For generations, the responsibility of birth control has fallen disproportionately on women. While scientific advances have offered an expanding arsenal of hormonal pills, patches, intrauterine devices, and implants for women, men have been left with little more than two options: condoms—unreliable, with a 13% failure rate—or vasectomy, a permanent surgical solution not easily reversible. But now, a quiet revolution is stirring in the world of reproductive medicine. A compound known as YCT-529 may finally be opening the door to safe, reversible, non-hormonal male contraception.
In an era that demands greater reproductive equity, the first human data on YCT-529 offers a rare glimmer of hope—and scientific rigor. Developed by YourChoice Therapeutics in collaboration with Quotient Sciences and Incyte, this experimental compound has passed a crucial early milestone: proving safe in healthy men, with no significant side effects, and reaching blood levels in humans that were previously shown to induce reversible infertility in nonhuman primates.
Science Without Hormones: Why YCT-529 Is Different
Most birth control methods that regulate fertility do so by targeting hormones. But for men, this strategy has proven elusive. Attempts to manipulate testosterone or other sex hormones have often resulted in side effects such as mood swings, decreased libido, and even long-term cardiovascular risks. YCT-529 breaks away from this hormonal path entirely.
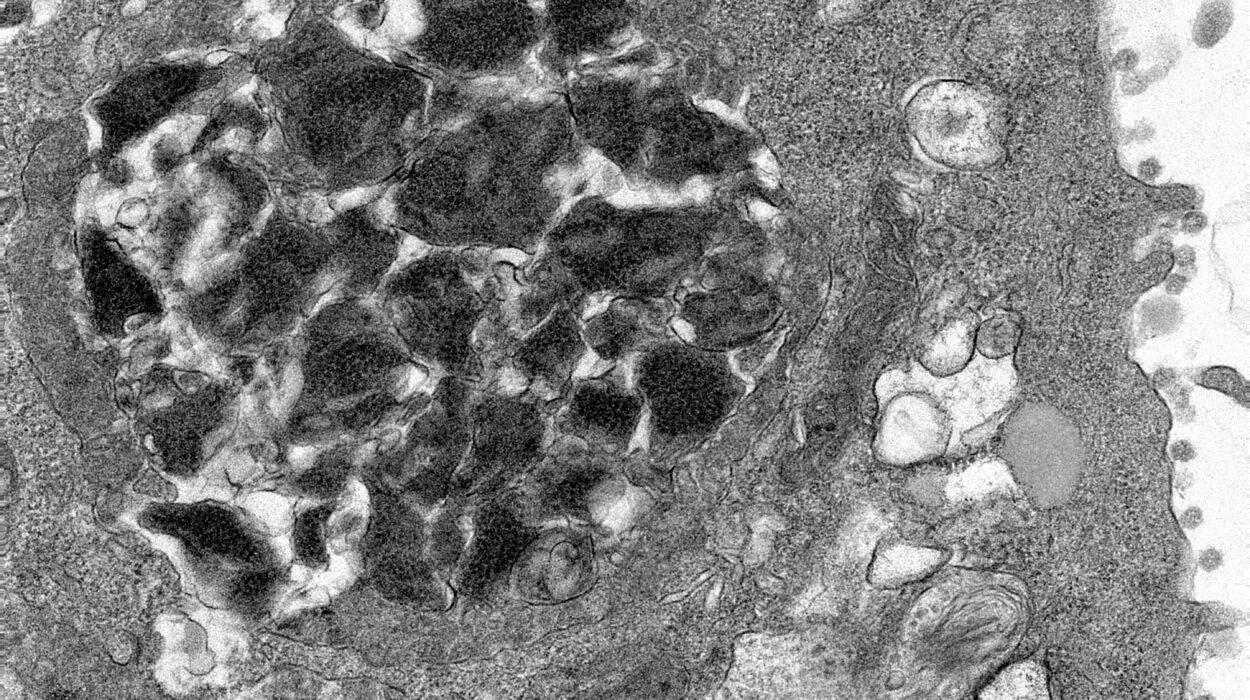
Instead, YCT-529 targets the retinoic acid receptor alpha (RAR-α)—a protein essential for sperm production. Blocking this receptor interrupts the cellular processes that guide sperm maturation. Animal studies have shown that interfering with RAR-α doesn’t suppress testosterone levels or affect sexual behavior, but it effectively halts the body’s ability to produce viable sperm. The effect is reversible, and crucially, it doesn’t interfere with the hormone feedback systems that govern mood, libido, or general metabolism.
The First Human Trial: A Carefully Designed Step Forward
In a groundbreaking study titled “Safety and pharmacokinetics of the nonhormonal male contraceptive YCT-529,” published in Communications Medicine, researchers carefully tested the compound in humans for the first time. It was a single-ascending-dose trial, randomized, double-blind, and placebo-controlled—the gold standard in clinical research.
Sixteen vasectomized men aged between 32 and 59 participated. Each was in good health, with body mass indexes (BMI) between 21.9 and 31.1 kg/m². Twelve received YCT-529 at ascending doses, while four received a placebo. The use of vasectomized men ensured that any future fertility impacts could be isolated from safety concerns in this early-phase trial.
Participants took the drug orally, in capsule form, with water. For 14 days afterward, they were closely monitored using continuous Holter ECGs to track heart rhythms, serial blood draws to monitor drug concentrations and biomarkers, psychosexual diaries to record any mood or libido changes, and inflammatory marker panels to catch any hidden biological shifts.
Safety First: The Results That Matter
The outcome was both reassuring and exciting. Across all doses—up to a maximum of 180 mg—no serious or severe side effects emerged. One participant developed a brief, symptomless arrhythmia at two dose levels (90 mg and 180 mg), but follow-up cardiology evaluation found no structural heart issues. Importantly, electrocardiogram (ECG) modeling demonstrated that YCT-529 did not prolong the heart’s electrical repolarization process. It stayed well below the threshold (10 milliseconds) that regulators use as a red flag for cardiac risk.
Other clinical tests were equally stable. Blood chemistry, hematology, urinalysis, and coagulation profiles showed no clinically meaningful deviations. Mood and libido, tracked through self-reports, remained unchanged. Inflammatory markers, too, remained within normal ranges, with one mild exception: a transient increase in IL-6 levels in one participant, likely linked to diet rather than the drug itself.
Pharmacokinetics—the study of how the drug behaves in the body—provided further promising news. The time to peak blood concentration (Tmax) ranged from four to 10 hours, and the geometric-mean half-life (how long the drug stayed active in the body) ranged from 51 to 76 hours. That means YCT-529 has the potential to be a once-daily or even less frequent dosing option. Notably, food increased drug absorption, although variability in those results made it difficult to draw firm conclusions.
Matching Animal Benchmarks for Infertility
Perhaps the most important result came from measuring drug exposure. At the 180 mg dose, the area under the curve (AUC)—a metric used to gauge the body’s total exposure to a drug over time—reached around 27,300 h·ng/mL. This matches the exposure levels that, in nonhuman primate studies, reliably produced temporary infertility.
Yet in the human subjects, levels of key reproductive hormones—testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and sex hormone-binding globulin (SHBG)—remained solidly within reference ranges. There was no evidence of systemic hormonal disruption, validating the compound’s non-hormonal mechanism in a real-world setting.
The Psychological Dimension: Trusting the Male Pill
One of the long-standing barriers to male contraception isn’t just science—it’s social trust. Would men willingly take a pill? Would their partners trust them to? These are valid concerns. That’s why understanding not only the biology but also the lived experience of taking YCT-529 matters so much.
This trial wisely incorporated psychosexual diaries, asking men to report on libido, mood, arousal, and sexual performance. None of these factors changed significantly across the dosing spectrum. There were no reported episodes of depression, no libido crashes, and no negative shifts in sexual confidence. This is critical, because any contraceptive method—no matter how effective—must be emotionally neutral or even positive to gain acceptance.
The early findings suggest that YCT-529 won’t just work biologically. It will also work socially, emotionally, and psychologically—making it far more likely to succeed where others have failed.
A Glimpse of What’s Next
This study marks only the beginning. YCT-529 has cleared one of the highest hurdles in drug development: establishing early human safety at pharmacologically meaningful doses. But now comes the even harder part—proving that repeat doses over time can safely and reliably suppress sperm production in fertile men, and that fertility returns once the drug is stopped.
An ongoing trial is now exploring just that, monitoring volunteers over 28- and 90-day repeat-dose windows. Scientists will be looking for sperm count suppression, full hormone profiles, and extended safety data. If YCT-529 continues to perform as it has, the world may soon witness a breakthrough as monumental as the birth control pill was for women in the 1960s.
Beyond Biology: Toward Reproductive Equality
It’s easy to talk about YCT-529 as just a chemical compound, a lab-born molecule with a promising future. But its potential is far more profound. In a world where half of all pregnancies are unintended, where reproductive responsibility has largely fallen on one gender, and where options for men have remained stagnant for decades, YCT-529 represents a quiet but powerful social revolution.
Giving men safe, reversible contraception doesn’t just expand their autonomy—it also frees couples from gendered burdens, improves family planning outcomes, and reduces global abortion rates. It means that contraception becomes a shared responsibility, a collaborative choice rooted in trust and science rather than asymmetrical sacrifice.
The Road Ahead
The journey of YCT-529 is far from over. Many experimental drugs stumble in the transition from early trials to long-term safety and effectiveness. The history of male contraception is filled with dashed hopes and abandoned projects, from WIN 18,446 (which caused dangerous alcohol reactions) to gossypol (linked to dangerously low potassium levels). YCT-529 must still prove it can achieve reversible, reliable infertility in diverse populations under real-world conditions.
But for the first time in decades, a scientifically grounded, emotionally tolerable, socially acceptable option is within sight. And if YCT-529 succeeds, it may not just redefine male contraception—it may redefine what shared responsibility looks like in the 21st century.
Conclusion: From Hope to Reality
Science often advances in silent moments—laboratory breakthroughs, quiet clinical trials, carefully logged blood samples. But sometimes, those moments reverberate far beyond the lab, reshaping how society functions. The development of YCT-529 is one such moment.
It is more than a molecule. It is a symbol of equity, a testament to scientific persistence, and a potential game-changer in human reproductive health.
If the ongoing studies validate its promise, YCT-529 may not only prevent pregnancies—it may rewrite the rules of who bears the burden of prevention. And in doing so, it may give rise to a future where men and women walk into parenthood—or choose to avoid it—not alone, but side by side.
Reference: Nadja Mannowetz et al, Safety and pharmacokinetics of the non-hormonal male contraceptive YCT-529, Communications Medicine (2025). DOI: 10.1038/s43856-025-01004-4