Pulmonary fibrosis, often described as “lung scarring,” is one of the most devastating lung diseases known today. Though relatively uncommon, its toll is heavy: most patients die within five years of diagnosis, and current treatments are limited in effectiveness. For decades, researchers have tried to unravel the mysteries of this illness by focusing mainly on how the delicate lining of the lungs becomes damaged and why the body’s repair systems go awry. But now, a team of scientists at the University of Calgary has uncovered a surprising new player in this story: the very nerve cells that usually help us feel pain.
This groundbreaking study, led by Dr. Bryan Yipp from the Cumming School of Medicine and published in Immunity, reveals that pain-sensing neurons do far more than alert us to discomfort. In fact, they may act as guardians of the lungs, working quietly to control harmful inflammation that fuels pulmonary fibrosis. This discovery could open the door to treatments that use the body’s own nervous system to protect against this deadly disease.
A Silent Disease With a Heavy Toll
Pulmonary fibrosis is an illness where healthy lung tissue is gradually replaced by scar tissue. As the scarring spreads, the lungs stiffen, making it increasingly difficult for patients to breathe. The disease is relentless, robbing people of their ability to draw air into their lungs, limiting oxygen in the blood, and ultimately threatening life itself.
Every year in Canada alone, about 2,500 people die from lung scarring, and around 30,000 live with the disease. The human toll goes far beyond numbers, touching families, caregivers, and communities who watch loved ones struggle with something as basic as taking a breath. Despite its devastating impact, treatment options remain limited, often slowing but not stopping the progression of the disease.
This is why the Calgary team’s findings matter so deeply. By uncovering an unexpected role for nerve cells, they have added an entirely new dimension to how we think about—and possibly treat—pulmonary fibrosis.
Neurons, the Immune System, and the Lungs
Neurons are usually thought of as messengers of the brain and spinal cord, transmitting signals that allow us to move, think, and feel. But the nervous system extends its reach into every corner of the body—including the lungs. Here, pain-sensing nerve cells, called nociceptors, normally help detect irritants or harmful particles. They can trigger coughing, a protective reflex that clears the airways.
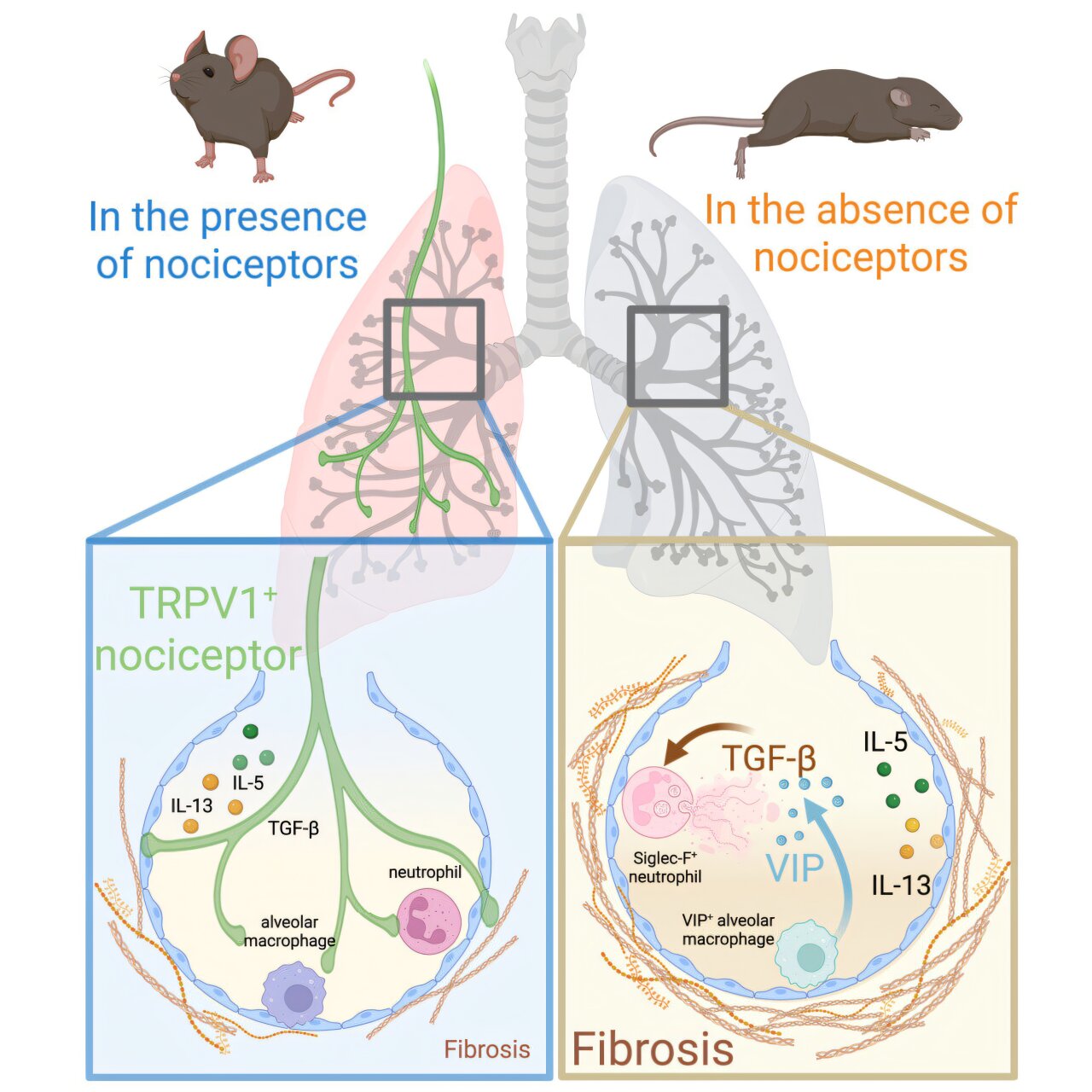
What the Calgary researchers found, however, is that these same nociceptor neurons also help regulate inflammation in the lungs. In experiments with mice, when these neurons were disrupted—either with drugs or by genetic techniques—the lungs lost a crucial line of defense. Harmful immune cells called neutrophils, normally kept under control, began to spiral into overactivity. This unleashed a wave of inflammation that made lung scarring significantly worse.
In other words, pain-sensing nerves do more than cause us to cough or feel discomfort—they actively protect lung tissue from the kind of inflammation that drives fibrosis.
The Role of a Surprising Molecule
As the scientists dug deeper, they uncovered an even more intriguing twist. Without the regulating presence of nociceptor neurons, immune cells in the lungs—called alveolar macrophages—began producing a neuropeptide named vasoactive intestinal peptide, or VIP. Normally, macrophages don’t generate this molecule, which is usually associated with nerve signaling. But under these unusual conditions, VIP production skyrocketed, and the result was damaging: inflammation worsened, and scarring advanced.
When the researchers blocked VIP or removed the gene responsible for producing it in macrophages, the harmful inflammation subsided and the lungs showed signs of improvement. But when VIP was artificially added back, the damage returned. This revealed a delicate interplay between neurons and immune cells, one that could be targeted for future therapies.
From Brain Therapies to Lung Protection
Perhaps the most exciting implication of this discovery is the possibility of using neurological therapies to treat lung disease. Devices that electrically stimulate nerves are already used to manage seizures, depression, and chronic pain. Dr. Yipp and his team suggest that the same kinds of therapies could be adapted to boost the protective role of nociceptor neurons in the lungs.
This is not a far-off fantasy but a plausible extension of existing treatments. If stimulating pain-detecting nerves can also calm harmful lung inflammation, we may be on the cusp of a revolutionary approach to managing pulmonary fibrosis—a disease long considered nearly untreatable.
As Dr. Carlos Hiroki, the study’s first author, explained, this discovery comes after years of exploring how nerve cells interact with lung disease. His work, part of his doctoral research, highlights how patience, curiosity, and persistence can yield insights with the power to change medicine.
A New Frontier in Lung Health
The University of Calgary’s findings mark a turning point in our understanding of pulmonary fibrosis. For the first time, the nervous system is being recognized not only as a messenger of pain but as an active regulator of lung health. By linking nociceptor neurons to the immune system, the study challenges old assumptions and invites bold new ideas for treatment.
The discovery also underscores a broader truth: the body is not a collection of separate systems working in isolation. Instead, it is an intricately connected network, where nerves, immune cells, and tissues are in constant conversation. In the case of pulmonary fibrosis, listening to that conversation could reveal life-saving strategies.
Looking Toward Hope
For those living with pulmonary fibrosis, every breath is precious, and every advance in science offers hope. The work of Dr. Yipp, Dr. Hiroki, and their colleagues does not provide a cure—not yet. But it offers something perhaps just as important: a new pathway forward.
In time, therapies inspired by this discovery could transform how doctors treat lung scarring, extending lives and easing suffering. Until then, the story of these pain-sensing neurons reminds us of the beauty and resilience of the human body. Even in its most fragile moments, it holds hidden defenses—waiting for science to discover and harness them.
Pulmonary fibrosis remains one of the most difficult challenges in medicine, but with discoveries like this, hope breathes a little easier.
More information: Carlos H. Hiroki et al, Nociceptor neurons suppress alveolar macrophage-induced Siglec-F+ neutrophil-mediated inflammation to protect against pulmonary fibrosis, Immunity (2025). DOI: 10.1016/j.immuni.2025.05.002