In a groundbreaking study published in Nature, scientists have uncovered a startling biological connection: common respiratory infections such as COVID-19 and influenza can awaken dormant breast cancer cells hidden in the lungs. These “sleeper” cancer cells—silent remnants of a previous disease—can be stirred into deadly action by the body’s immune response to respiratory viruses, potentially setting the stage for new metastatic tumors.
Led by researchers from the University of Colorado Anschutz Medical Campus, Montefiore Einstein Comprehensive Cancer Center (MECCC), and Utrecht University, the study draws a direct biological line between inflammation caused by respiratory infections and the resurgence of metastatic breast cancer. What was once speculation, bolstered by anecdotal evidence during the pandemic, has now found firm scientific footing through meticulous research using both animal models and large human datasets.
Cancer’s Lingering Shadow
For patients in remission, cancer can feel like a shadow that never fully disappears. Even after treatment, tiny colonies of cells—called disseminated cancer cells (DCCs)—can travel through the bloodstream and settle in distant organs like the lungs. Often, these rogue cells lie dormant for years, even decades, before reawakening. What triggers their return has remained one of the greatest mysteries in oncology.
Now, that mystery is beginning to unravel.
“Our findings indicate that individuals with a history of cancer may benefit from taking precautions against respiratory viruses,” said Dr. Julio Aguirre-Ghiso, director of MECCC’s Cancer Dormancy Institute and a senior leader of the study. “Even common infections may carry risks we hadn’t fully appreciated before.”
The implications are as profound as they are urgent. With respiratory viruses—especially COVID-19—firmly embedded in the landscape of everyday life, the need to understand their long-term impact on cancer survivors is no longer theoretical. It is a matter of life and death.
Awakening the Sleeping Enemy in the Lungs
The researchers began their investigation in the controlled environment of a lab. Using specially designed mouse models from Dr. Aguirre-Ghiso’s lab—models that simulate dormant breast cancer cells in the lungs—scientists exposed the mice to SARS-CoV-2 and influenza viruses.
The results were staggering.
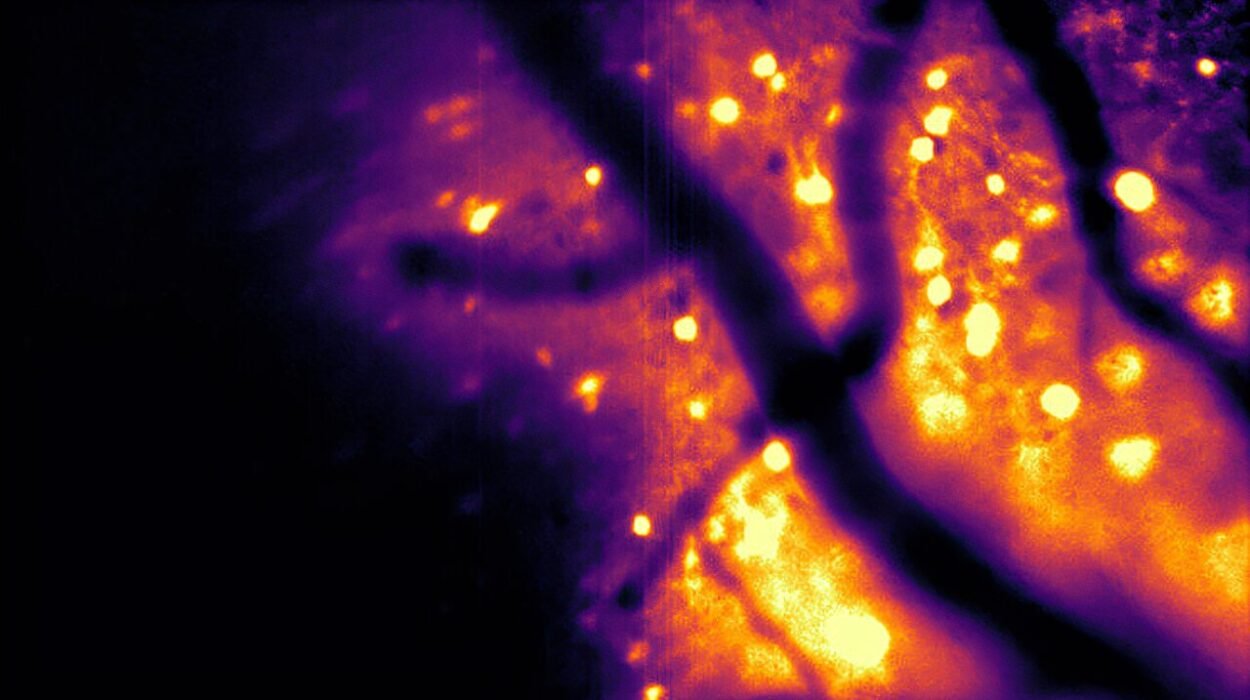
Within days of infection, the mice showed a massive reactivation of these dormant cells. Dormant colonies that had been stable for long periods suddenly expanded, leading to the formation of aggressive metastatic tumors in the lungs in just two weeks.
“Dormant cancer cells are like the embers left in an abandoned campfire,” said Dr. James DeGregori, senior author and deputy director of the University of Colorado Cancer Center. “Respiratory viruses are like a strong wind that reignites the flames.”
At the molecular level, this reawakening was traced to a protein called interleukin-6 (IL-6). This immune molecule is produced during inflammation and infection and is one of the key players in the body’s response to viruses. However, its presence also acts like a signal flare to sleeping cancer cells, encouraging them to grow once more.
IL-6: The Double-Edged Sword of Immunity
IL-6 is no stranger to immunologists. It’s a powerful cytokine—a messenger molecule that tells immune cells where to go and what to do. During a viral infection, IL-6 helps coordinate a strong defense. But in the context of dormant cancer cells, that very defense mechanism appears to become dangerous.
By releasing IL-6, the body inadvertently triggers changes in the environment around DCCs, creating conditions ripe for metastasis. This doesn’t just change the theoretical landscape of cancer biology—it opens the door for targeted intervention.
“The identification of IL-6 as a key mediator in arousing DCCs suggests that using IL-6 inhibitors or other targeted immunotherapies might prevent or lessen the resurgence of metastasis following viral infection,” explained Dr. Aguirre-Ghiso.
This offers hope. IL-6 inhibitors already exist and are used to treat inflammatory diseases like rheumatoid arthritis and cytokine storm in severe COVID-19 cases. With further research, these drugs could be repurposed as protective agents for cancer survivors during periods of viral infection.
Data From the Pandemic: A Natural Experiment
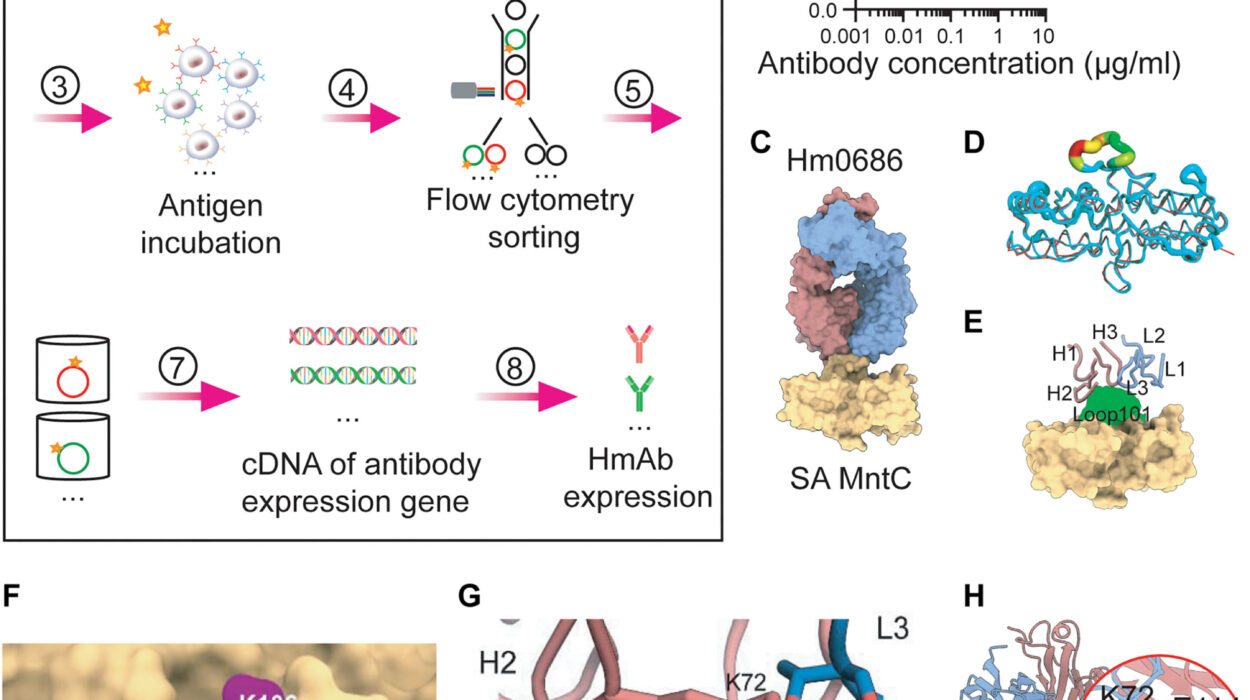
The real-world impact of these findings is underscored by two large population studies conducted alongside the lab work. Using the UK Biobank and the U.S. Flatiron Health database, the researchers investigated whether COVID-19 infections in cancer survivors correlated with worsened outcomes. The results echoed the animal studies in chilling detail.
In the UK Biobank study, scientists examined 487 cancer survivors who had contracted COVID-19 and compared them with over 4,300 matched cancer survivors who had not. Crucially, they excluded those who died directly from COVID-19. Even after this, they found that those who had tested positive for COVID-19 faced nearly double the risk of dying from cancer. The effect was most pronounced within the first year after infection—aligning with the timeline observed in the mouse models.
In the Flatiron Health study, researchers analyzed data from over 36,000 breast cancer patients treated in 280 cancer clinics across the U.S. Among these, 532 had contracted COVID-19. Over a follow-up period of approximately four years, patients who had experienced COVID-19 were nearly 50% more likely to develop new lung metastases than those who had not.
“These results are sobering,” said Dr. Roel Vermeulen of Utrecht University and Imperial College London, who co-led the population studies. “They suggest that respiratory viral infections may not just be short-term challenges for cancer survivors—they could have long-lasting consequences.”
A Warning, and a Path Forward
These findings come with a clear message: vigilance is warranted, but panic is not. For millions of cancer survivors worldwide, this study signals a new era in understanding the silent threats that may linger even after apparent recovery.
Vaccination against respiratory viruses—particularly COVID-19 and influenza—could become an essential part of survivorship care. Preventing these infections may be a simple, powerful tool in reducing the risk of metastatic recurrence. The study also points to the need for routine monitoring and potentially even preventive treatments for high-risk survivors during outbreaks.
“Our findings suggest that cancer survivors may be at increased risk of metastatic relapse after common respiratory viral infections,” Dr. Vermeulen emphasized. “By understanding the underlying mechanisms, we will work hard to develop interventions that can limit the risk.”
Already, researchers are expanding the study’s scope, investigating whether other cancers and metastatic sites are similarly affected by respiratory infections. They also plan to explore whether IL-6 inhibitors and related therapies could offer a shield to vulnerable patients.
“We’ve opened a door into a world we didn’t fully understand before,” said Dr. DeGregori. “Now we need to walk through it responsibly and with urgency.”
The Bigger Picture: The Intersection of Infection and Cancer
This study represents more than just a medical discovery—it’s a paradigm shift. For decades, cancer research and infectious disease research moved in parallel lanes. But the COVID-19 pandemic has blurred those boundaries. We now see that viral infections may not only be co-existing threats but may also directly influence the course of cancer.
This isn’t the first time infection and cancer have been linked. Human papillomavirus (HPV) causes cervical cancer, and Helicobacter pylori infection can lead to stomach cancer. But what this study reveals is more subtle and haunting: that a viral infection can awaken a past cancer, even when the tumor was long gone.
It redefines remission. It underscores the importance of inflammation as not merely a symptom but a potential driver of disease. It opens up new questions about how the immune system, long hailed as a warrior against cancer, can also be a reluctant accomplice under certain conditions.
A New Chapter in Survivorship
For the millions of people who have fought breast cancer and won, this study is a wake-up call. But it is also a source of hope. By illuminating the pathways by which infections reawaken dormant cancer cells, scientists are better equipped to develop strategies that interrupt that process. Science, after all, is not only about discovering dangers—it is about discovering solutions.
As we learn to live with viruses like COVID-19 as part of our daily landscape, it becomes more urgent than ever to understand their full impact. This research brings us closer to that understanding and offers a powerful reminder: even the smallest embers can reignite, but they can also be extinguished—if we know where to look.
More information: James DeGregori, Respiratory viral infections awaken metastatic breast cancer cells in lungs, Nature (2025). DOI: 10.1038/s41586-025-09332-0
Brooke P. Dresden et al, Inflammation during viral infection can rouse dormant cancer cells, Nature (2025). DOI: 10.1038/d41586-025-02137-1 , www.nature.com/articles/d41586-025-02137-1