In the deepest chambers of the body, far below conscious awareness, a fire can begin to smolder. This fire doesn’t burn with flames, but with cells and signals—fierce and focused, ancient as life itself. We call it inflammation. For many, the word conjures up images of red, swollen joints or puffy, irritated skin. But inflammation is far more than discomfort. It is one of the most powerful tools the body possesses to protect itself—and sometimes, to destroy itself.
Inflammation is a biological response, a kind of internal emergency system, that springs into action when tissues are injured or threatened. It is part of our immune system’s ancient arsenal, a cascade of molecules and cells that race to the site of trouble. Without inflammation, a simple scratch could become fatal. Yet when inflammation spirals out of control or fails to turn off, it can drive chronic diseases, from heart disease to cancer, arthritis to Alzheimer’s.
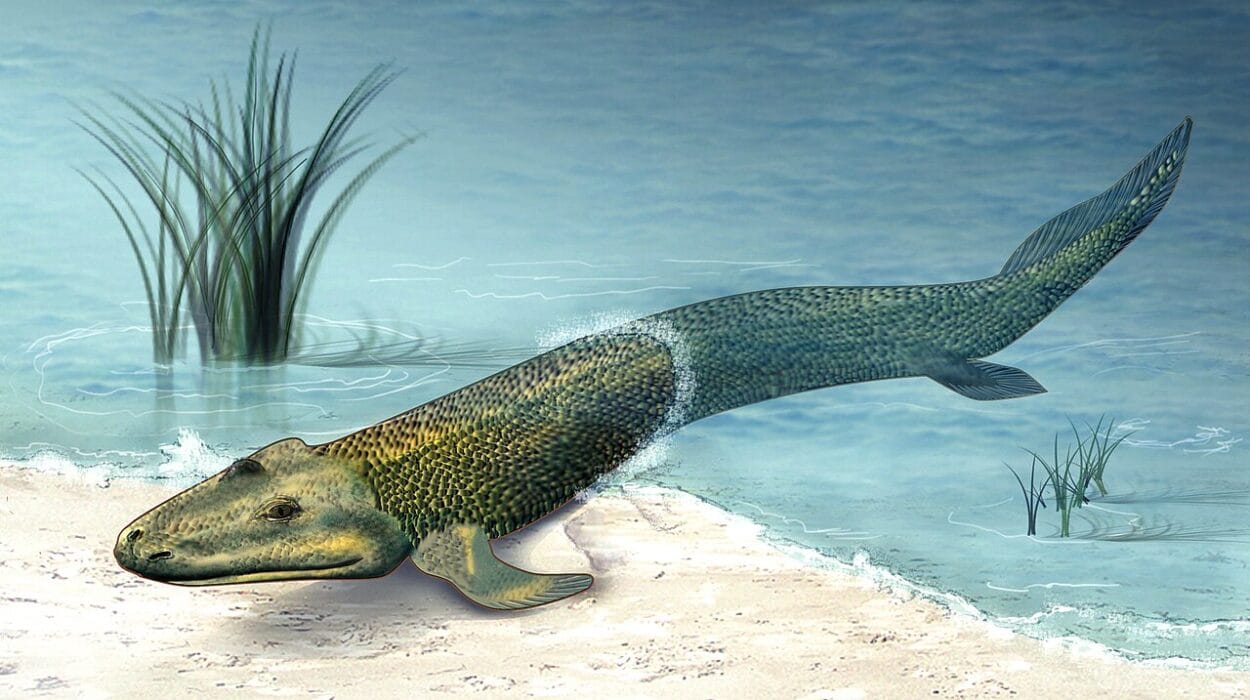
But what exactly sets this fire alight? One of the most potent sparks is infection—especially by microbes: bacteria, viruses, fungi, and parasites. These tiny invaders have coexisted with us for millions of years, evolving to slip past our defenses, hijack our cells, and even manipulate our immune responses. And in turn, our bodies have evolved to recognize them instantly and respond with ferocity.
To understand inflammation is to understand the very nature of survival: how the body wages war and seeks balance, how it remembers old enemies and fears new ones, and how the tiniest microbe can unleash a thunderstorm of cellular fury.
The Biology of Inflammation: A Controlled Chaos
At its core, inflammation is a protective response. It is the body’s way of eliminating harmful stimuli—such as damaged cells, irritants, or pathogens—and initiating the healing process. When a pathogen breaches the body’s first lines of defense (like the skin or mucosal membranes), the immune system sounds the alarm. Cells near the breach begin producing molecular signals—called cytokines and chemokines—that summon immune cells to the site.
Blood vessels dilate, increasing blood flow. This is why inflamed areas often appear red and feel warm. The vessel walls become more permeable, allowing immune cells, fluids, and proteins to leak into the surrounding tissue. This creates swelling and may stimulate nearby nerves, causing pain.
There are two major types of inflammation: acute and chronic. Acute inflammation is short-lived, lasting minutes to days. It’s the body’s rapid and focused response to injury or infection, designed to contain and eliminate the threat. Chronic inflammation, on the other hand, lingers. It can smolder for months or years, often in response to persistent infection, autoimmunity, or even environmental toxins. This chronic inflammation can slowly damage tissues, contributing to disease.
In both types, inflammation is not just an act of destruction. It is also an act of repair. After the threat is eliminated, the same immune cells that fought the invaders help clean up the debris and guide tissue regeneration. Ideally, inflammation ends with resolution—a return to homeostasis. But in many diseases, that resolution never fully arrives.
The Role of Microbes: Ancient Adversaries and Allies
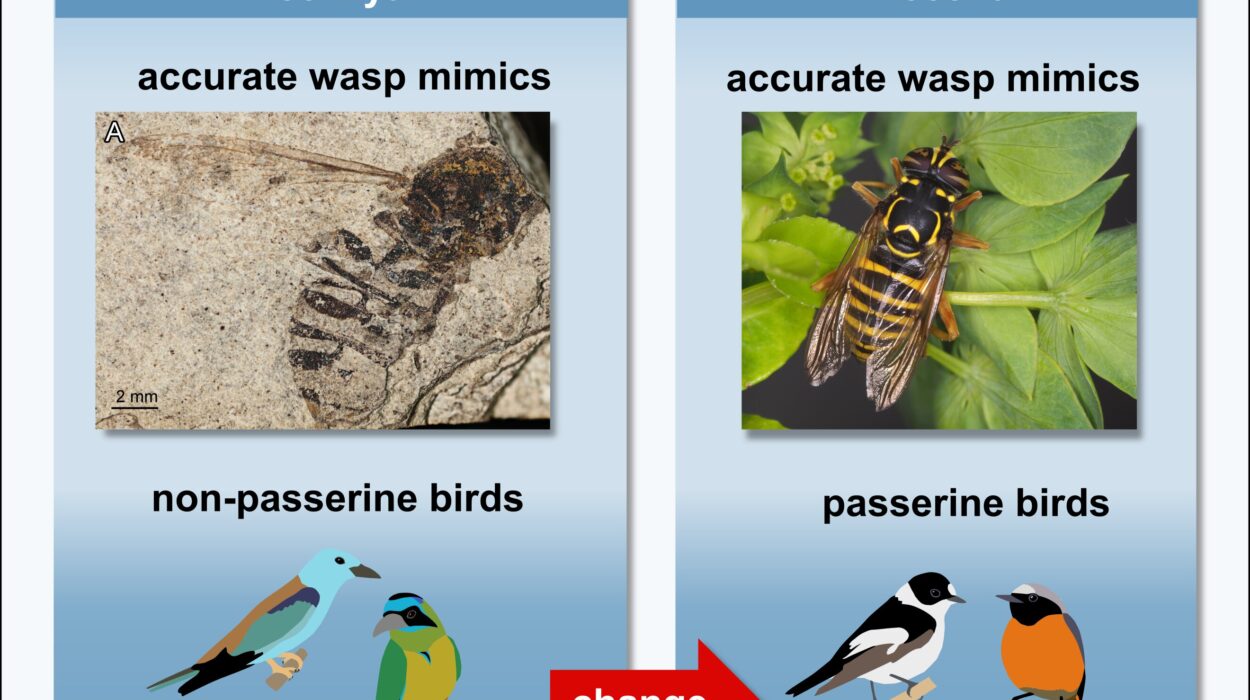
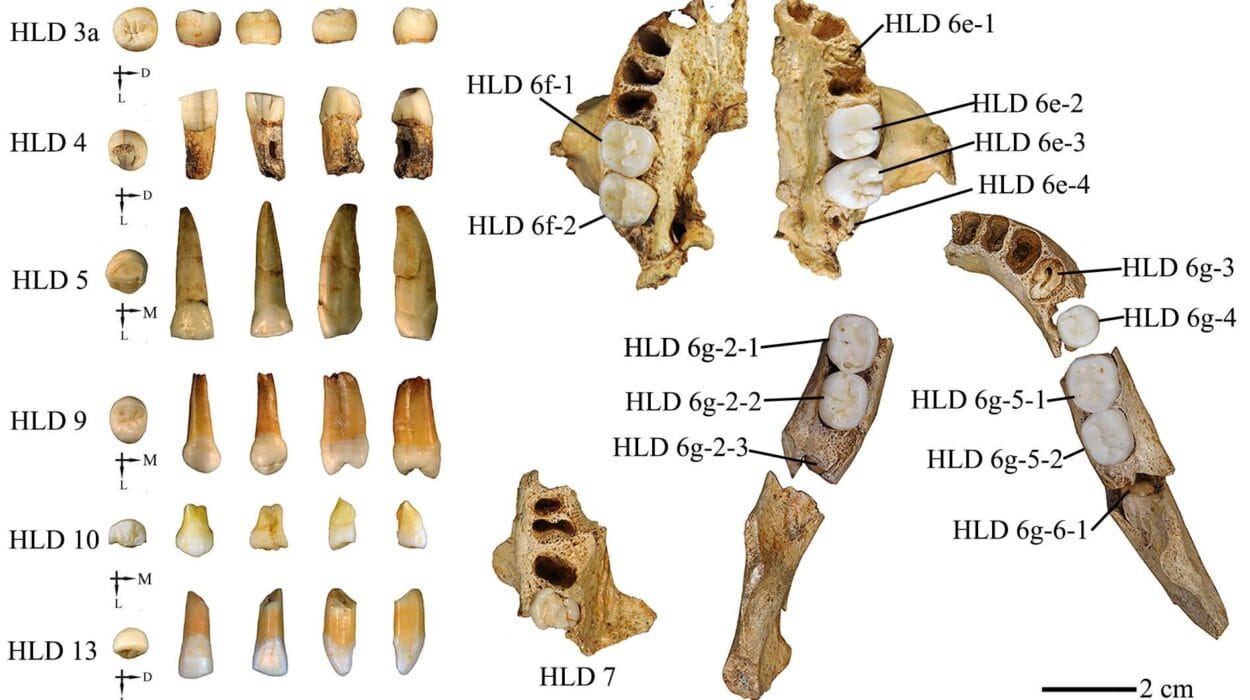
Microbes have existed on Earth for billions of years. Long before humans evolved, these tiny life forms were already engaged in complex battles for survival. Some microbes have always been harmful, causing disease and death. Others are essential to our health—forming the microbiome that lives in our guts, skin, lungs, and more.
The relationship between microbes and the human immune system is intricate and dynamic. On one hand, the immune system must recognize and destroy pathogens quickly and efficiently. On the other, it must tolerate and even cooperate with beneficial microbes. This delicate balance is learned over time, beginning at birth, as the body is colonized by its first microbes.
But when a harmful microbe breaches our defenses, the immune system doesn’t hesitate. It activates inflammation to isolate, destroy, and remove the invader. Different types of microbes trigger different kinds of inflammatory responses—each tailored to the invader’s structure, behavior, and method of attack.
For example, bacteria that live outside cells—like Staphylococcus aureus—are often met with neutrophils, the immune system’s first responders, who engulf and kill them. Viruses, which hide inside host cells, trigger a different set of alarms—interferons, cytotoxic T cells, and natural killer cells that target infected cells for destruction.
In this evolutionary arms race, microbes have developed sophisticated ways to avoid detection or suppress inflammation. Some bacteria produce molecules that mimic human proteins, confusing immune cells. Others hide within host cells, cloaked from view. Viruses can disable immune signaling pathways or even exploit them for their own replication. Despite these tricks, the immune system often wins—but not without cost.
Pattern Recognition: How the Body Knows a Microbe Has Arrived
To initiate inflammation, the immune system first has to recognize that something is wrong. It does this using molecular “sensors” known as pattern recognition receptors (PRRs). These receptors are found on the surfaces and insides of immune cells, and they detect pathogen-associated molecular patterns (PAMPs)—distinctive molecular signatures found only on microbes.
These PAMPs can include things like bacterial cell wall components (lipopolysaccharides), flagellin (a protein in bacterial flagella), double-stranded RNA (from viruses), or fungal cell wall sugars. When PRRs detect these patterns, they activate signaling pathways inside the immune cell, triggering the production of inflammatory mediators like cytokines, prostaglandins, and reactive oxygen species.
Toll-like receptors (TLRs) are one of the most well-known families of PRRs. They act like watchtowers, each tuned to detect a different microbial signal. Some are on the cell surface, detecting bacteria or fungi; others are inside, sensing viral genetic material.
The engagement of PRRs launches the inflammatory response almost immediately. Cells signal for reinforcements, blood flow increases, and within hours, the area becomes a battlefield.
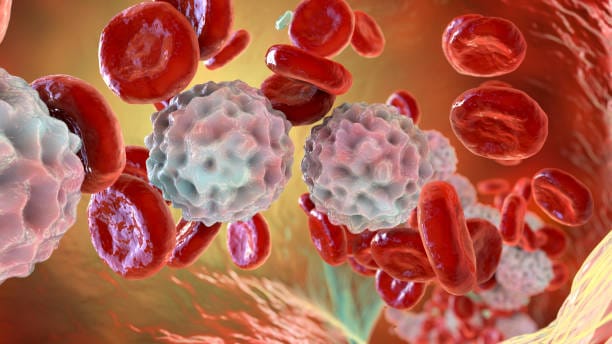
The Soldiers of Inflammation: Cells on the Front Lines
The inflammatory response mobilizes a diverse and powerful army. Each type of immune cell plays a specialized role in the defense against microbes.
Neutrophils are the most abundant white blood cells in the bloodstream and the first to arrive at the site of infection. They engulf pathogens in a process called phagocytosis and then kill them with toxic enzymes and reactive oxygen species. Their lifespan is short—they often die within hours, leaving behind a trail of cellular debris and pus.
Macrophages arrive slightly later. These long-lived cells continue the fight but also help clean up the mess, ingesting dead cells and signaling for tissue repair. Macrophages also present pieces of microbes to other immune cells, acting as a bridge between the innate and adaptive immune systems.
Dendritic cells play a similar role, carrying microbial antigens to lymph nodes, where they activate T cells and B cells—the memory-makers of the immune system. T cells, once activated, can kill infected cells or coordinate the immune response. B cells produce antibodies that bind to microbes and mark them for destruction.
Natural killer (NK) cells, another frontline defense, are especially important against viruses. They can detect cells that are stressed, damaged, or altered by infection and kill them before the virus can spread.
The orchestration of these cells and their signals creates a wave of inflammation that can eliminate an infection swiftly—but if misdirected, can cause severe collateral damage.
Microbial Masterminds: How Pathogens Exploit Inflammation
Just as the immune system has evolved to detect and destroy microbes, pathogens have evolved to manipulate inflammation to their advantage.
Some bacteria, like Mycobacterium tuberculosis, can survive inside macrophages, avoiding destruction while triggering just enough inflammation to keep immune cells coming—creating a long-lasting infection. Helicobacter pylori, which infects the stomach lining, can induce chronic inflammation that damages tissue over time, increasing the risk of ulcers and cancer.
Certain viruses, such as HIV, actively suppress inflammatory signals that would lead to their elimination. Others, like the influenza virus, provoke an overwhelming inflammatory response—known as a cytokine storm—that can be more deadly than the infection itself.
Parasitic worms (helminths) take a different approach. Rather than triggering intense inflammation, they often induce a more tolerant, anti-inflammatory response that allows them to live undisturbed within their host for years.
Even some members of the microbiome can cause trouble if they find themselves in the wrong place. When gut bacteria escape the intestine—through injury, leaky gut, or surgery—they can trigger a massive inflammatory response called sepsis, which can be fatal.
The microbial world is not just a battlefield—it’s a complex chessboard, where each side is constantly adapting to outmaneuver the other.
Inflammation Gone Wrong: When the Response Becomes the Problem
While inflammation is meant to protect, it can become a double-edged sword. An uncontrolled or misguided inflammatory response can damage healthy tissues and organs, leading to chronic disease.
Sepsis, the body’s overreaction to a systemic infection, floods the bloodstream with inflammatory mediators. Blood pressure drops, organs fail, and without swift treatment, death follows. Sepsis is one of the leading causes of death in intensive care units worldwide.
In autoimmune diseases, the immune system mistakenly identifies the body’s own cells as microbial invaders. Diseases like lupus, rheumatoid arthritis, and multiple sclerosis arise when this misidentification leads to chronic inflammation against healthy tissues.
Persistent infections can also drive chronic inflammation. Hepatitis B and C viruses, for example, can cause long-term liver inflammation that eventually leads to fibrosis, cirrhosis, or cancer. Human papillomavirus (HPV) infection of the cervix can provoke changes that lead to cervical cancer.
Even in the absence of infection, microbial products can still trigger inflammation. In conditions like inflammatory bowel disease (IBD), components of the gut microbiota may activate immune responses that never fully shut off, leading to cycles of flare-ups and damage.
The Resolution Phase: Turning Off the Alarm
For inflammation to be beneficial, it must end. The body cannot remain in a state of high alert forever. Fortunately, the immune system has built-in mechanisms for resolution—a phase where inflammation is actively turned off and healing begins.
This phase is not passive. Specialized molecules called resolvins, protectins, and maresins—derived from omega-3 fatty acids—help dampen inflammation and promote tissue repair. Macrophages change their behavior, becoming more focused on cleanup than combat. Regulatory T cells arrive to suppress further immune activation.
In healthy people, this resolution phase ensures that the fire of inflammation is extinguished before it consumes the host. But in chronic inflammation, this phase may fail to occur properly, or the body may lose the ability to return to baseline. Understanding how to control this transition is one of the great frontiers of immunology.
Future Frontiers: Harnessing Inflammation for Healing
As our understanding of inflammation and its microbial triggers deepens, so too does our ability to manipulate it for medical benefit. New therapies aim not only to block inflammation but to fine-tune it—preserving its protective qualities while avoiding harm.
Monoclonal antibodies now target specific cytokines—like TNF-alpha or interleukin-6—to treat diseases like rheumatoid arthritis and inflammatory bowel disease. Drugs that mimic resolvins are being developed to promote resolution. Probiotics and prebiotics are being explored to rebalance the gut microbiota and reduce inflammation.
Vaccines are another powerful tool. By training the immune system to recognize microbial threats in advance, they can prevent infection and the inflammatory damage that follows.
The rise of personalized medicine may allow us to tailor anti-inflammatory treatments based on a person’s genetics, microbiome, and immune profile. And researchers are investigating how diet, stress, sleep, and lifestyle influence inflammation, offering hope that everyday choices can support a more balanced immune response.
Conclusion: The Fire That Protects—and Burns
Inflammation is a paradox—a fierce protector that can also become a source of harm. It is the body’s answer to danger, triggered by the tiniest sparks: the molecules of a bacterium, the strands of a virus, the whispers of fungal spores. In responding to these microbial threats, the body summons forces of extraordinary power. But this power must be controlled.
Our evolving understanding of inflammation reveals not just the complexity of the immune system, but the fragile tightrope the body walks between defense and destruction. It shows us how deeply we are entangled with the microbial world, how our health depends on a constant and careful negotiation with the invisible life around—and within—us.
The future of medicine may lie in our ability to master this balance: to extinguish the harmful fires of inflammation while preserving their protective flame. For in the fire lies both the story of disease—and the promise of healing.