In the quiet shadows of the human mind, where mood swings can rise like thunderclouds or sink into the fog of despair, bipolar disorder continues to haunt millions. It’s a condition that does not simply alter moods—it warps the experience of reality itself. For those who live with it, and the people who love them, bipolar disorder is both a thief of peace and, at times, a harrowing intensifier of life.
Despite its widespread prevalence, the disorder remains deeply misunderstood—not only by the public, but by science itself. For decades, researchers have sought to decode what lies beneath the unpredictable emotional tides: the intense euphoria of mania, followed by the devastating collapse into depression. But while symptoms have been documented and treatments refined, the underlying biological causes remain only partially visible—like stars dimmed behind the clouds of human complexity.
Now, a new chapter is unfolding in our understanding of bipolar disorder. And it begins deep within the genome.
When DNA Holds the Answers Emotion Alone Cannot Provide
Every human being carries within them a book of genetic instructions—an encyclopedia of life, scribbled in four chemical letters. For years, scientists have suspected that bipolar disorder is written into this manual, its presence hinted at in twin studies and family trees where the illness reappears generation after generation.
Bipolar disorder is not just heritable—it is among the most heritable psychiatric disorders known, with estimates suggesting that over 70% of the risk is inherited. But pinning down the precise genetic culprits responsible has been like hunting ghosts in a library of three billion letters.
Genome-wide association studies, or GWAS, have offered glimpses into regions of the genome linked to higher risk. Yet these studies often identify broad regions, casting suspicion on hundreds—sometimes thousands—of genetic variants. They find “risk loci” rather than definitive causes, painting a hazy picture of correlation rather than causation.
What the field needed was clarity. And clarity requires resolution—down to the very building blocks of DNA.
Mapping the Maze: A New Approach to Genetic Discovery
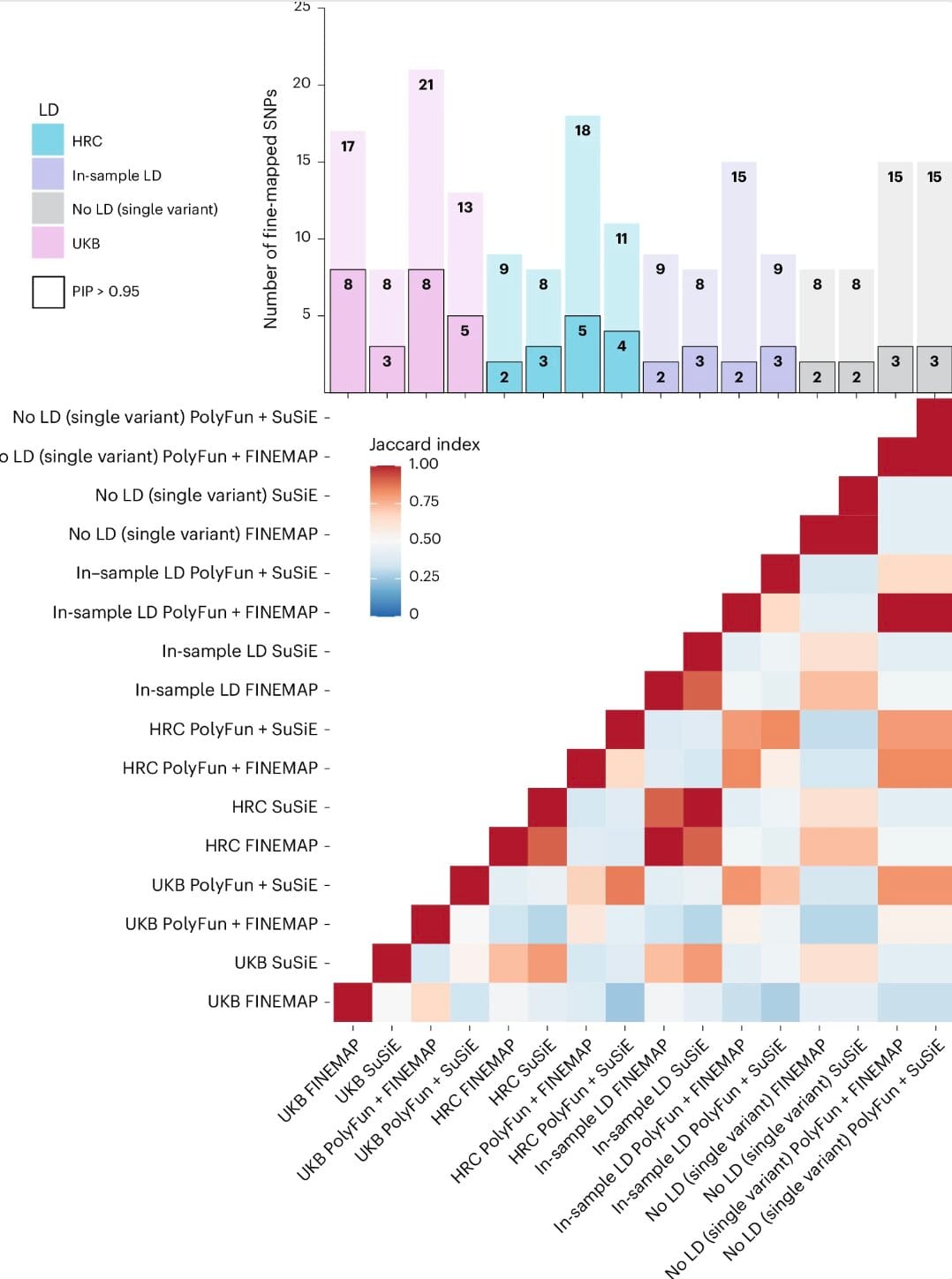
To bring light to this genetic darkness, researchers at the Icahn School of Medicine at Mount Sinai, along with colleagues from international institutions, launched a bold new study. Their work, recently published in Nature Neuroscience, employed a powerful methodology known as “fine-mapping”—a set of advanced statistical tools that aim to zero in on causal single nucleotide polymorphisms (SNPs). These are the tiny variations—changes in a single letter of DNA—that don’t just accompany bipolar disorder but may cause it.
Led by Maria Koromina, the team sifted through genetic data from more than 41,000 individuals with bipolar disorder and over 370,000 without, all of European ancestry. These numbers alone speak to the scale of the study, but it’s the precision of the analysis that marks a leap forward.
Unlike broader GWAS efforts, this study layered epigenomic data, examining how genes are expressed in specific brain cell types, and QTLs (quantitative trait loci), which help explain how genetic variants influence biological processes like gene splicing or DNA methylation.
This multi-dimensional approach allowed the researchers to move beyond identifying “where” the danger zones are in the genome—to identifying which mutations are likely guilty and which genes they disrupt.
Seventeen Signposts in the Genetic Fog
After years of piecing together this immense biological jigsaw, the fog has begun to lift. Koromina’s team identified 17 SNPs that stand out as likely causal contributors to bipolar disorder. These are not vague markers or genomic suspects. These are precise coordinates in the human genome that now carry the weight of scientific suspicion.
And more than that, these SNPs have been tied to specific genes—genes already known to play critical roles in how the brain develops, how neurons communicate, and how emotions are regulated.
Among the most compelling of these genes are:
- SCN2A: A key player in brain development and electrical signaling.
- TRANK1: Long associated with psychiatric risk but now more precisely linked to causality.
- CACNA1B: Involved in calcium signaling—crucial for neural function.
- THSD7A and FURIN: With roles in both neural and immune systems.
Each of these genes tells a story—about how our brains are wired, how they grow, and perhaps, how they sometimes fall apart.
The Brain-Gut Connection: A Genetic Clue in the Microbial Mirror
One of the more unexpected, even poetic, findings was that three of the genes most strongly linked to bipolar disorder also show high expression in gut cells. This isn’t coincidence—it’s part of a growing scientific recognition of the microbiota–gut–brain axis, a complex, bidirectional communication network between our digestive tract and our brain.
Could it be that some of the emotional turbulence seen in bipolar disorder begins in the belly? That the gut’s microbial residents, influenced by our genes, affect not just digestion but the delicate balance of neurotransmitters like serotonin and dopamine?
While the full story remains unwritten, the genetic connection hints at a deep biological unity between mind and body, between what we eat and how we feel.
Beyond Prediction: Toward Personalized Psychiatry
The practical implications of these findings stretch far beyond academia. By integrating fine-mapped variants into polygenic risk scores (PRS)—a statistical tool that estimates a person’s genetic likelihood of developing a condition—the researchers saw a significant boost in predictive accuracy. More importantly, this improvement held true across diverse ancestral populations, addressing a long-standing weakness in psychiatric genetics, which has often centered on European data at the expense of global applicability.
This means that future mental health assessments may involve not just conversations and checklists, but a peek into a person’s DNA. For some, it may mean earlier detection, targeted therapies, and a better understanding of their inner emotional landscape.
But the researchers are cautious. As Koromina herself noted, these are still probabilistic tools, not crystal balls. They guide, they don’t dictate. And they open the door not to genetic determinism, but to precision psychiatry—the art of matching treatment to biology, of healing tailored to the individual.
The Road Ahead: From Genes to Therapies
Science rarely offers instant answers. Discoveries, even groundbreaking ones, often raise as many questions as they resolve. The team behind this study knows that. Their next goal is not merely to catalogue SNPs, but to interrogate their function—to ask, gene by gene, mutation by mutation: What do you actually do?
This work will likely involve CRISPR gene editing, neuronal stem cells, and even brain organoids—miniature brain-like structures grown in the lab. These living models will allow researchers to observe, in real-time, how these mutations alter the way neurons connect, fire, or die.
It’s a journey from data to biology. From identification to intervention.
And ultimately, the dream is simple and profound: to transform suffering into understanding, confusion into clarity, despair into hope.
What It Means for the Human Experience
Bipolar disorder isn’t just a clinical diagnosis—it’s a deeply human experience. It lives in memoirs and hospital rooms, in whispered family histories and sleepless nights. It alters relationships, sabotages careers, fuels creativity, and inflicts agony. It is both an illness and, for some, a source of strange beauty.
For too long, those who suffer from bipolar disorder have lived in a world where their biology remained opaque. “Why me?” is a question too often met with silence. But now, bit by bit, science is replying.
The answer isn’t complete. It may never be. But we are beginning to see the outlines—of a disorder rooted in the circuitry of the brain, shaped by the ancient code of our DNA, and modulated by the environments we inhabit and the bacteria that call us home.
The Dawn of a New Understanding
This study is more than a scientific triumph—it’s a human one. It reflects the perseverance of researchers, the generosity of study participants, and the quiet revolution underway in psychiatry, where genomics and compassion walk hand in hand.
As the data continues to pour in, and as new tools sharpen our vision, we move closer to a world where bipolar disorder is not merely managed but truly understood—where treatments aren’t one-size-fits-all, but calibrated with exquisite precision to the genes and stories of each patient.
And in that world, perhaps, those who wrestle with bipolar disorder will find not just medicine, but meaning. Not just control, but connection. Not just stability, but a deeper peace—anchored in the knowledge that their suffering was never random, never meaningless, but the echo of complex biology we are finally beginning to understand.
Reference: Maria Koromina et al, Fine-mapping genomic loci refines bipolar disorder risk genes, Nature Neuroscience (2025). DOI: 10.1038/s41593-025-01998-z.