In the modern world, where food is more abundant than ever and lifestyles have become increasingly sedentary, one condition has quietly—and sometimes not so quietly—become a defining health challenge of our time: obesity. Once considered a problem of only wealthy nations, obesity is now a global epidemic that spans across every continent, age group, and socioeconomic class. According to the World Health Organization, obesity rates have nearly tripled since 1975, and today, more than 1 billion people worldwide are classified as obese.
But the story of obesity is not just about body weight or physical appearance. At its core, it is about health and survival. Obesity is far more than an aesthetic concern; it is a biological state that profoundly disrupts the body’s natural balance and fuels the onset of chronic diseases—conditions that can last a lifetime and diminish both quality of life and longevity. From diabetes to cardiovascular disease, from certain cancers to joint disorders, the web of connections between obesity and chronic illness is complex and deeply concerning.
To truly understand the gravity of this crisis, we must go beyond statistics and explore the intricate relationship between excess weight and the diseases that often follow in its wake.
Defining Obesity: More Than Just a Number
Obesity is commonly measured using the Body Mass Index (BMI), which is calculated by dividing weight in kilograms by height in meters squared. A BMI of 30 or higher is generally considered obese. While BMI has its limitations—it does not distinguish between fat and muscle mass, for instance—it remains a useful tool for population-level assessments.
Yet obesity is not just about weight; it is about excess adiposity, or fat accumulation, especially visceral fat that surrounds internal organs. This type of fat is metabolically active, meaning it releases hormones and inflammatory substances that disrupt normal body functions. Unlike subcutaneous fat, which lies under the skin and is relatively inert, visceral fat acts almost like a rogue organ, interfering with metabolism, immune function, and cardiovascular health.
This understanding has led scientists to see obesity not simply as a cosmetic condition but as a chronic disease in itself—one that triggers a cascade of other chronic illnesses.
The Biological Mechanisms Linking Obesity and Disease
The connection between obesity and chronic disease is rooted in biology. Excess fat tissue is not a passive storage site for calories; it is an active, dynamic tissue that communicates with the rest of the body through hormones, enzymes, and inflammatory molecules.
One of the key processes at work is chronic low-grade inflammation. Fat cells in obese individuals release pro-inflammatory cytokines, which keep the body in a constant state of mild inflammation. Over time, this inflammation damages tissues, impairs insulin signaling, stiffens blood vessels, and disrupts hormonal balance.
Another mechanism is insulin resistance. In obesity, the body’s cells become less responsive to insulin, the hormone that regulates blood sugar. As a result, glucose builds up in the bloodstream, leading eventually to type 2 diabetes.
Obesity also affects lipid metabolism, leading to elevated cholesterol and triglyceride levels. Combined with inflammation, these changes accelerate the buildup of arterial plaques, laying the foundation for cardiovascular disease.
Thus, obesity is not merely a background factor—it is an active driver of biological processes that culminate in chronic disease.
Obesity and Type 2 Diabetes: A Dangerous Partnership
Perhaps the most well-documented connection between obesity and chronic disease is its role in the development of type 2 diabetes. Nearly 90% of people with type 2 diabetes are overweight or obese.
The mechanism is straightforward but devastating: excess fat, particularly visceral fat, leads to insulin resistance. At first, the pancreas compensates by producing more insulin, but over time, it cannot keep up with demand. Blood sugar rises, and type 2 diabetes develops.
Diabetes itself is not only a disease but also a gateway to further complications. It damages blood vessels, nerves, kidneys, eyes, and even the brain. Stroke, heart disease, kidney failure, blindness, and dementia are all linked to diabetes, which in turn is closely tied to obesity. This chain of cause and effect highlights how obesity can be the starting point of a lifelong battle with chronic illness.
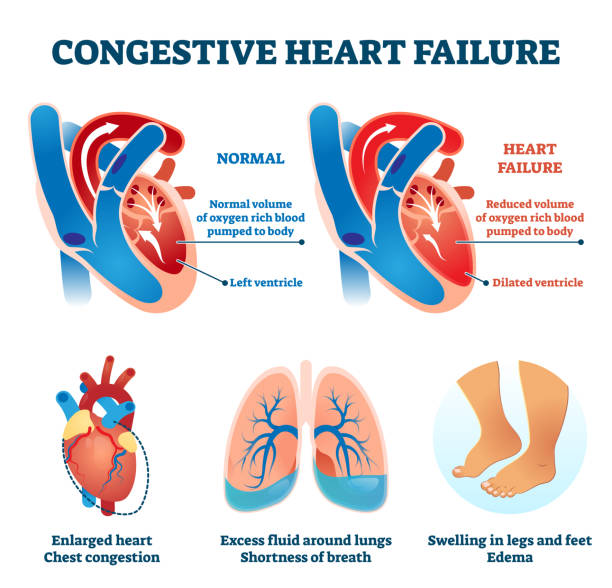
Obesity and Cardiovascular Disease: The Silent Killer
Cardiovascular disease (CVD) is the leading cause of death worldwide, and obesity significantly increases its risk. Excess fat contributes to high blood pressure, abnormal cholesterol levels, and atherosclerosis—the buildup of fatty deposits inside arteries.
Obesity-related hypertension is especially concerning. Extra fat tissue demands more oxygen and nutrients, forcing the heart to pump harder. This increased workload raises blood pressure, damages arteries, and strains the heart muscle. Over time, these changes can lead to heart attacks, strokes, and heart failure.
The danger lies in the fact that CVD often develops silently. Arteries can gradually narrow for years without symptoms, until one day a heart attack or stroke occurs. In this way, obesity plants the seeds of disease long before they fully bloom.
Obesity and Cancer: The Hidden Link
Cancer may not immediately come to mind when thinking about obesity, but mounting evidence shows that excess weight increases the risk of several cancers, including breast, colorectal, endometrial, pancreatic, and kidney cancer.
One reason is hormonal. Fat tissue produces estrogen, and elevated levels of estrogen are linked to cancers such as breast and endometrial cancer. Obesity also raises insulin and insulin-like growth factors, which can promote tumor growth.
Furthermore, the chronic inflammation associated with obesity creates an environment where cancerous cells are more likely to thrive. DNA damage, cell proliferation, and impaired immune surveillance—all influenced by obesity—combine to increase cancer risk.
Thus, obesity is not only about metabolic and cardiovascular disease but also about cancer risk, making it one of the most far-reaching health concerns of our time.
Obesity and Musculoskeletal Disorders: The Weight of the Body on Itself
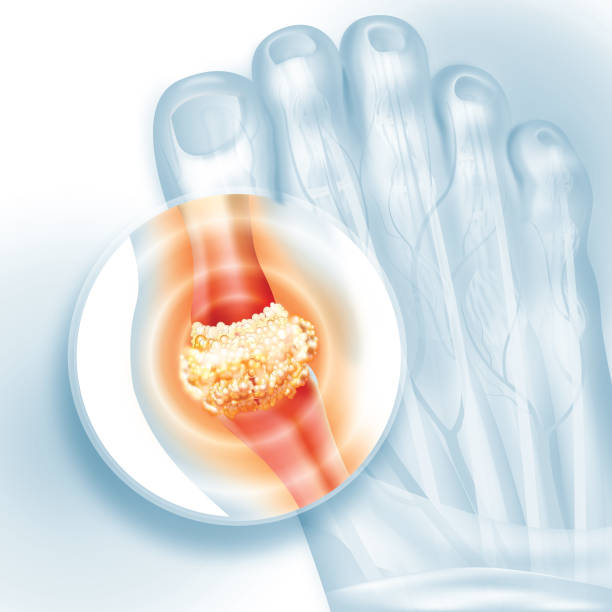
Carrying excess weight places tremendous mechanical stress on the bones, joints, and muscles. This leads to conditions such as osteoarthritis, particularly in weight-bearing joints like the knees and hips.
Obesity also contributes to back pain, reduced mobility, and a higher risk of injuries. For many people, this creates a vicious cycle: pain and reduced mobility discourage physical activity, which in turn leads to more weight gain and further deterioration of musculoskeletal health.
The emotional toll of limited mobility should not be underestimated. For many individuals, the inability to move freely diminishes independence, increases isolation, and contributes to mental health challenges such as depression.
Obesity and Respiratory Disorders: Breathing Under Pressure
Excess weight, especially around the abdomen, restricts the movement of the diaphragm and lungs, making breathing more difficult. This can lead to conditions such as sleep apnea, where breathing repeatedly stops and starts during sleep.
Sleep apnea is more than a nuisance; it disrupts rest, causes chronic fatigue, and increases the risk of high blood pressure, heart disease, and stroke. Obesity also worsens asthma symptoms and is associated with reduced lung function overall.
In this way, the very act of breathing—fundamental to life—becomes compromised by obesity.
The Psychological and Emotional Burden
While much focus is placed on the physical consequences of obesity, the psychological and emotional impact is equally profound. People living with obesity often face stigma, discrimination, and social isolation, which can fuel anxiety, depression, and low self-esteem.
This psychological burden can further complicate health outcomes. Depression may reduce motivation to exercise or eat healthily, while stress may drive emotional eating. The result is a cycle where physical and mental health feed into each other, deepening the challenges faced by those with obesity.
Obesity and Childhood: A Concerning Start
Childhood obesity has become one of the most pressing health concerns of the 21st century. Children who are obese are more likely to become obese adults, carrying with them the risks of diabetes, heart disease, and other chronic conditions at younger ages.
The implications extend beyond physical health. Childhood obesity affects self-esteem, social relationships, and academic performance. It also burdens families and healthcare systems, creating challenges that ripple through society.
Addressing obesity early in life is crucial, as habits formed in childhood often shape health trajectories for decades to come.
Societal and Environmental Drivers of Obesity
While it is tempting to view obesity as a matter of personal choice, the reality is far more complex. Modern environments are often “obesogenic,” meaning they promote weight gain through a combination of factors:
- Ubiquitous availability of calorie-dense, nutrient-poor foods
- Aggressive marketing of unhealthy products, especially to children
- Sedentary lifestyles driven by technology and urban design
- Stressful, fast-paced lives that limit time for cooking or exercise
These structural forces mean that obesity is not solely an individual problem but a societal one. Public health interventions, policies, and community-level changes are essential in creating environments that support healthier choices.
The Economic Cost of Obesity
Obesity is not only a personal health issue but also an economic burden. Healthcare systems spend billions of dollars treating obesity-related conditions, from diabetes medications to heart surgeries. Beyond direct medical costs, obesity leads to lost productivity, absenteeism, and disability, placing strain on economies worldwide.
The financial toll underscores the urgency of prevention and intervention. Investing in health promotion and obesity prevention is not only a moral imperative but also an economic necessity.
Strategies for Prevention and Management
Addressing obesity and its connection to chronic disease requires a multifaceted approach. Healthy eating, regular physical activity, adequate sleep, and stress management are cornerstones of prevention. But systemic changes are equally important: creating safe spaces for exercise, ensuring access to nutritious foods, regulating harmful marketing practices, and providing equitable healthcare.
Medical treatments, including medications and bariatric surgery, may be necessary for some individuals. These interventions, however, should be viewed not as shortcuts but as tools within a comprehensive strategy that includes lifestyle and behavioral support.
Above all, compassion and empathy must guide our approach. Obesity is not simply about willpower; it is about biology, environment, and society. Solutions must empower individuals without blaming or shaming them.
The Future of Obesity and Chronic Disease
The connection between obesity and chronic disease is clear and profound, but the future is not predetermined. Advances in genetics, microbiome research, and personalized medicine offer hope for more effective prevention and treatment strategies. Public health innovations, from urban planning to digital health tools, can also create environments that nurture health rather than undermine it.
Yet the most important shift may be cultural: a move toward valuing health as more than just the absence of disease or a number on a scale. Health must be seen as vitality, resilience, and well-being—a goal worth striving for across all levels of society.
Conclusion: A Call to Action
Obesity is not a superficial problem, nor is it simply a matter of personal choice. It is a powerful driver of chronic disease, shaping the health of individuals, families, and nations. Its roots run deep in biology, psychology, environment, and society. Its consequences ripple through every system of the body, from the heart to the brain, from the lungs to the joints.
The connection between obesity and chronic disease is one of the most urgent challenges of our time. But it is also a call to action—a reminder that health is both an individual journey and a collective responsibility. By understanding the science, addressing the social determinants, and fostering compassion, we can turn the tide on this epidemic and build a healthier future for generations to come.