For millions around the world, waking up each morning doesn’t mean starting a new day—it means confronting a familiar wall of exhaustion, pain, and cognitive fog. These individuals live with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a condition so misunderstood that it is often dismissed, misdiagnosed, or completely overlooked.
Despite its devastating effects—rivaling or surpassing those of diseases like multiple sclerosis or lupus—ME/CFS has long remained in the shadows of medicine. Many sufferers are told that it’s all in their head. Some are prescribed antidepressants. Others are simply told to “try harder.” But the fatigue they feel is not the tiredness that rest can fix; it’s cellular, biological, and crushing. It is a body’s plea for help—a plea that science, until recently, has struggled to understand.
That is beginning to change.
Cracking the Code Through Connection
In a breakthrough study published in Nature Medicine, scientists have finally started to map the complex biological landscape of ME/CFS. Using a new artificial intelligence platform called BioMapAI, researchers have uncovered how this elusive disease disrupts the intimate connections between our gut microbiome, immune system, and metabolism—an intricate symphony that, when broken, leads to the chorus of pain, fatigue, and dysfunction seen in ME/CFS.
Led by Dr. Julia Oh, now a professor at Duke University, in collaboration with immunologist Dr. Derya Unutmaz of The Jackson Laboratory, and clinicians from the Bateman Horne Center, this research marks one of the most comprehensive biological analyses of ME/CFS ever conducted. The team examined 249 individuals—153 patients and 96 healthy controls—integrating vast layers of biological data, from gut bacteria to immune profiles, from blood chemistry to symptom diaries.
With remarkable precision—over 90% diagnostic accuracy—the study could distinguish between those living with ME/CFS and those without. For a disease that has historically lacked even the most basic biomarker, this represents a turning point.
The Human Cost of Being Ignored
In the United States alone, up to 3.3 million people may suffer from ME/CFS, though many remain undiagnosed. The economic burden is staggering—ranging from $18 to $51 billion annually in health care costs and lost productivity. But numbers fail to capture the emotional toll.
People with ME/CFS often lose careers, relationships, and dreams. Some become housebound for decades. Many navigate a maze of doctors, only to be told they are exaggerating or depressed. Parents have lost custody of children after refusing psychiatric care for what they know is a physical disease. Teenagers have been confined to wheelchairs and hospital rooms with no answers.
What this new research offers is more than scientific discovery—it offers validation. It tells patients that they are not imagining things. Their suffering is real, and now, finally, science is listening.
From Chaos to Clarity
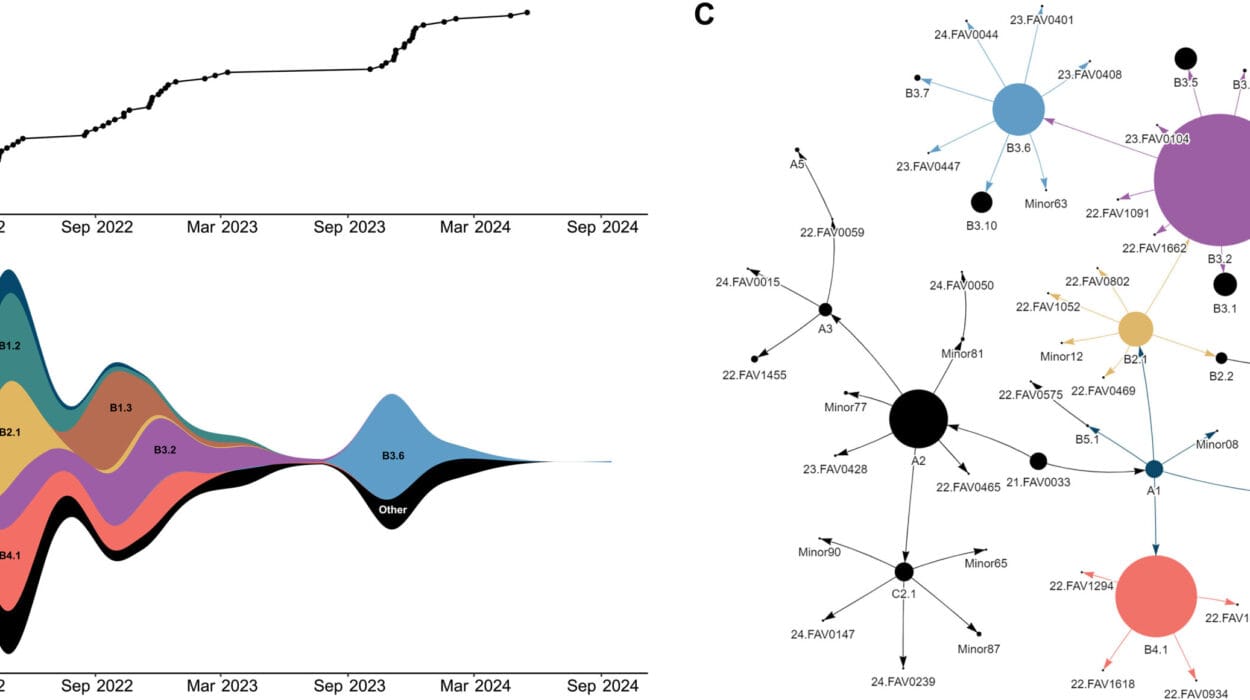
The genius of BioMapAI lies in its ability to decode biological complexity. ME/CFS isn’t one-size-fits-all. Some patients suffer more from pain, others from sleep dysfunction, dizziness, or emotional swings. The diversity of symptoms has long confounded researchers. What this AI model does is connect thousands of biological data points with 12 classes of patient-reported symptoms—mapping how microbiome imbalances, immune cell abnormalities, and metabolic disruptions converge to shape the unique experience of each patient.
Dr. Ruoyun Xiong, co-lead author, spent four years building this model. It digests enormous streams of data—gut metagenomics, plasma metabolomics, immune signatures, and clinical symptoms—and finds patterns that humans alone would miss. Most strikingly, it showed that immune cell data best predicted symptom severity, while microbiome profiles most strongly correlated with sleep, emotional health, and digestive issues.
Patients who had been sick for over a decade exhibited deeper, more entrenched biological disruptions. But those ill for fewer than four years showed less breakdown between systems, hinting at a potential window for earlier, more effective intervention.
Dr. Unutmaz explained the importance of this timeline: “Our data indicate these biological disruptions become more entrenched over time. That doesn’t mean longer-duration ME/CFS can’t be reversed, but it may be more challenging.”
Microbial Murmurs and Silent Messengers
One of the study’s most intriguing revelations came from the gut—the home of trillions of bacteria that influence everything from digestion to mood. In ME/CFS patients, the researchers found reduced levels of butyrate, a short-chain fatty acid produced by healthy gut microbes. Butyrate is known for its anti-inflammatory properties and its role in maintaining gut integrity. Its absence hints at a microbial ecosystem out of balance.
Alongside this deficit, researchers observed increased levels of tryptophan and benzoate—byproducts that can either calm or agitate the nervous system depending on their processing. Elevated levels suggest a gut-brain axis that’s misfiring, possibly contributing to the cognitive fog and emotional instability many ME/CFS patients report.
Even more compelling was the behavior of a special type of immune cell called MAIT cells, which are highly responsive to gut microbial health. These cells were hyperactive in patients, suggesting that chronic immune stimulation—possibly due to microbial dysbiosis—is driving inflammation throughout the body. In healthy individuals, these cells acted in harmony with gut bacteria. In ME/CFS patients, the connection was frayed.
“MAIT cells bridge gut health to broader immune functions,” Unutmaz said. “Their disruption alongside butyrate and tryptophan pathways, normally anti-inflammatory, suggests a profound imbalance.”
Drawing Parallels with Long COVID
As the world grapples with the long shadow of COVID-19, many researchers have noticed eerie parallels between ME/CFS and long COVID. Both conditions often follow viral infections. Both manifest with fatigue, brain fog, and a bewildering range of symptoms. And both seem to involve disruptions in the immune system and microbiome.
This makes the findings of the BioMapAI study doubly important. What we learn about ME/CFS could offer clues for understanding—and treating—long COVID. It could also help scientists understand why some viral infections never fully resolve in certain people, and how early immune-microbiome interactions might hold the key to resilience or relapse.
Toward Precision, Toward Hope
While BioMapAI is not a diagnostic tool ready for everyday clinics—at least not yet—it lays the groundwork for something revolutionary: personalized medicine for a disease long trapped in a medical fog.
That future could include tailored probiotics, anti-inflammatory therapies, or diet interventions guided by specific microbiome and metabolome profiles. It might include immune-modulating drugs that target the hyperactive cells identified in this study. Or it might involve therapies we haven’t even conceived yet, built on data from real people living with ME/CFS.
Dr. Julia Oh remains optimistic: “The microbiome and metabolome are dynamic,” she said. “That means we may be able to intervene—through diet, lifestyle, or targeted therapies—in ways that genomic data alone can’t offer.”
Importantly, the study’s findings held true across external datasets, reinforcing that these are not random observations but repeatable biological signatures. That consistency is what gives researchers confidence—and patients, perhaps, a reason to hope.
A Roadmap for the Future
The team plans to make their dataset and BioMapAI platform widely available. By doing so, they hope to enable researchers around the world to further investigate ME/CFS and similar conditions. The goal is not just to describe the disease, but to understand it deeply enough to outsmart it.
“We want to build a detailed map of how the immune system interacts with gut bacteria and the chemicals they produce,” Oh said. “By connecting these dots we can start to understand what’s driving the disease and pave the way for genuinely precise medicine.”
No one claims this is the end of the road. Much more work is needed to validate the findings, refine the models, and translate insights into treatments. But for the first time in decades, the road ahead is illuminated—however faintly—with the light of understanding.
Listening to the Body’s Whisper
Science moves slowly. But when it listens—truly listens—it can begin to hear the subtle whispers of the body, the hidden conversations between cells and microbes, between inflammation and exhaustion. ME/CFS has long been a disease defined by silence—by the silence of ignored patients, of unanswered questions, of treatments that didn’t work.
This research breaks that silence. It affirms what patients have known all along: their illness is real, their suffering is measurable, and the story written inside their bodies is one that science can finally begin to read.
In the quiet, in the fatigue, in the loneliness—there is a signal. And we are finally learning how to hear it.
Reference: AI-driven multi-omics modeling of myalgic encephalomyelitis/chronic fatigue syndrome, Nature Medicine (2025). DOI: 10.1038/s41591-025-03788-3