Every moment of every day, your body is engaged in a war. Not the kind of war we read about in history books or see in the news—but a ceaseless, invisible war that plays out beneath the surface of your skin. Billions of microscopic invaders—bacteria, viruses, fungi, parasites—are constantly seeking ways to infiltrate, colonize, and use your body for their own ends. And yet, you wake up each morning unharmed, unaware, and oblivious to the daily siege. Why?
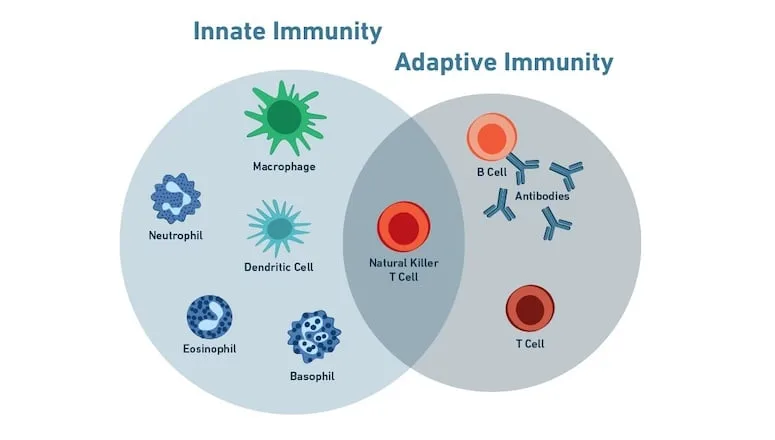
Because inside you, an intricate defense system operates with astonishing precision and adaptability. This is your immune system—a vast network of cells, tissues, and molecules that guards you from the microbial world with relentless vigilance. It is not one monolithic force, but rather two interconnected realms: innate immunity and adaptive immunity. Together, they form a biological symphony of defense, each with its own tempo, instruments, and strategies.
To understand how your body survives and thrives in a microbial world, we must journey into the inner workings of these two arms of immunity. It is here that we witness the raw, immediate power of nature’s first responders and the elegant, learning power of its long-term strategists.
What Is Innate Immunity?
Innate immunity is the body’s first line of defense. It is ancient, fast, and brutally efficient. From the moment you are born—and in fact, even before—you possess an inborn arsenal of defenses designed to identify and destroy invaders. This part of the immune system does not require prior exposure to a pathogen to act. It is always ready. It is instinct.
When a pathogen breaches the physical barriers of the body—such as the skin or the mucous membranes of the nose, mouth, or gut—the innate immune system leaps into action. Its response is immediate. Within minutes or hours, immune cells flood the site of infection, engulfing invaders, releasing chemical signals, and triggering inflammation. This is the immune system’s version of sounding the alarm.
Cells like neutrophils, macrophages, dendritic cells, and natural killer (NK) cells dominate this early defense. Each has evolved to detect broad patterns shared by many microbes—patterns that humans have encountered for millennia. These include certain carbohydrate molecules on bacterial surfaces, or double-stranded RNA associated with viruses. The innate immune system doesn’t need to know the name of the invader; it only needs to recognize the danger.
But while innate immunity is rapid and vital, it has limitations. It is not specialized. It doesn’t remember. It treats every threat the same way, whether it’s a mild cold virus or a lethal bacterial toxin. And once the immediate threat is controlled, innate immunity fades away. It is a blunt sword—powerful but indiscriminate.
The Power of Inflammation
One of the hallmark features of the innate immune response is inflammation. This familiar yet misunderstood process is not merely a symptom—it is a carefully orchestrated strategy.
When tissues are damaged or infected, cells release signaling molecules called cytokines and chemokines. These chemicals dilate blood vessels, increase their permeability, and recruit immune cells to the battlefield. The heat, redness, swelling, and pain that characterize inflammation are not signs of defeat, but of mobilization.
Neutrophils, the most abundant white blood cells, are often the first to arrive. They engulf and digest microbes in a process known as phagocytosis. Macrophages join them, not only destroying pathogens but also cleaning up debris and coordinating the next phases of the response. These cells act without hesitation, driven by signals hardwired into their biology.
Yet, inflammation is a double-edged sword. Left unchecked, it can damage healthy tissue. Chronic inflammation is at the heart of many diseases—from arthritis to heart disease to neurodegeneration. The immune system must walk a tightrope between aggression and restraint, a balance it has honed over eons of evolution.
The Role of Pattern Recognition
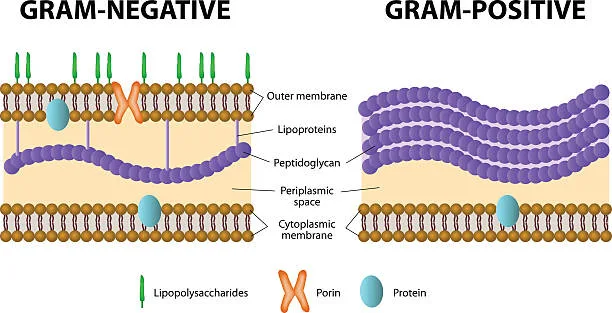
Innate immunity operates through a set of molecular sensors known as pattern recognition receptors (PRRs). These receptors detect pathogen-associated molecular patterns (PAMPs)—signature molecules common to broad classes of microbes.
Toll-like receptors (TLRs), one of the best-known families of PRRs, are found on immune cells and even on non-immune cells like skin and gut epithelium. They act like security scanners at an airport, quickly identifying suspicious items and triggering alarms.
Each TLR is tuned to detect specific microbial patterns: bacterial flagella, lipopolysaccharides, viral RNA, and more. When a TLR is activated, it sets off a cascade of signaling pathways that lead to inflammation, recruitment of immune cells, and the activation of genes involved in defense.
This system, while lacking memory, is astonishingly efficient. It ensures that the body reacts swiftly to the first sign of infection. But for a deeper, more tailored, and longer-lasting response, another system must be called upon.
The Rise of Adaptive Immunity
If innate immunity is nature’s hammer, adaptive immunity is its scalpel. It is precise, slow to awaken, but capable of extraordinary feats of memory and specificity. Adaptive immunity is what allows the body to “learn” from past infections and become stronger with each encounter.
Unlike innate immunity, the adaptive system does not rely on recognizing generic patterns. Instead, it creates unique receptors—billions of them—each capable of identifying a specific molecular fragment of a pathogen, called an antigen. This remarkable diversity is generated through genetic rearrangement during the development of lymphocytes, the chief architects of the adaptive immune system.
There are two main types of lymphocytes: B cells and T cells. B cells are responsible for producing antibodies—molecular homing missiles that target pathogens for destruction. T cells come in several forms: helper T cells that coordinate the immune response, cytotoxic T cells that destroy infected cells, and regulatory T cells that keep the system from overreacting.
The adaptive response takes time to develop. After an initial infection, it may take days for T cells and B cells to expand and mature. But once they do, they not only eliminate the current threat but also leave behind a trail of memory—cells that will recognize the same pathogen years, even decades later.
This is the power behind vaccines: by exposing the body to a harmless version of a pathogen, we train the adaptive immune system to recognize and eliminate the real threat before it can gain a foothold.
Antibodies: The Body’s Precision Weapons
Antibodies, or immunoglobulins, are Y-shaped proteins produced by activated B cells. Each antibody is a unique molecular lock, shaped to bind to a specific key—the antigen. When an antibody binds to its target, it can neutralize toxins, prevent viruses from entering cells, or mark invaders for destruction by other immune cells.
There are several classes of antibodies, each tailored to different environments and functions. IgA patrols mucosal surfaces; IgG circulates in the blood; IgE is involved in allergic reactions and defense against parasites.
The beauty of antibodies lies in their precision. While innate immunity might treat all bacteria the same, antibodies can distinguish between different strains of the same virus. This allows the immune system to fine-tune its attack and avoid unnecessary collateral damage.
Moreover, once a B cell has been activated and matured, it can transform into a memory B cell. These cells persist in the body for years, scanning for the return of their specific foe. If the same pathogen returns, the memory B cells rapidly churn out antibodies in overwhelming numbers—often eliminating the invader before symptoms ever appear.
T Cells and Cellular Immunity
While B cells handle extracellular threats, T cells are the guardians of the inner world. They detect and respond to infected or abnormal cells that hide viruses or harbor mutations.
Cytotoxic T cells patrol the body looking for cells that display viral or abnormal peptides on their surface. These cells carry the molecular equivalent of a sniper rifle: a lethal dose of granules that, once delivered, induce the infected cell to self-destruct.
Helper T cells do not kill directly but are critical for coordinating the immune response. They secrete cytokines that stimulate B cells, activate cytotoxic T cells, and recruit other immune cells to the site of infection. Without helper T cells, the adaptive response is crippled—something dramatically illustrated in diseases like HIV/AIDS, where these cells are destroyed.
Regulatory T cells serve as peacekeepers. Once a threat has passed, they help shut down the immune response, preventing excessive inflammation and autoimmunity. This ability to self-regulate is what makes the adaptive immune system not just powerful, but wise.
Memory: The Soul of Adaptive Immunity
One of the most astonishing features of adaptive immunity is its memory. After an infection is cleared, memory B cells and memory T cells remain in the body, sometimes for a lifetime. These cells carry the genetic imprint of the pathogen and are poised for action if it ever returns.
This immunological memory explains why diseases like measles, mumps, or chickenpox usually occur only once. It also underpins the science of vaccination, which simulates an infection to create memory without causing disease.
Memory cells respond faster and more vigorously than naive cells. A second encounter with the same pathogen triggers a massive and rapid immune response, often preventing illness altogether. In essence, the body becomes smarter with every microbial encounter, building a molecular diary of past battles and victories.
The Dance Between Innate and Adaptive Immunity
Though often treated as separate entities, innate and adaptive immunity are deeply intertwined. The innate system sets the stage—it senses the presence of a threat, alerts nearby cells, and creates an environment that allows adaptive responses to develop.
Dendritic cells, which straddle both worlds, are especially important. They act as sentinels, capturing antigens from invaders and presenting them to T cells in the lymph nodes. This antigen presentation is the critical handshake between innate recognition and adaptive precision.
In return, the adaptive system fine-tunes the innate response. Antibodies can enhance phagocytosis, while cytokines released by T cells modulate the behavior of innate cells. It is a dance of mutual instruction and adaptation—a system that learns, evolves, and responds with increasing elegance.
When the System Fails
Despite its sophistication, the immune system is not infallible. When the balance between innate and adaptive immunity breaks down, disease can follow.
In autoimmune disorders, the adaptive system mistakenly targets the body’s own tissues, unable to distinguish self from non-self. In immunodeficiencies, parts of the system are missing or malfunctioning, leaving the body vulnerable. Chronic inflammation, allergies, and cancer all represent different kinds of immune dysfunction—instances where the system is too aggressive, too weak, or misdirected.
Understanding the intricate relationship between innate and adaptive immunity is critical for treating these conditions. Modern therapies increasingly target specific parts of the immune system—blocking inflammatory cytokines, suppressing T cell activity, or engineering new immune responses through CAR-T cells or monoclonal antibodies.
The Future of Immunity
The immune system is a frontier still unfolding. Scientists are discovering new cell types, signaling pathways, and molecular mechanisms every year. The boundary between innate and adaptive immunity is more porous than once believed. Cells like innate lymphoid cells and trained immunity blur the lines, suggesting that even innate responses can adapt, learn, and evolve.
In a world facing new infectious diseases, antimicrobial resistance, and rising rates of autoimmune and allergic disorders, understanding immunity is not just a scientific quest—it is a moral imperative. Vaccines, immunotherapies, gene editing, and microbiome research all hold promise for strengthening and harnessing our inner defenses.
But beyond the science lies something even more profound: a deeper appreciation for the hidden intelligence of the body. Your immune system is not merely a defense—it is a story of connection, recognition, and memory. It is a whisper from your evolutionary past and a guardian of your future.
A Closing Reflection
The war inside you is never over, but it is not fought with chaos or fear. It is waged with purpose, intelligence, and compassion. The innate immune system rushes in first, fearless and unwavering, ready to sacrifice itself to protect the whole. The adaptive immune system arrives later, slower but more refined, learning from the enemy and ensuring it can never strike again in the same way.
Together, they are not just parts of a defense—they are expressions of life’s resilience. They are the reason you can heal from wounds, recover from colds, and live in harmony with a world teeming with microbes. In every heartbeat, they are there—silent, vigilant, and endlessly wise.