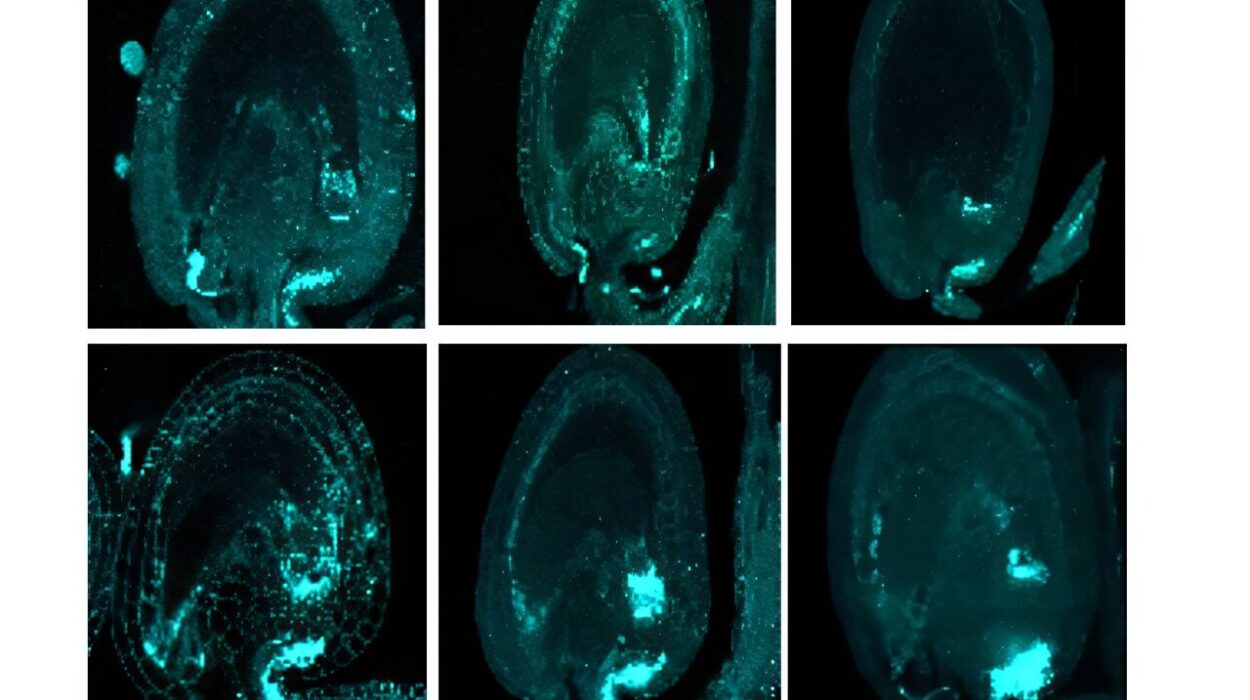
One of the most important immune cell types influenced by the microbiome is the regulatory T cell (Treg). These cells act like immune peacekeepers. They prevent autoimmune reactions and control inflammatory responses. Studies show that germ-free mice, raised in sterile environments without any microbes, have underdeveloped immune systems and fewer Tregs. When these mice are colonized with healthy microbes, their immune systems mature, and tolerance is restored.
This microbial education is not passive. Certain bacteria have been shown to actively promote the development of Tregs. For example, Clostridia species in the colon induce the production of interleukin-10 (IL-10), an anti-inflammatory cytokine essential for maintaining immune balance. Without these signals, the immune system becomes prone to overreaction, leading to allergies, asthma, and autoimmune diseases.
Gut-Associated Lymphoid Tissue: The Immune Brain of the Intestines
The gut is not just a digestive organ—it is the largest immune organ in the body. Over 70% of the body’s immune cells reside in the gastrointestinal tract, particularly in structures known as gut-associated lymphoid tissue (GALT). These include Peyer’s patches, isolated lymphoid follicles, and mesenteric lymph nodes.
The GALT serves as an interface between the microbial world and the immune system. It’s a zone of constant surveillance and communication. Dendritic cells present antigens from microbes to naïve T cells, deciding whether to mount an immune response or induce tolerance. This decision is influenced by microbial signals, dietary components, and the integrity of the intestinal barrier.
When the barrier breaks down—a phenomenon known as “leaky gut”—microbes and their components can cross into the bloodstream, triggering systemic inflammation. This has been implicated in numerous chronic diseases, from rheumatoid arthritis to type 1 diabetes.
Maintaining barrier integrity is another task the microbiome excels at. Commensal bacteria stimulate the production of mucus and tight junction proteins that seal the spaces between epithelial cells. SCFAs also nourish colonocytes, the cells that line the colon, promoting a healthy, impermeable lining.
Microbiome-Driven Immune Disorders: When Peace Turns to War
When the microbiome is in balance, the immune system remains calm and vigilant. But when the microbial composition becomes skewed, the results can be devastating.
One striking example is inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis. In these conditions, the gut immune system launches a chronic attack on the intestinal lining, driven in part by dysbiosis. Patients with IBD often have reduced microbial diversity, lower levels of beneficial Faecalibacterium prausnitzii, and higher levels of pro-inflammatory bacteria like Escherichia coli.
In autoimmune diseases like multiple sclerosis (MS) and type 1 diabetes, altered gut microbiota have been observed. Germ-free mice are resistant to developing these diseases, while transferring gut microbes from affected animals or humans can induce symptoms. These findings suggest that the microbiome doesn’t just modulate local gut immunity—it influences systemic immunity and even brain inflammation.
Allergic diseases also show microbial fingerprints. Children growing up on farms or exposed to diverse microbes in early life are less likely to develop asthma and eczema—a phenomenon known as the hygiene hypothesis. The idea is that too little microbial exposure in childhood leads to an undertrained immune system, which overreacts to harmless allergens.
Microbes as Immunotherapists: The Promise of Probiotics and Fecal Transplants
With the growing recognition that microbes regulate immunity, scientists are exploring ways to harness this power therapeutically. Probiotics—live microorganisms that confer health benefits—are one approach. Some strains of Lactobacillus and Bifidobacterium have shown promise in reducing inflammation, improving eczema, and even enhancing the effectiveness of vaccines. However, results are mixed, and much depends on the specific strain, dose, and the individual’s existing microbiome.
A more radical therapy is fecal microbiota transplantation (FMT), where stool from a healthy donor is transferred to a patient to restore microbial balance. FMT has shown dramatic success in treating recurrent Clostridioides difficile infections, which often occur after antibiotic use. In some cases, FMT restores immune balance and resolves symptoms in days.
Researchers are now investigating FMT for autoimmune diseases, depression, metabolic disorders, and even autism. Early results are promising but require cautious interpretation. The microbiome is a delicate ecosystem, and manipulating it requires precision and care. The future may lie in “designer probiotics”—engineered microbes that deliver targeted immune signals or therapeutic molecules.
Diet, Microbes, and Immunity: Feeding the Inner Garden
What we eat profoundly shapes our microbiome and, by extension, our immune system. Diets high in fiber, fermented foods, and polyphenols foster microbial diversity and support the growth of beneficial bacteria. These bacteria, in turn, produce SCFAs and other metabolites that reduce inflammation, promote Treg development, and strengthen the gut barrier.
Conversely, the modern Western diet—rich in processed foods, sugar, and animal fat—disrupts the microbiome. It favors the growth of pro-inflammatory species, reduces microbial diversity, and increases intestinal permeability. Animal studies have shown that high-fat diets can induce low-grade systemic inflammation through microbiome changes alone.
Moreover, specific foods act as prebiotics—fuel for good microbes. These include garlic, onions, leeks, bananas, and oats. Fermented foods like yogurt, kefir, kimchi, and sauerkraut provide live bacteria and beneficial enzymes that support gut health.
Nutritional interventions that target the microbiome offer a powerful, non-invasive way to modulate immunity. They may prevent disease, improve vaccine responses, and reduce the need for immunosuppressive drugs. In the future, your personalized diet may be as much about feeding your microbes as it is about feeding yourself.
The Microbiome Beyond the Gut: Skin, Lungs, and the Brain
While the gut microbiome has received the most attention, other body sites also harbor microbial communities with immune-regulating roles. The skin microbiome, for example, helps maintain the skin’s acid mantle, prevents colonization by pathogens, and educates local immune cells. Disruptions in the skin microbiome are linked to eczema, psoriasis, and acne.
The respiratory tract also hosts its own microbiome. Emerging evidence suggests that lung microbes influence susceptibility to asthma, chronic obstructive pulmonary disease (COPD), and viral infections. The gut-lung axis—a bidirectional communication between gut microbes and lung immunity—is now a major focus of research.
Perhaps most surprisingly, the microbiome influences the brain and behavior through the gut-brain axis. Microbes produce neurotransmitters, modulate stress hormones, and affect blood-brain barrier integrity. They even shape microglia—the brain’s immune cells. Dysbiosis has been implicated in anxiety, depression, autism, and neurodegeneration. As researchers dig deeper, the connection between microbes, immunity, and the mind becomes increasingly clear.
Antibiotics and Modern Medicine: A Double-Edged Sword
The discovery of antibiotics revolutionized medicine, saving countless lives. But their widespread, often indiscriminate use has unintended consequences. Antibiotics not only kill harmful bacteria—they also decimate beneficial microbiota, sometimes permanently altering microbial ecosystems.
Repeated antibiotic exposure, especially in early life, is associated with increased risk of asthma, obesity, and autoimmune diseases. This suggests that antibiotics, by disrupting microbial-immune crosstalk during critical windows, can reprogram immunity in harmful ways.
Moreover, the rise of antibiotic resistance threatens to make even minor infections deadly once again. Preserving microbial diversity and restoring microbial balance after antibiotic use is now a priority in medical practice. This includes probiotic use, microbiome monitoring, and limiting antibiotic prescriptions to necessary cases.
Toward a Microbial Renaissance in Medicine
The microbiome is ushering in a new era of medicine—one that sees health not just as a battle against pathogens, but as a dynamic balance within a complex ecosystem. Immunity is no longer understood solely as a function of white blood cells and antibodies, but as a conversation between host and microbe.
Future therapies may include microbiome profiling as a routine part of diagnosis. Treatments will be personalized, targeting microbial imbalances unique to each individual. Vaccines may be developed that modulate the microbiome to enhance immunity. Cancer therapies could be optimized based on microbial signatures that predict response to immunotherapy.
Even mental health may be approached through microbial lenses, treating depression with dietary changes, probiotics, or microbial metabolites that influence brain function.
But with this promise comes responsibility. As we learn to manipulate the microbiome, we must remember that we are dealing with a living, evolving system. Ethical considerations, long-term studies, and ecological awareness must guide our steps. The microbiome is not a tool to exploit—it is a partner to understand and nurture.
A Final Reflection: We Are Not Alone
The story of the microbiome is, ultimately, a humbling one. It reminds us that we are not solitary beings but ecosystems. We are host and habitat, human and more-than-human. The trillions of microbes that dwell within us are not parasites—they are part of what makes us whole.
They shape our immunity, our metabolism, our mood, and perhaps even our identity. They remember our exposures, guide our development, and protect us from the chaos of the outside world. In return, we offer them shelter, nutrients, and continuity across generations.
In the silence of our cells, the microbiome speaks. It speaks the language of molecules, of ancient symbiosis, of mutual survival. And as we listen more closely, we begin to understand not just the science of immunity—but the profound interdependence that defines life itself.