Alzheimer’s disease is one of the greatest health challenges of our time. It robs people of their memories, independence, and identities, gradually dismantling the very essence of who they are. For families, watching a loved one drift away into confusion and disorientation is heartbreaking, and for societies, the burden is enormous. With populations aging worldwide, Alzheimer’s is expected to affect more than 150 million people by 2050, according to recent global projections.
Amid this rising crisis, scientists and doctors are racing to understand not just how to treat Alzheimer’s but how to prevent it. There is no single magic bullet yet—no pill, no injection that can completely stop the disease. But research has increasingly pointed toward something profoundly accessible, ancient, and powerful: exercise.
The idea that moving our bodies could shield our brains might sound almost too simple. Yet, decades of neuroscience, epidemiology, and physiology have converged to show that physical activity is one of the strongest defenses we have against Alzheimer’s disease. Exercise nourishes the brain, reshapes its structure, and fortifies it against decline. To understand why, we must journey into both the human body and mind, exploring how exercise acts like a medicine, a protector, and even a sculptor of memory.
What Exactly Is Alzheimer’s Disease?
To appreciate how exercise helps, we first need to understand what Alzheimer’s is and how it affects the brain. Alzheimer’s disease is a neurodegenerative disorder—meaning it involves the gradual breakdown of neurons, the cells that carry information in the brain. It is the most common cause of dementia, accounting for 60–70% of cases.
The hallmarks of Alzheimer’s are two abnormal protein deposits: amyloid-beta plaques and tau tangles. These toxic buildups disrupt communication between neurons and eventually kill them. Over time, entire brain regions shrink, particularly the hippocampus, which is crucial for memory and learning.
The symptoms unfold slowly. At first, it may be forgetting where the keys are or repeating a question. Later, it progresses to confusion about time and place, difficulty recognizing loved ones, and an inability to perform daily tasks. In advanced stages, Alzheimer’s strips away speech, mobility, and even the ability to swallow.
There is currently no cure. Medications can slow symptoms or improve quality of life temporarily, but they do not stop the underlying damage. This is why prevention is so vital—and where exercise enters the story.
Exercise as Medicine for the Brain
We often think of exercise as something for the body: for stronger muscles, a healthier heart, or weight loss. But modern neuroscience has revealed that exercise is equally medicine for the brain. Unlike some organs, the brain is not fixed or static—it is plastic, capable of changing and adapting throughout life. Physical activity is one of the most potent drivers of this neuroplasticity.
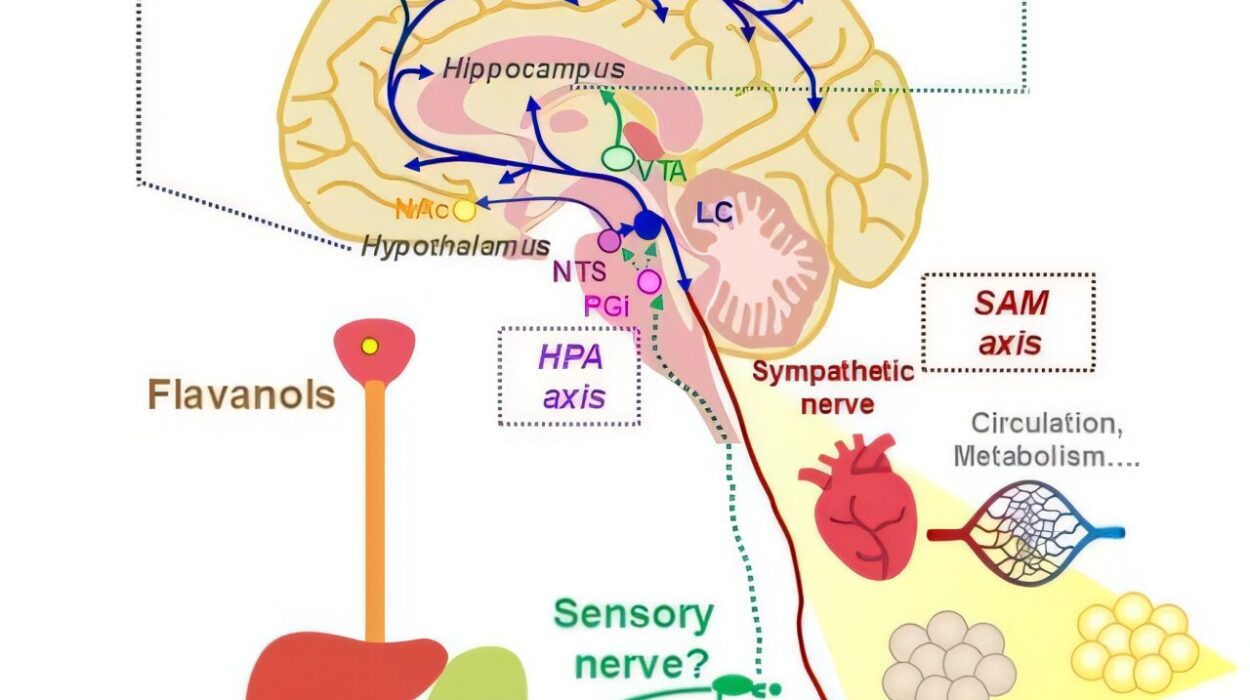
When we move—whether it’s running, cycling, swimming, or even brisk walking—our muscles contract and release proteins that travel through the bloodstream, influencing organs far beyond the skeletal system. Among the organs most profoundly affected is the brain.
Exercise increases blood flow, delivering more oxygen and nutrients to brain cells. It reduces inflammation, balances hormones, and stimulates the production of growth factors—molecules that support the survival and growth of neurons. Over time, exercise reshapes the very architecture of the brain, protecting it from degeneration and enhancing its ability to repair itself.
The Science of How Exercise Protects Against Alzheimer’s
Exercise Boosts Brain-Derived Neurotrophic Factor (BDNF)
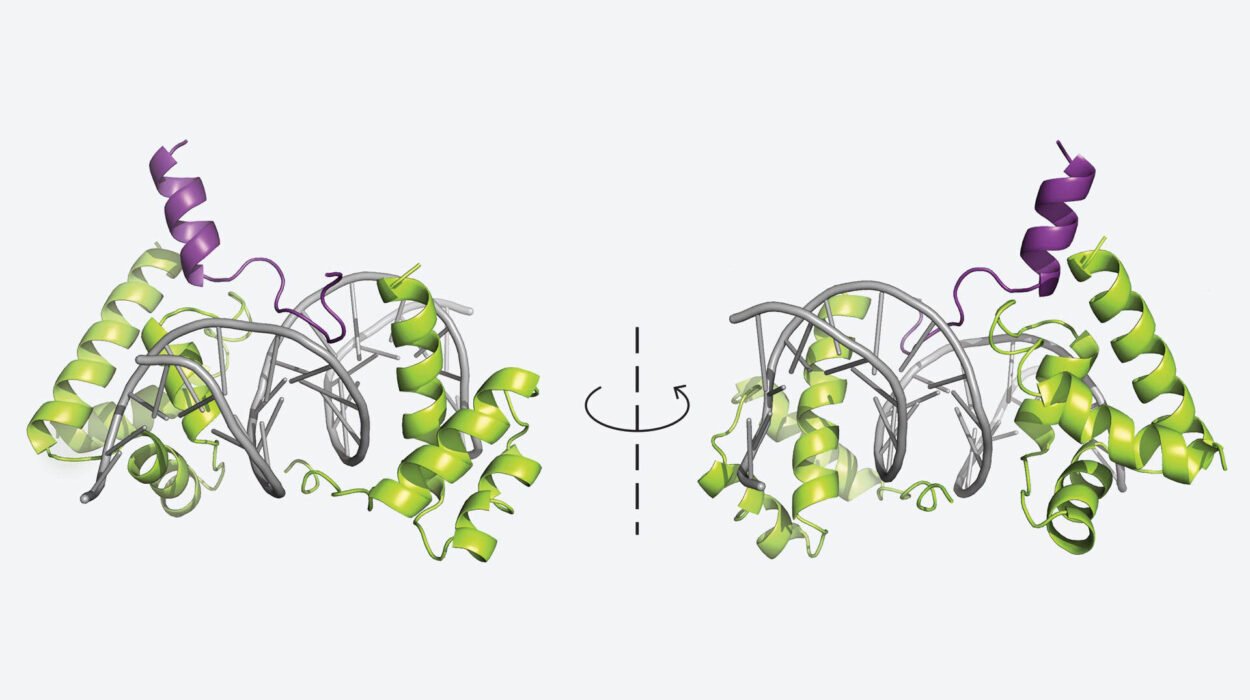
One of the most exciting discoveries in neuroscience is the role of brain-derived neurotrophic factor (BDNF). Often called “fertilizer for the brain,” BDNF promotes the survival of neurons, encourages the growth of new connections (synapses), and even stimulates the birth of new brain cells—a process called neurogenesis.
Alzheimer’s disease is marked by a dramatic decline in BDNF, which accelerates memory loss. Exercise, however, stimulates BDNF production. When you exercise, your muscles release proteins that cross into the brain and signal the production of BDNF, particularly in the hippocampus—the very region ravaged by Alzheimer’s.
This means that exercise not only protects existing brain cells but may also help the brain generate new ones, keeping memory circuits alive and functional.
Exercise Improves Blood Flow and Vascular Health
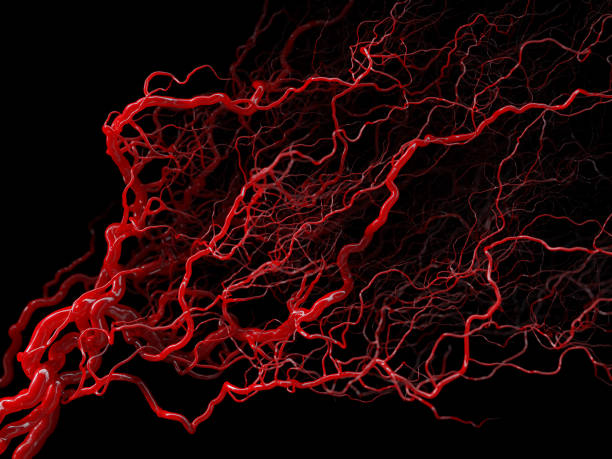
Another way exercise shields the brain is by supporting cardiovascular health. The brain is an energy-hungry organ, consuming about 20% of the body’s oxygen. For neurons to function properly, they rely on a constant supply of oxygen-rich blood.
Alzheimer’s often coincides with poor vascular health—stiff arteries, reduced blood flow, and microvascular damage that deprives neurons of nutrients. Exercise strengthens the heart, lowers blood pressure, improves circulation, and keeps blood vessels flexible. These effects reduce the risk of vascular dementia and also protect against the vascular contributions to Alzheimer’s disease.
By improving the delivery of oxygen and glucose, exercise ensures the brain’s energy demands are met, sustaining cognition and memory over time.
Exercise Reduces Inflammation
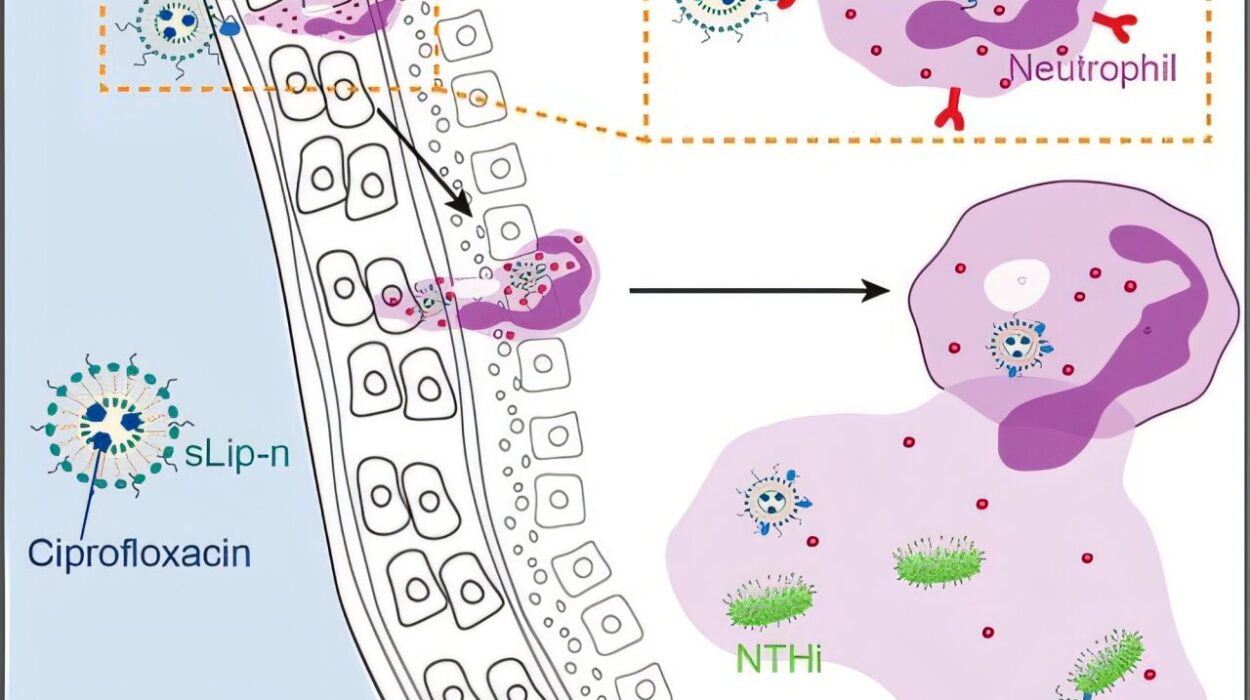
Chronic inflammation is a key driver of Alzheimer’s disease. When the immune system goes into overdrive, it releases molecules that damage neurons and accelerate the buildup of amyloid and tau.
Exercise acts as a powerful anti-inflammatory agent. It reduces systemic inflammation in the body, lowers levels of harmful cytokines, and helps regulate the immune system’s activity in the brain. Studies have shown that regular physical activity lowers the risk of chronic inflammatory diseases—and in the brain, this translates to fewer triggers for Alzheimer’s progression.
Exercise Clears Amyloid and Tau
Research in animal models has shown that exercise may directly influence the clearance of amyloid-beta plaques. Mice genetically engineered to develop Alzheimer’s show fewer plaques when given access to running wheels. Exercise stimulates the brain’s waste-disposal system, including the glymphatic system, which flushes out toxins during deep sleep.
Though more studies are needed in humans, early evidence suggests that physical activity helps regulate amyloid metabolism, slowing down its accumulation. This raises the possibility that exercise doesn’t just help the brain cope with Alzheimer’s—it may directly counteract its pathological roots.
Exercise Enhances Cognitive Reserve
One of the most fascinating findings in Alzheimer’s research is that some people with significant brain pathology—plaque and tangle buildup—never show symptoms of dementia. Scientists call this phenomenon cognitive reserve. It is the brain’s ability to compensate for damage by recruiting alternative pathways and networks.
Exercise is a powerful builder of cognitive reserve. By strengthening synaptic connections, stimulating neurogenesis, and enriching brain networks, physical activity equips the brain with greater resilience. Even if Alzheimer’s changes occur, a stronger brain may delay or blunt their impact on daily life.
Types of Exercise and Their Impact on the Brain
Not all exercise has the same effects on the brain, though most forms provide benefits. Researchers have studied different types of physical activity to see which might be most protective against Alzheimer’s.
Aerobic exercise—activities like running, brisk walking, cycling, and swimming—appears to be the most powerful in boosting BDNF, blood flow, and hippocampal volume.
Resistance training—lifting weights or using resistance bands—improves insulin sensitivity, reduces inflammation, and supports executive functions, which are often impaired in Alzheimer’s.
Mind-body exercises—such as yoga, tai chi, and qigong—reduce stress, improve balance, and enhance emotional regulation. Chronic stress is a risk factor for Alzheimer’s, and these practices lower cortisol levels, protecting the brain from stress-induced damage.
High-intensity interval training (HIIT)—short bursts of intense effort followed by rest—has shown promise in animal studies, with robust increases in BDNF. Early human trials also suggest HIIT may be particularly effective for cognitive health.
In reality, the best exercise is the one people enjoy and can sustain. Consistency is key. Even moderate activity, like daily walking, can significantly reduce Alzheimer’s risk.
Exercise Across the Lifespan: It’s Never Too Late
A common misconception is that exercise only helps if started young. While lifelong physical activity does provide the greatest protection, research shows it is never too late to benefit.
In one study, older adults with mild cognitive impairment who began a six-month program of brisk walking showed improvements in memory and executive function compared to sedentary peers. Another study found that individuals who started exercising in midlife reduced their Alzheimer’s risk by nearly 40%.
Even those already diagnosed with Alzheimer’s can benefit. Exercise in patients has been shown to improve mood, slow functional decline, and reduce agitation. While it may not reverse the disease, it improves quality of life and preserves independence for longer.
The Emotional Power of Movement
Science explains the biological mechanisms, but health is not only about molecules and neurons. Exercise also transforms how people feel. It lifts mood, reduces anxiety, and sparks a sense of vitality that is often missing in aging.
For individuals at risk of Alzheimer’s, exercise brings hope. It is an act of empowerment—a way to take control in the face of uncertainty. Each step, each breath, each heartbeat during physical activity becomes a declaration: I am fighting for my mind, for my memories, for my future.
For caregivers and families, encouraging loved ones to move can be a gift. Shared walks, dance sessions, or yoga classes are not just preventive medicine—they are moments of connection, joy, and love.
Barriers to Exercise and How to Overcome Them
Despite its proven benefits, many people struggle to exercise regularly. Barriers include lack of time, physical limitations, chronic illness, or simply not knowing where to start. For older adults, fear of injury or lack of motivation may also play a role.
Overcoming these barriers requires creativity and compassion. Exercise does not need to mean running marathons. Walking the dog, gardening, swimming at a gentle pace, or dancing in the living room all count. The key is regularity and enjoyment.
Community programs, supportive environments, and health policies can also play a role. Cities with safe parks, accessible gyms, and walking-friendly neighborhoods empower their citizens to stay active. Public health campaigns highlighting the brain benefits of exercise can further motivate people to move.
The Future of Research: Exercise as a Prescription
Doctors are increasingly recognizing exercise as a legitimate prescription for brain health. Clinical trials are now testing specific exercise regimens as treatments for mild cognitive impairment and early Alzheimer’s. Wearable devices are helping track activity, while imaging technologies measure changes in brain volume and connectivity.
The hope is that within the next decade, doctors will prescribe not just drugs but personalized exercise programs—tailored to genetic risk, age, and lifestyle—as powerful tools to prevent Alzheimer’s.
Conclusion: Moving Toward a Brighter Mind
Alzheimer’s disease may be one of the most daunting medical challenges of our era, but exercise shines as a beacon of hope. It strengthens the body, nourishes the brain, and empowers people to take charge of their cognitive future. By boosting growth factors, improving circulation, reducing inflammation, and building cognitive reserve, exercise strikes at the very vulnerabilities that make the brain prone to Alzheimer’s.
We cannot change our genes, but we can change how we live. Every walk in the park, every stretch on a yoga mat, every session at the gym is more than physical activity—it is an investment in memory, independence, and identity.
In the fight against Alzheimer’s, movement is not just medicine. It is resistance. It is resilience. It is the rhythm of life itself, protecting what makes us human—the ability to think, to remember, to love, and to be.