The human body is built on a staggering harmony. Every cell, every molecule, every whisper of immune activity is part of a finely tuned orchestra, defending us against invaders while sparing our own tissues. But what happens when that symphony goes awry? When the instruments of defense mistake the body’s own tissues for the enemy?
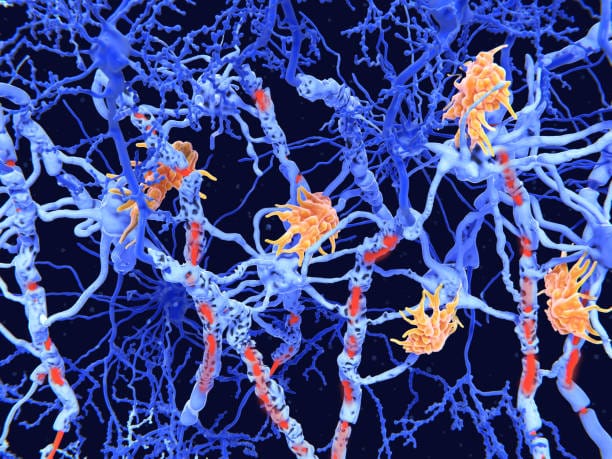
That is the dark paradox of autoimmune disease. In these complex and often mysterious conditions, the very system designed to protect us becomes a source of harm. White blood cells, antibodies, inflammatory chemicals—they all turn inward, attacking healthy organs, nerves, joints, and even skin.
For those who live with autoimmune diseases, the experience is often one of betrayal. The body, once a place of security and wholeness, becomes a battlefield. Pain, fatigue, swelling, and damage can flare up unpredictably. Diagnosis may be delayed by years. Treatment often focuses on calming the immune system without fully understanding why it rebelled in the first place.
And yet, in recent years, a new dimension to this story has emerged—one that is microscopic in size but cosmic in implication. Microbes—bacteria, viruses, fungi, and even parasites—appear to be intimately involved in shaping, training, and sometimes misguiding the immune system. These invisible passengers of our bodies may hold the key to both the origins of autoimmune disease and, perhaps, its eventual healing.
To understand this, we must journey into the immune system itself, then dive into the teeming world of the microbiome, and finally confront the delicate dance between humans and their microbial companions.
The Immune System: Friend and Foe
Our immune system is one of the most sophisticated defense networks in the natural world. It protects us from a constant barrage of threats—pathogens like viruses, bacteria, and parasites that would otherwise make short work of our tissues.
This defense system consists of two main arms: the innate immune system and the adaptive immune system. The innate immune system is the first line of defense. It responds quickly, often within minutes or hours, using barriers like skin, mucous membranes, and specialized cells that can destroy invaders without needing to recognize them specifically.
The adaptive immune system, on the other hand, is more precise. It includes T cells and B cells—types of white blood cells that can remember previous invaders and mount tailored responses to specific threats. Once trained, they can detect and destroy particular viruses, bacteria, or even cancerous cells. This learning process allows for immunity, either through natural infection or vaccination.
But the power of the immune system comes with a terrible risk. If it makes a mistake—if it misidentifies the body’s own tissues as foreign—it can unleash destruction on organs, nerves, or joints. This is autoimmunity: a case of mistaken identity with painful consequences.
A Landscape of Disease
There are more than 80 recognized autoimmune diseases, and their manifestations are as diverse as the tissues they attack. Multiple sclerosis targets the insulating sheaths of nerve cells in the brain and spinal cord, disrupting communication between the brain and body. Type 1 diabetes destroys insulin-producing cells in the pancreas, leading to life-long dependency on synthetic insulin. Rheumatoid arthritis inflames joints, often causing debilitating pain and deformity. Lupus, perhaps the most enigmatic of them all, can affect the skin, joints, kidneys, and even the heart and brain.
Some autoimmune diseases are organ-specific, while others are systemic, attacking multiple parts of the body. What unites them is the loss of tolerance: the immune system’s ability to distinguish self from non-self.
Women are disproportionately affected by autoimmune diseases, making up nearly 80% of all diagnosed cases. The reasons for this are still under investigation, though hormonal differences, genetic factors, and even X-chromosome dosage may play a role.
Genetics certainly contributes. Certain gene variants, especially those in the HLA (human leukocyte antigen) region, increase the risk of developing autoimmune diseases. But genetics alone doesn’t tell the whole story. In identical twins, if one twin develops an autoimmune disease, the other does not always follow—suggesting that something else must be involved.
That “something else” may lie in our relationship with the microbial world.
The Microbiome: An Invisible Organ
Inside your body, there are more microbial cells than human ones. Trillions of bacteria, viruses, archaea, and fungi live on your skin, in your mouth, in your lungs, and most abundantly, in your gut. This ecosystem of microorganisms, known collectively as the microbiome, weighs several pounds and functions like a hidden organ—one that digests food, synthesizes vitamins, and most intriguingly, educates the immune system.
From the moment of birth, the immune system is exposed to microbes. In fact, this exposure begins even earlier, as maternal microbes influence fetal development in ways scientists are only beginning to understand. During infancy, contact with maternal vaginal flora, breast milk, skin microbes, and the wider environment helps populate the newborn’s gut and skin with beneficial microbes. These microbes help “train” the immune system to recognize friend from foe.
Throughout life, the microbiome remains dynamic—shaped by diet, antibiotics, infections, travel, hygiene, stress, and more. In return, it shapes us. A healthy microbiome can promote tolerance, helping the immune system avoid overreacting to harmless stimuli like pollen, food proteins, or even the body’s own tissues. But a disrupted or imbalanced microbiome—called dysbiosis—can throw this balance into chaos.
Dysbiosis and Autoimmunity
Evidence has mounted in recent years that dysbiosis is linked to many autoimmune diseases. In patients with inflammatory bowel disease (IBD), for example, scientists have found a reduction in beneficial bacteria like Faecalibacterium prausnitzii and an overgrowth of pro-inflammatory species. In multiple sclerosis, gut microbiome studies have shown altered microbial populations, including bacteria that can stimulate autoreactive T cells.
In type 1 diabetes, certain microbial signatures appear in children months before the disease is clinically diagnosed. These changes may interact with a genetically primed immune system, tilting it toward self-destruction.
Rheumatoid arthritis has been linked to a curious microbe called Prevotella copri, which may trigger or amplify inflammatory responses in genetically susceptible individuals. Meanwhile, the presence or absence of certain bacteria seems to influence whether lupus flares remain dormant or erupt into full-blown disease.
But correlation does not always equal causation. Are microbes triggering these diseases, or is the disease state itself reshaping the microbiome? The answer is likely both. Inflammation can disrupt microbial communities, but microbial communities can also prime the immune system for attack. It’s a chicken-and-egg mystery at the heart of autoimmune science.
Molecular Mimicry and Friendly Fire
One of the ways microbes may trigger autoimmunity is through a phenomenon known as molecular mimicry. In this scenario, a microbial protein closely resembles a human protein. When the immune system launches a defense against the microbe, it also targets the body’s own tissues by mistake.
The bacterium Campylobacter jejuni, for instance, has been linked to Guillain-Barré syndrome—a condition in which the immune system attacks peripheral nerves, leading to paralysis. The bacterial surface molecules resemble components of human nerves, leading to mistaken immune attacks.
Epstein-Barr virus (EBV), a common herpesvirus that infects most people at some point, has been strongly linked to multiple sclerosis and lupus. Studies suggest that the virus may drive autoimmunity by activating latent B cells and triggering cross-reactive immune responses.
Streptococcal infections have been associated with autoimmune neuropsychiatric disorders in children (PANDAS), where immune responses to strep bacteria seem to attack parts of the brain involved in behavior and movement.
Even COVID-19, caused by the novel coronavirus SARS-CoV-2, has been implicated in triggering autoimmune responses in some patients, including autoimmune thyroiditis, Guillain-Barré, and lupus-like syndromes. Whether these cases reflect temporary immune overreaction or permanent reprogramming remains unclear.
The Hygiene Hypothesis: Too Clean for Our Own Good?
In the late 20th century, scientists began to notice an odd trend. In wealthier, industrialized countries—where infectious diseases had become rare—autoimmune and allergic diseases were on the rise. Asthma, type 1 diabetes, multiple sclerosis, celiac disease—all were more common in places with high hygiene standards, low infection rates, and widespread antibiotic use.
This led to the hygiene hypothesis: the idea that overly sterile environments deprive the immune system of the microbial “education” it needs in early life. Without exposure to a diverse array of microbes, the immune system may fail to develop proper regulatory mechanisms. As a result, it becomes more prone to misfires—targeting harmless allergens or the body’s own tissues.
Support for this idea has come from studies of children raised on farms, who are exposed to more diverse microbes through soil, animals, and unprocessed foods. These children are significantly less likely to develop autoimmune and allergic conditions than their urban counterparts.
Other research has looked at the role of parasitic worms (helminths), which were once common in human populations. Some helminths appear to modulate the immune system in ways that promote tolerance. In experimental models, infection with helminths can actually protect against autoimmune diseases like multiple sclerosis and colitis.
While no one is advocating a return to poor sanitation, these findings raise profound questions about how modern life has altered our microbial companions—and what that means for our immune health.
Restoring Balance: Toward Microbial Therapies
If the microbiome plays a role in the development of autoimmune disease, could it also be part of the cure?
The idea is no longer theoretical. Fecal microbiota transplantation (FMT)—the transfer of stool from a healthy donor into the gut of a sick person—has already shown dramatic success in treating Clostridium difficile infection, a life-threatening condition linked to antibiotic-induced dysbiosis.
Clinical trials are now exploring whether FMT or targeted probiotic treatments can help reset the microbiome in autoimmune diseases like ulcerative colitis, Crohn’s disease, and even multiple sclerosis. Early results are promising but mixed. The microbiome is extraordinarily complex, and transplanting it is not like swapping out a faulty part. Success may depend on matching donors and recipients, timing the intervention, and understanding which microbes matter most.
Some researchers are turning to “next-generation” probiotics—engineered or naturally occurring strains of bacteria that can deliver therapeutic effects. Others are investigating postbiotics (metabolites produced by beneficial microbes) or prebiotics (dietary fibers that nourish them) as ways to influence the immune system gently and safely.
Diet also plays a role. Diets rich in plant fibers and fermented foods appear to support a diverse and anti-inflammatory microbiome. Western-style diets, high in sugar, fat, and processed foods, may promote dysbiosis and inflammation. Personalized nutrition, based on individual microbiome profiles, may one day become part of autoimmune treatment.
Living with Autoimmunity: A Human Story
Behind every scientific theory or microbial discovery is a human being—often exhausted, frightened, and confused by what is happening inside their own body. For people living with autoimmune diseases, life can be a rollercoaster of flares and remissions, hope and disappointment, clarity and confusion.
The uncertainty of these diseases is part of what makes them so cruel. Symptoms can be invisible to others. Diagnosis may take years. Treatments often suppress the immune system broadly, increasing the risk of infections and other complications. And because these diseases are chronic, management becomes a lifelong journey.
Yet many people find strength, resilience, and meaning in that journey. They become experts on their own bodies. They learn to navigate healthcare systems, advocate for themselves, and find community with others who understand.
As our understanding of the microbiome and its role in immunity deepens, there is real hope for new treatments that go beyond symptom control and aim for true balance—restoring the immune system to its rightful place as guardian, not aggressor.
A Delicate Balance
The story of autoimmune disease is not one of simple cause and effect. It is a story of balance—between self and other, between attack and tolerance, between the immune system and the microbial world it grew up with.
Microbes are not merely invaders or passengers; they are co-evolutionary partners, whispering to our immune cells, shaping our development, and sometimes—tragically—leading us astray. Understanding how and why that happens is one of the great scientific quests of our time.
In the end, the solution may not lie in eradicating microbes or suppressing immunity, but in listening more deeply—to the signals of the microbiome, the language of the immune system, and the lived experiences of those whose bodies carry this burden.
Autoimmune diseases may be diseases of mistaken identity—but in seeking to understand them, we may rediscover something fundamental about who we are, and who we have always been: not alone, but in constant conversation with the invisible life within and around us.